Published online Jun 27, 2023. doi: 10.4240/wjgs.v15.i6.1216
Peer-review started: December 22, 2022
First decision: January 3, 2023
Revised: January 14, 2023
Accepted: April 19, 2023
Article in press: April 19, 2023
Published online: June 27, 2023
Processing time: 175 Days and 11.6 Hours
Bronchogenic cysts are congenital lesions requiring radical resection because of malignant potential. However, a method for the optimal resection of these cysts has not been completely elucidated.
Herein, we presented three patients with bronchogenic cysts that were located adjacent to the gastric wall and resected laparoscopically. The cysts were detected incidentally with no symptoms and the preoperative diagnosis was challenging to obtain via radiological examinations. Based on laparoscopic findings, the cyst was attached firmly to the gastric wall and the boundary between the gastric and cyst walls was difficult to identify. Consequently, resection of cysts alone caused cystic wall injury in Patient 1. Meanwhile, the cyst was resected completely along with a part of the gastric wall in Patient 2. Histopathological examination revealed the final diagnosis of bronchogenic cyst and revealed that the cyst wall shared the muscular layer with the gastric wall in Patients 1 and 2. In Patient 3, the cyst was located adjacent to the gastric wall but histopathologically originated from diaphragm rather than stomach. All the patients were free from recurrence.
The findings of this study state that a safe and complete resection of bronchogenic cysts required the adherent gastric muscular layer or full-thickness dissection, if bronchogenic cysts are suspected via pre- and/or intraoperative findings.
Core Tip: Bronchogenic cysts are rare congenital lesions, which require radical resection as they might turn malignant. We presented three patients with bronchogenic cysts that were located adjacent to the gastric wall and resected laparoscopically. Based on the findings, we hypothesized that it was advisable to proceed to the stomach wall to remove the cyst completely, preventing rupture of it. This was supported by histopathological assessment which revealed bronchogenic cysts of the stomach generally shared the muscular layer with the gastric wall. Resection of cysts with the adherent gastric muscular layer or full-thickness dissection should be considered for a safe and complete resection.
- Citation: Terayama M, Kumagai K, Kawachi H, Makuuchi R, Hayami M, Ida S, Ohashi M, Sano T, Nunobe S. Optimal resection of gastric bronchogenic cysts based on anatomical continuity with adherent gastric muscular layer: A case report. World J Gastrointest Surg 2023; 15(6): 1216-1223
- URL: https://www.wjgnet.com/1948-9366/full/v15/i6/1216.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i6.1216
Bronchogenic cysts are congenital lesions that develop during embryogenesis, with a prevalence rate of 1 in 68000[1]. Most of them are found in the mediastinum because they arise from the primitive tracheobronchial trees. Therefore, bronchogenic cysts located adjacent to the stomach are extremely rare[2,3].
Surgical resection is considered a radical treatment for bronchogenic cysts because they have a malignant potential[4-6]. However, the sole resection of the cyst has a possible risk of rupture because the boundary between the gastric and cyst walls is sometimes difficult to recognize grossly[7,8]. Meanwhile, the partial or conventional gastrectomy seems to be an excessive treatment in terms of the balance between postoperative decreased quality of life and the low incidence of malignant trans
We have recently encountered three patients with bronchogenic cysts. During the surgical treatment, it was challenging to identify the proper dissection line between the gastric and cyst walls. Based on these experiences, we hypothesized that it is advisable to proceed to the stomach wall to remove the cyst completely, preventing rupture of it. To elucidate our hypothesis, we aimed to histopathologically assess the three patients with bronchogenic cyst that were located adjacent to the gastric wall, mainly focusing on the continuity of the gastric muscular layers. This case report and pathological assessments will really help surgeons remove gastric bronchial cysts with minimum invasion, safely and completely because gastric bronchial cyst is extremely rare, and few surgeons can effectively tackle the disease.
All three patients had no chief complaints.
Patient 1: A 37-year-old female patient was referred to our hospital due to a mass that was incidentally detected on perioperative examination for palate tonsillectomy.
Patient 2: A 47-year-old male patient underwent physical assessment, and a cystic mass with a diameter of 3 cm was detected in the abdomen for which he had been undergoing follow-up examinations from 4 years at a local hospital. However, the mass size increased to 5 cm and referred to our hospital thereafter.
Patient 3: A 37-year-old male patient was referred to our hospital due to a mass that was incidentally detected.
Patient 1: The patient had a previous history of immunoglobulin A nephropathy.
Patients 2 and 3: The patients had no previous history of illness.
All three patients had no personal and family history.
All three patients had neither symptoms nor abnormal physical findings.
Patient 1: Routine blood examination results and the levels of tumor markers such as carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 19-9 were normal.
Patient 2: Routine blood examination results were normal, but there was an increase in the serum CA 19-9 levels of the patient.
Patient 3: The routine laboratory tests results and serum levels of tumor markers, such as CEA and CA 19-9, were normal.
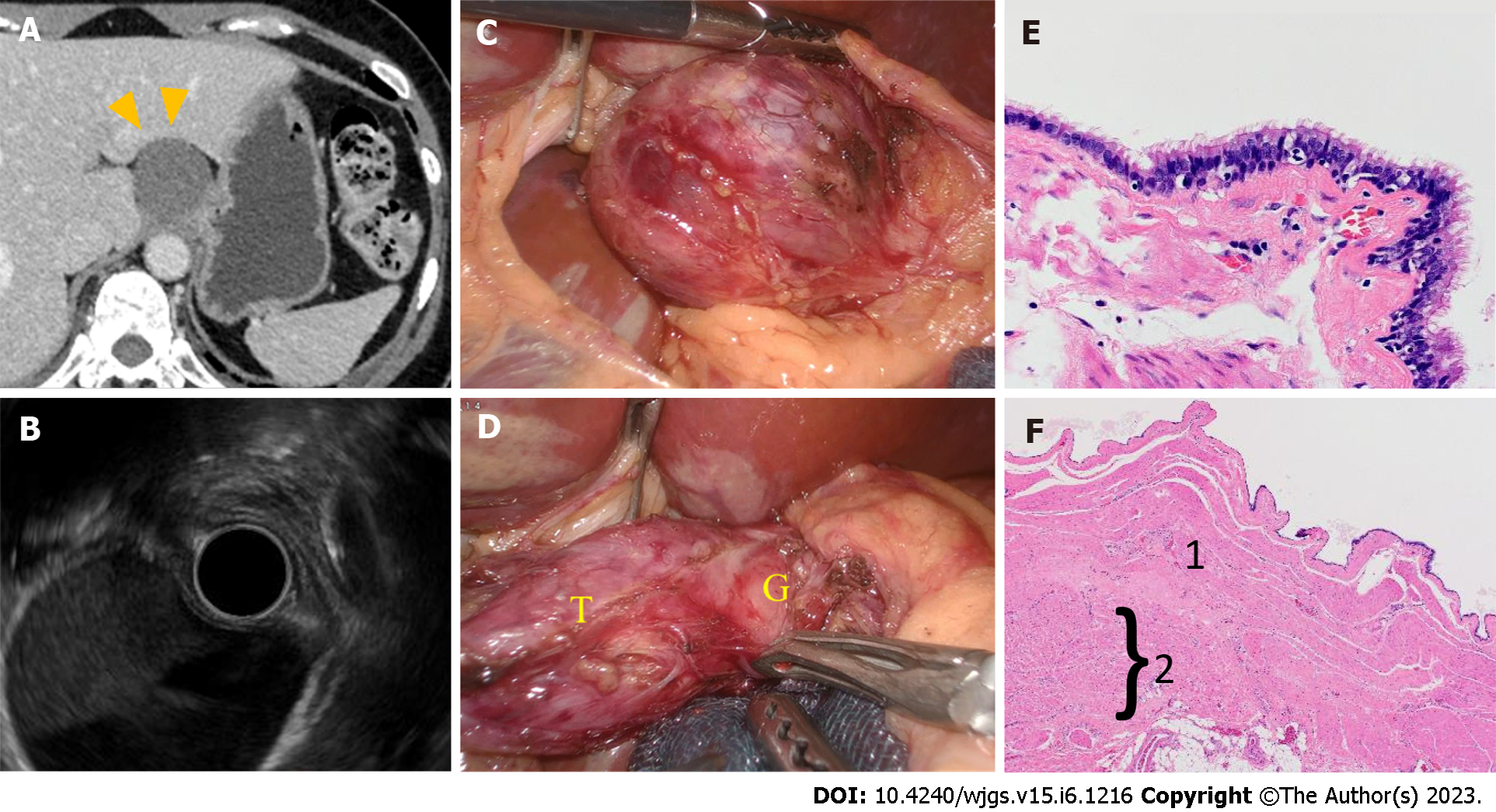
Patient 1: Computed tomography (CT) scan revealed a cystic mass with a diameter of 3 cm. There was no contrast enhancement, and the mass was located adjacent to the gastric cardia with regular outlines (Figure 1A). No calcification or septation was observed. Upper endoscopic examination showed no communication between the lesion and gastric lumen.
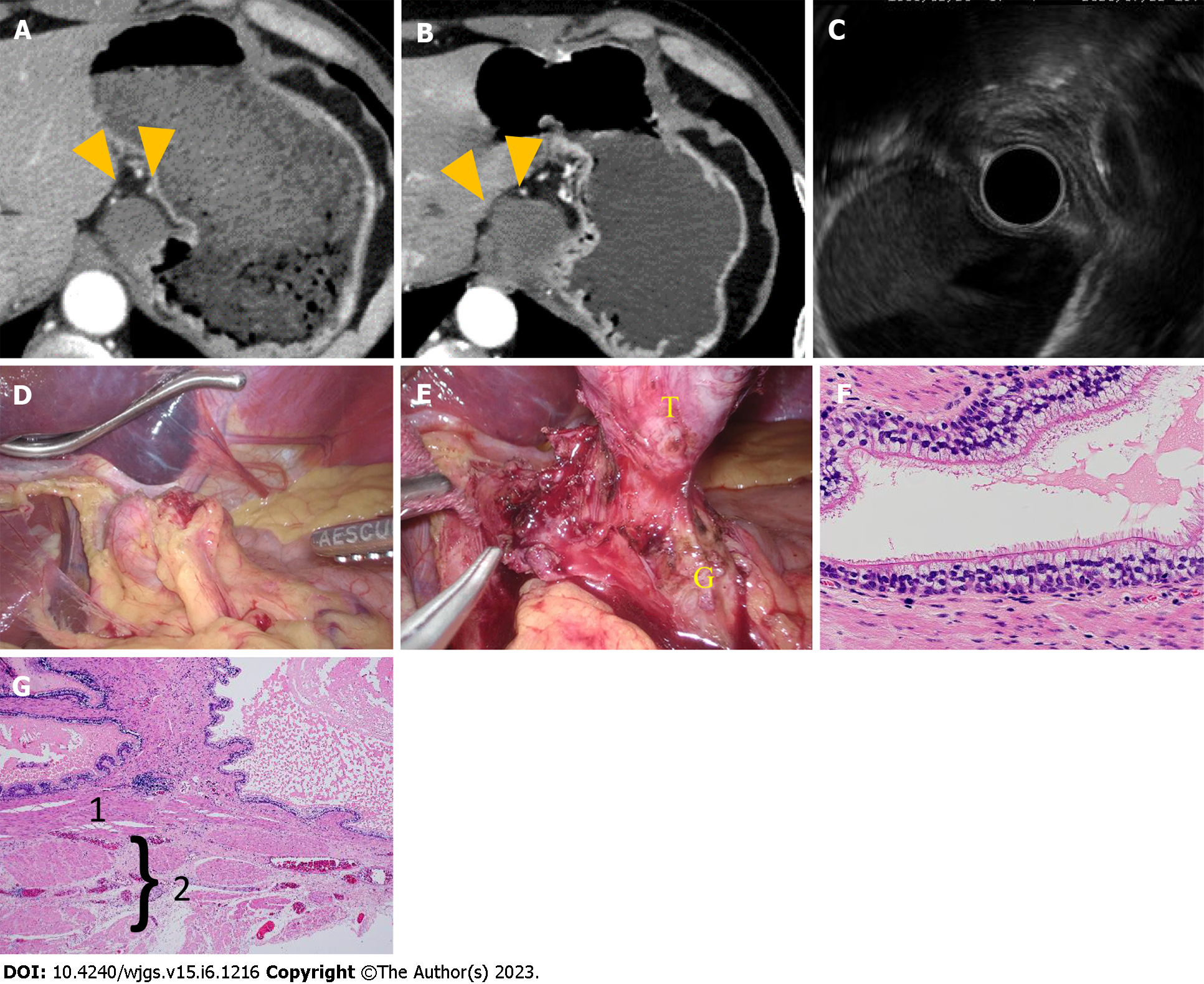
Patient 2: CT scan revealed a homogeneous low-density lesion with a diameter of 5 cm, and the mass was located adjacent to the cardia of the stomach (Figure 2A and B). Upper endoscopic examination showed no malignant findings in the stomach.
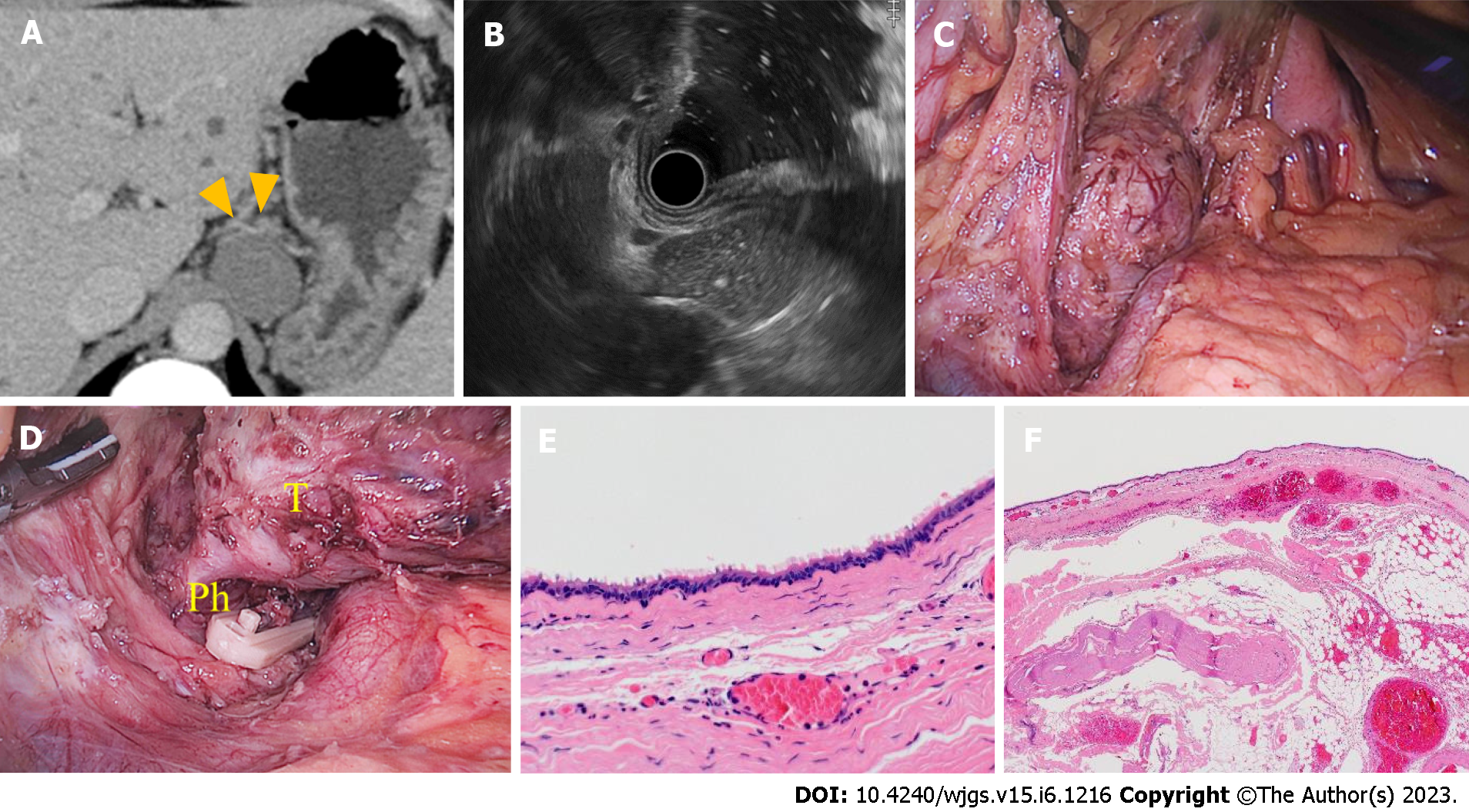
Patient 3: CT scan revealed a cystic mass with a diameter of 35 mm. The lesion was located adjacent to the posterior wall of the proximal stomach (Figure 3A). Magnetic resonance imaging showed a smooth and quasi-circular lesion with a high intensity on T2-weighted images and iso-intensity on T1-weighted images.
Endoscopic ultrasonography (EUS) detected an extramural cystic mass in the cardia (Figure 1B). However, there was no continuity with the gastric wall. Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) was not performed. The preoperative differential diagnoses were gastric duplication, foregut cyst, and bronchogenic cyst.
EUS revealed an extramural mass in the cardia (Figure 2C). Pseudostratified ciliated columnar epithelium and seromucous glands were observed on EUS-FNA. Thus, gastric bronchogenic cyst was suspected.
EUS showed a hyperechoic cystic mass (Figure 3B), which might be connected to the gastric wall. However, its continuity could not be detected. A yellow-brownish liquid was aspirated via subsequent needle biopsy.
Histopathologically, the cystic wall was lined with the ciliated columnar epithelia and mucous glandular cells without cytological atypia and was surrounded by smooth muscle fibers (Figure 1E). A diagnosis of bronchogenic cyst was made. The smooth muscle fibers of the cyst wall were continuous with the gastric muscular layer (Figure 1F). Based on these findings, the bronchogenic cyst arose from the gastric wall.
As in Patient 1, histopathological examination showed the typical findings of bronchogenic cyst, which include the presence of smooth muscle fibers, focal mucous glands, and ciliated columnar epithelia (Figure 2F). The cyst shared the muscular layer with the stomach, which indicated that the smooth muscle of the bronchogenic cyst was continuous with that of the gastric wall (Figure 2G).
A smooth cystic mass was identified on laparoscopic exploration of the gastric cardia (Figure 1C). A part of the cyst adhered firmly to the gastric wall and might have shared the muscular layer with the stomach (Figure 1D). Hence, it was difficult to detach from the gastric wall, and there was a bright yellow fluid discharge from the cyst during resection. Thus, the gastric muscular layer was incised, and the tumor was extracted. Thereafter, the gastric wall was sutured and reinforced by hand-sewing. Subsequently, intraoperative endoscopy was performed to validate gastric integrity.
Laparoscopy was performed, and the cyst was found in the lesser gastric curvature (Figure 2D). The lesser omentum was opened, and the tissue surrounding the lesion was resected. The feeding artery was found around the lesion and was transected using a vessel sealing system. The cyst wall was firmly connected to a part of the gastric wall (Figure 2E). Therefore, the muscular layer of the cyst seemed to be continuous with the gastric wall. The muscle between the cyst and gastric wall was divided. The tumor was completely excised along with a part of the gastric muscle layer. After extracting the specimen, the gastric wall was reapproximated, and the suture line was secured via intraoperative endoscopy.
Laparoscopy was performed, and the cyst was found in the lesser gastric curvature (Figure 3C). The lesser omentum was opened, and the tissue surrounding the lesion was resected. The feeding artery was found around the lesion and was transected using a vessel sealing system. The cyst wall was firmly connected to a part of the gastric wall (Figure 3D). Therefore, the muscular layer of the cyst seemed to be continuous with the gastric wall. The muscle between the cyst and gastric wall was divided. The tumor was completely excised along with a part of the gastric muscle layer. After extracting the specimen, the gastric wall was reapproximated, and the suture line was secured via intraoperative endoscopy.
The postoperative course was uneventful, and the patient was discharged on postoperative day 7. No recurrence was observed within the follow-up period of postoperative 9 mo.
The postoperative course was satisfactory, and no recurrence was observed within the follow-up period of postoperative 6 mo.
The postoperative course was uneventful, and no recurrence was observed within the follow-up period of postoperative 3 mo.
Bronchogenic cysts of the stomach are extremely rare[9]. Their histogenesis comprises abnormal buds of the tracheobronchial tree that are pinched off and migrate into the abdomen. Surgical resection is recommended as these cysts can be malignant. However, the current knowledge on the methods used for the optimal resection of bronchogenic cysts is limited due to the small number of cases. Herein, we report three patients with bronchogenic cysts that were located adjacent to the stomach and resected laparoscopically. Based on our surgical experiences and detailed histopathological examination results, knowledge on the pathological features of bronchogenic cyst is essential in facilitating a safe, complete, and less invasive resection.
Bronchogenic cysts should be considered when a cystic mass is found in the stomach, especially near the cardia and esophagogastric junction. Embryologically, they arise in the mesogastrium. A typical differential diagnosis of gastric cysts are gastric duplication cysts; however, they are usually located along the greater gastric curvature and endoscopically presented with ulcer formations or overlying dimple at the top of the protruding mass[10]. Therefore, these anatomical differences might be beneficial in diagnosing bronchogenic cysts. Meanwhile, a preoperative definitive diagnosis is still challenging via radiological examinations. CT scan could detect a solitary, low density, homogeneous uniocular mass, and magnetic resonance imaging revealed iso-intensity on T1-weighted images and high intensity on T2-weighted images[11,12]. However, these radiological findings are not specific to bronchogenic cysts. EUS can be performed to evaluate anatomical relationship and echoic characteristics, and subsequent FNA cytology can be useful[13]. No studies have discussed the diagnostic rate of bronchogenic cysts, and several reports have shown the feasibility of EUS-FNA for establishing a preoperative histological diagnosis of gastric bronchogenic cysts, as in Patient 2[13,14]. Some reports have shown that the diagnostic yield of cytology is limited because of the low number of cells that disperse in the cystic fluid[15], as in Patient 3. Thus, further research is required to evaluate the usefulness of EUS-FNA. However, to date, it is the only tool that can be used to obtain a preoperative diagnosis of bronchogenic cysts.
Surgical resection is recommended for radical treatment if bronchogenic cysts of the stomach are suspected due to the risk of malignant transformation. The carcinoma arising from the epithelial cells of bronchogenic cyst was reported[16]. Also, the patient with bronchogenic cyst of the stomach involved with gastric adenocarcinoma was reported[17]. Therefore, the risk of recurrence was high with incomplete resection, and complete resection was required[18,19]. Previous report showed that patients who underwent complete resection showed no recurrence[20]. The laparoscopic approach may be less invasive[21]. However, no optimal strategies for the complete resection of bronchogenic cysts of the stomach have been established. Previous reports showed that incomplete resection of bronchogenic cysts could lead to local recurrence or dissemination[4]. In the cases in which bronchogenic cysts are firmly attached to and invading the surrounding organs, combined resection is required to completely excise the lesions. As the lesions are commonly found in the lesser curvature of the stomach near the gastroesophageal junction or gastric cardia[1], partial or conventional gastrectomy is occasionally unavoidable[8,22]. However, most lesions had no communication with the gastric lumen, as in our case. Gastrectomy might be extensive with consideration of the facts that the incidence of malignant transformation is low and the procedure is associated with a decreased quality of life.
However, resection of cysts alone is associated with a risk of rupture because bronchogenic cysts have thin walls with regular borders[1]. Knowledge on pathological features is essential for the complete and less invasive resection of cysts because radiological examinations could not detect the positional associations between the cysts and surrounding organs. In previous cases of gastric bronchogenic cysts, the lesion was continuous with the stomach wall or was surrounded with the smooth muscle, which is continuous with the gastric muscular layer[23]. In Patients 1 and 2, the cysts also shared their muscular layer with that of the gastric wall histopathologically. However, the cyst had no communication with the muscular layer of the gastric wall, and it originated from the retroperitoneum rather than the stomach in Patient 3. In Patient 1, based on the preoperative radiological findings, the cyst was located outside the gastric wall, and resection of cysts alone was performed, which caused cystic wall injury. By contrast, in Patient 2, the cyst was successfully resected along with a part of the gastric wall. Based on these findings, combined resection of cysts with a part of the gastric wall or full-thickness dissection is required to facilitate a safe and complete resection in cases wherein the cyst shared the muscular layer with the stomach. This notion was confirmed by our pathological findings. To the best of our knowledge, this is the first report that discussed the optimal resection of bronchogenic cysts of the stomach based on its histopathological feature. Our patients were free from recurrence, and this type of resection was less invasive than conventional gastrectomy.
In conclusion, bronchogenic cyst of the stomach shares the muscular layer with the gastric wall. Resection of cysts with the adherent gastric muscular layer or full-thickness dissection should be considered for a safe and complete resection, if bronchogenic cysts are suspected via pre- and/or intraoperative findings.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gálvez Salazar P, Ecuador; Yao J, China S-Editor: Liu JH L-Editor: A P-Editor: Wu RR
| 1. | Tu C, Zhu J, Shao C, Mao W, Zhou X, Lin Q, Li Z, Zhang J, Zhou Q, Chen W. Gastric bronchogenic cysts: A case report and literature review. Exp Ther Med. 2016;11:1265-1270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 2. | Aktoğu S, Yuncu G, Halilçolar H, Ermete S, Buduneli T. Bronchogenic cysts: clinicopathological presentation and treatment. Eur Respir J. 1996;9:2017-2021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 102] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Seddik H, Adioui T, Rouibaa F, El Hamdi FZ, Aourarh A, Mahi M, Benkirane A, Zentar A. Gastric bronchogenic cyst presenting as a submucosal mass: a case report. J Med Case Rep. 2012;6:262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Rice DC, Putnam JB Jr. Recurrent bronchogenic cyst causing recurrent laryngeal nerve palsy. Eur J Cardiothorac Surg. 2002;21:561-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Hasegawa T, Murayama F, Endo S, Sohara Y. Recurrent bronchogenic cyst 15 years after incomplete excision. Interact Cardiovasc Thorac Surg. 2003;2:685-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Sullivan SM, Okada S, Kudo M, Ebihara Y. A retroperitoneal bronchogenic cyst with malignant change. Pathol Int. 1999;49:338-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 75] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Ubukata H, Satani T, Motohashi G, Konishi S, Goto Y, Watanabe Y, Nakada I, Tabuchi T. Intra-abdominal bronchogenic cyst with gastric attachment: report of a case. Surg Today. 2011;41:1095-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Kurokawa T, Yamamoto M, Ueda T, Enomoto T, Inoue K, Uchida A, Kikuchi K, Ohkohchi N. Gastric bronchogenic cyst histologically diagnosed after laparoscopic excision: report of a case. Int Surg. 2013;98:455-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Hedayati N, Cai DX, McHenry CR. Subdiaphragmatic bronchogenic cyst masquerading as an "adrenal incidentaloma". J Gastrointest Surg. 2003;7:802-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Wakabayashi H, Okano K, Yamamoto N, Suzuki Y, Inoue H, Kadota K, Haba R. Laparoscopically resected foregut duplication cyst (bronchogenic) of the stomach. Dig Dis Sci. 2007;52:1767-1770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Murakami R, Machida M, Kobayashi Y, Ogura J, Ichikawa T, Kumazaki T. Retroperitoneal bronchogenic cyst: CT and MR imaging. Abdom Imaging. 2000;25:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Vos CG, Hartemink KJ, Golding RP, Oosterhuis JW, Paul MA. Bronchogenic cysts in adults: frequently mistaken for a solid mass on computed tomography. Wien Klin Wochenschr. 2011;123:179-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Sato M, Irisawa A, Bhutani MS, Schnadig V, Takagi T, Shibukawa G, Wakatsuki T, Imamura H, Takahashi Y, Sato A, Hikichi T, Obara K, Hashimoto Y, Watanabe K, Ohira H. Gastric bronchogenic cyst diagnosed by endosonographically guided fine needle aspiration biopsy. J Clin Ultrasound. 2008;36:237-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Sun L, Lu L, Fu W, Li W, Liu T. Gastric bronchogenic cyst presenting as a gastrointestinal stromal tumor. Int J Clin Exp Pathol. 2015;8:13606-13612. [PubMed] |
| 15. | Cassiani J, Crinò SF, Manfrin E, Rivelli M, Gabbrielli A, Guglielmi A, Pedrazzani C. Endoscopic Ultrasound Through-the-Needle Biopsy for the Diagnosis of an Abdominal Bronchogenic Cyst. Clin Endosc. 2021;54:767-770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Endo C, Imai T, Nakagawa H, Ebina A, Kaimori M. Bronchioloalveolar carcinoma arising in a bronchogenic cyst. Ann Thorac Surg. 2000;69:933-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 60] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Shibahara H, Arai T, Yokoi S, Hayakawa S. Bronchogenic cyst of the stomach involved with gastric adenocarcinoma. Clin J Gastroenterol. 2009;2:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Read CA, Moront M, Carangelo R, Holt RW, Richardson M. Recurrent bronchogenic cyst. An argument for complete surgical excision. Arch Surg. 1991;126:1306-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 45] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Gharagozloo F, Dausmann MJ, McReynolds SD, Sanderson DR, Helmers RA. Recurrent bronchogenic pseudocyst 24 years after incomplete excision. Report of a case. Chest. 1995;108:880-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Yang X, Guo K. Bronchogenic cyst of stomach: two cases report and review of the English literature. Wien Klin Wochenschr. 2013;125:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Izumi H, Yoshii H, Abe R, Mukai M, Nomura E, Ito H, Sugiyama T, Tajiri T, Makuuchi H. Successful laparoscopic resection for gastric duplication cyst: a case report. J Med Case Rep. 2019;13:240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Chhaidar A, Ammar H, Abdessayed N, Azzaza M, Gupta R, Abdennaceur N, Bdioui A, Mokni M, Ali AB. Large bronchogenic cyst of stomach: A case report. Int J Surg Case Rep. 2017;34:126-129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Sun B, Wang AK, Chen H, Qian BL, Yi XK, Jiang Y, Li Q, Fu WG, Li J. Bronchogenic cyst of the stomach: A case report and literature review. Exp Ther Med. 2020;20:166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |