Published online Jun 27, 2023. doi: 10.4240/wjgs.v15.i6.1191
Peer-review started: January 20, 2023
First decision: February 14, 2023
Revised: February 17, 2023
Accepted: April 19, 2023
Article in press: April 19, 2023
Published online: June 27, 2023
Processing time: 145 Days and 13.7 Hours
The management of gallbladder perforation (GBP) with fistulous communication (Neimeier type I) is controversial.
To recommend management options for GBP with fistulous communication.
A systematic review of studies describing the management of Neimeier type I GBP was performed according to the PRISMA guidelines. The search strategy was conducted in Scopus, Web of Science, MEDLINE, and EMBASE (May 2022). Data extraction was obtained for patient characteristics, type of intervention, days of hospitalization (DoH), complications, and site of fistulous communication.
A total of 54 patients (61% female) from case reports, series, and cohorts were included. The most frequent fistulous communication occurred in the abdominal wall. Patients from case reports/series had a similar proportion of complications between open cholecystectomy (OC) and laparoscopic cholecystectomy (LC) (28.6 vs 12.5; P = 0.569). Mortality was higher in OC (14.3 vs 0.0; P = 0.467) but this proportion was given by only one patient. DoH were higher in OC (mean 26.3 d vs 6.6 d). There was no clear association between higher rates of complications of a given intervention in cohorts, and no mortality was observed.
Surgeons must evaluate the advantages and disadvantages of the therapeutic options. OC and LC are adequate options for the surgical management of GBP, with no significant differences.
Core Tip: Gallbladder perforations are rare. Management guidelines are non-specific. Although a clear benefit of laparoscopic cholecystectomy over open cholecystectomy is lacking, with the increase in laparoscopic training and availability, this approach may demonstrate superiority in time.
- Citation: Quiroga-Garza A, Alvarez-Villalobos NA, Muñoz-Leija MA, Garcia-Campa M, Angeles-Mar HJ, Jacobo-Baca G, Elizondo-Omana RE, Guzman-Lopez S. Gallbladder perforation with fistulous communication. World J Gastrointest Surg 2023; 15(6): 1191-1201
- URL: https://www.wjgnet.com/1948-9366/full/v15/i6/1191.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i6.1191
Gallbladder disease is a common pathology, frequently aggravated by gallstones, with a risk of complications. Such complications include the rare spontaneous (non-traumatic) gallbladder perforation (GBP), with an incidence ranging from 0.8% to 15.0% and a mortality of 12% to 16%[1-3]. It is caused by an obstruction of the cystic duct, which results in bile stasis with bacterial proliferation, distension, increased pressure, and vascular and lymphatic collapse and thereby leads to ischemia, necrosis, and finally perforation[3,4]. The most common site of perforation is the fundus, as it has the lowest vascular supply[5].
Acute cholecystitis may be classified into different grades of severity using the Tokyo guidelines or the Parkland classification[6,7]. However, GBP itself can be classified into three types according to Neimeier: Chronic perforation with fistulous communication (type I); subacute perforation with a surrounding abscess contained by adhesions (type II); and acute perforation and spillage to the cavity with generalized biliary peritonitis (type III)[8]. Due to a historically erroneous cite, authors frequently switch types I and III, a reason why it is important to specify the characteristics of the perforation[1-3,8-12].
Management protocols are well established in acute cholecystitis, but GBP management remains controversial. Preoperative diagnosis is difficult, usually only identified in half the cases[13]. Abdominal computed tomography (CT) provides the most sensitive and specific imaging tool allowing the evaluation of surrounding structures[1-3,14]. A recent systematic review of localized GBP established that open cholecystectomy (OC) has a lower incidence of requiring added procedures and a lower rate of postoperative complications[13]; however, recent cohorts support laparoscopic management[10,12,15]. Recommendations need to be reviewed as more current studies are added to the available literature. Fistulous communication has not been studied in detail and may vary depending on the organ/cavity of communication[16-19]. This systematic review aims to gather and revise the available evidence regarding chronic GBP with fistulous communication, focusing on management, specifically the type of surgical intervention, timing, and complications.
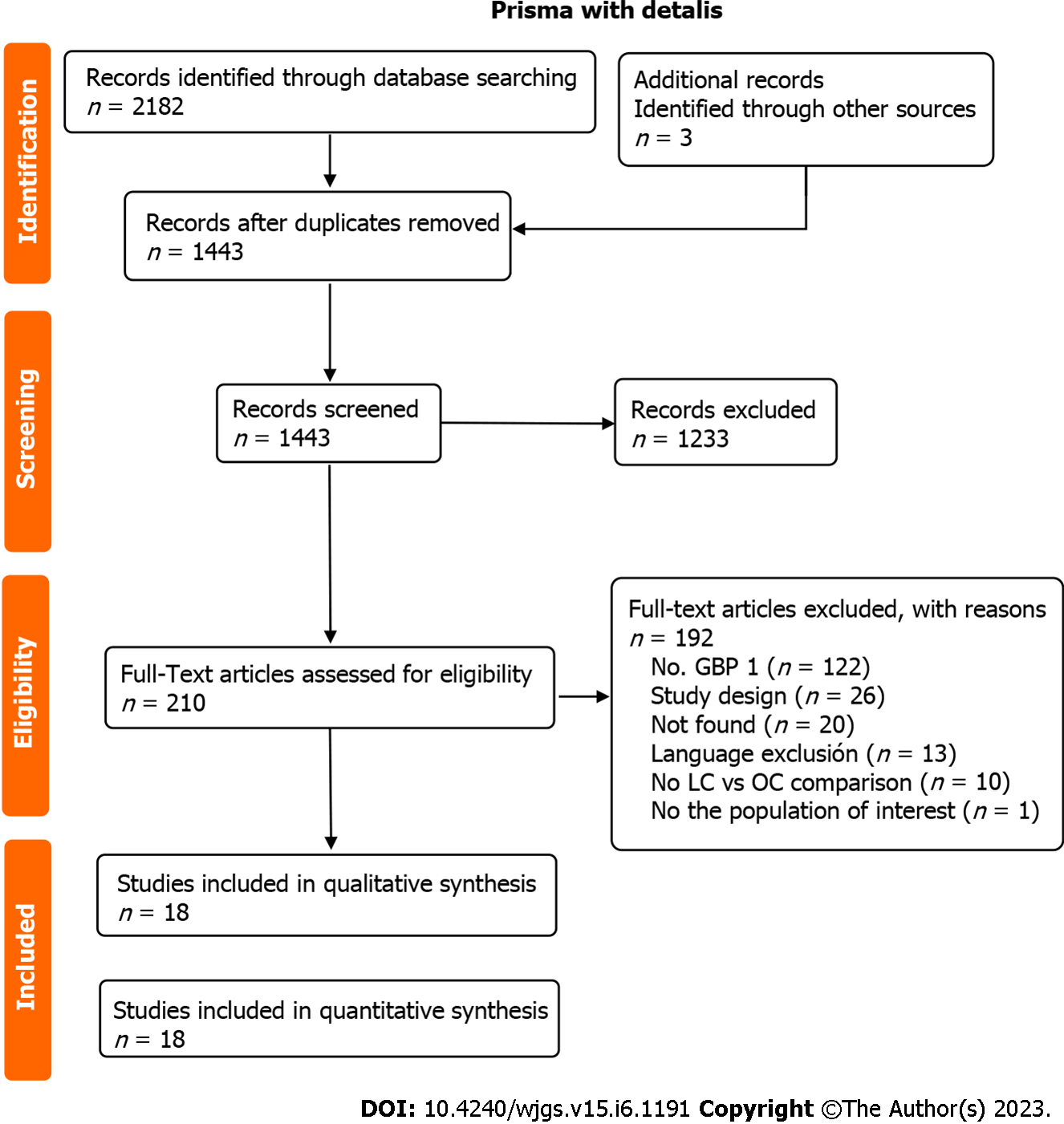
This study adhered to the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) statement[20]. It was successfully registered in the International Prospective Register of Systematic Reviews (PROSPERO, NIHR) under the ID: CRD42021275733. It was also reviewed and approved by the University’s Ethics and Research Committees with the registration number RV21-0019.
Studies meeting the following criteria were included in this review: (1) Randomized controlled trials (RCTs), quasi-RCTs, and observational studies (cohorts, case studies, and case series) that compared/reported OC and/or laparoscopic cholecystectomy (LC) for Neimeier type I GBP in adult patients (> 18 years old). The intervention must have been OC or LC and patients could have received another intervention either before or after the interventions of interest; (2) Studies that reported mean DoH (set as primary outcome), complications related to the surgical intervention, need of another intervention after OC/LC (the interventions did not resolve the GBP), mortality, fistulation organ, and need of intensive care unit (ICU) admission and (3) Studies reported in English or Spanish. Studies in which GBP Neimeier type I diagnosis was unclear were excluded. No restrictions were applied in terms of study setting or time frame.
An experienced librarian designed and conducted the search strategy in the following databases in May 2022: Scopus, Web of Science, MEDLINE, and EMBASE. An additional search was performed on Google Scholar. Reference lists from studies selected by the authors were added to identify any potential studies that may have been missed. This included clinical trial registries, and contacting experts in the field to identify any unpublished or in-progress eligible studies.
EndNote X8 was used to upload results and process de-duplication. The resulting studies were uploaded to Distiller Systematic Review (DSR) software to continue with title/abstract and full-text screening.
A two-phase study selection was performed (title/abstract and full-text screening). In each, two reviewers worked independently and in duplicate to assess the eligibility of the studies. Kappa statistic was used to calculate chance-adjusted inter-rater agreement[21]. A pilot test was performed before each screening phase, using a random sample of studies from the search strategy results to standardize the reviewers’ criteria. In case of disagreements, these were discussed to adjust criteria, if necessary. The pilot tests were repeated until reaching a Kappa index of > 0.70. The title and abstract were screened during the first phase, and reviewers selected the eligible articles based on the established inclusion criteria. Studies with discordant decisions were passed to the full-text phase to achieve a highly sensitive selection. Eligibility was then assessed through a full-text screening. In the second phase, any disagreements between the reviewers were resolved by consensus and if it was not achieved, a third reviewer arbitrated the evaluation. The number of included and excluded articles, as well as the reasons for the exclusion were documented.
Data from eligible articles were collected using a web-based data extraction form by two independent reviewers working in duplicate. The information obtained included: The type of study, author information, follow-up, year of publication, baseline characteristics of patients, type of intervention, DoH, days from diagnosis to intervention, complications, mortality, ICU admission, site of perforation, and fistulous communication. Disagreements were resolved by consensus, with the final decision made by a third reviewer in case that an agreement was not reached.
Missing or unclear data considered important for the outcomes were sought out. The corresponding author was contacted via e-mail with specific questions regarding their study. In case of non-response in a lapse of 10 d, a second email was sent. If no response was obtained, other authors were contacted. If contact failed, the data or study was excluded.
Two reviewers working independently and in duplicate evaluated the risk of bias from the studies using the Cochrane’s ROBINS-I tool for the quasi-RCTs and observational studies[22], and the tool for assessing the methodological quality of case reports/series proposed by Murad et al[23] for case reports/series. Any disagreement during this process was resolved by consensus, with the final decision made by a third reviewer in case that an agreement was not achieved.
The studies included are described in a table detailing study design and setting, sample size, target population characteristics, description of the intervention, study groups, type of outcomes, and the level of risk of bias.
SPSS version 25[24] and RevMan5[25] were used for statistical analyses. Variables are summarized and presented as the mean with standard deviation for the primary outcome. Dichotomous outcomes are presented as the number of events and proportions. Categorical variables were analyzed using the Chi-squared test, and Student’s t-test for independent groups for continuous numerical variables. If two or more studies were homogeneous enough, a cumulative meta-analysis was performed. A random-effects model was used with χ2 test and I2 statistic to assess heterogeneity between studies. The χ2 cut-off value of P < 0.10 and an I2 value > 50% were considered indicative of considerable heterogeneity. For all statistical analyses, a P value of < 0.05 was considered statistically significant. If this was not achieved, clinical outcomes are summarized narratively.
There was a sustainable level of agreement between reviewers in the title and abstract screening phase (k = 0.72) and full-text phase (k = 0.86). A total of 1443 studies were identified and screened, with 210 included for full-text screening. After both screening phases, 18 studies were included for the qualitative and quantitative synthesis of fifteen case reports/series and two cohort studies (Figure 1). Across all studies, no conflict of interest was observed. Most studies were published in 2016 or later (n = 47 patients vs 8 from studies published in 2015 or before), with 26 of the 55 total patients managed by LC (Table 1).
| Year | Patients with type I GBP | Men | Women | Lap Chol | Open Chol | Conservative treatment | ||||
| n | Qx pre | Qx post | n | Qx pre | Qx post | |||||
| ≤ 2005 | 2 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 |
| 2006-2010 | 3 | 1 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 1 |
| 2011-2015 | 3 | 0 | 3 | 1 | 0 | 0 | 1 | 0 | 0 | 1 |
| 2016-2020 | 25 | 11 | 14 | 19 | 0 | 0 | 5 | 0 | 1 | 1 |
| ≥ 2021 | 22 | 5 | 17 | 5 | 4 | 0 | 17 | 4 | 0 | 0 |
A total of 20 patients were included from case reports/series, with a mean age of 66.6 ± 17.6, of which 65% were female (Table 2). Nine patients denied comorbidities. The most common comorbidity was diabetes mellitus followed by cardiovascular diseases (Supplementary Table 1)[26-41]. Preoperative diagnosis was identified as a cholecystic fistula in 16 patients (4 not reported). The most utilized diagnostic imaging tool was abdominal ultrasound (US) and CT. The most common site of GBP was the fundus (n = 5) with communication to the abdominal wall (n = 11). Eight patients were treated by LC, but three were converted to OC, making it the most common (n = 12) approach. Four patients were managed conservatively, while three required added endoscopic retrograde cholangiopancreatography (ERCP). One patient with a pleural fistula required a chest tube. Patients treated conservatively had a shorter evolution time of symptoms to their admission to the emergency room (ER) with (141.5 d; range, 13-270), compared to those treated by OC (265 d; range, 10-730) and LC (174.2 d; range, 2-730). Patients undergoing OC had a shorter range of 7-18 d from their ER admission to the operating room (OR) compared to those undergoing LC with a range of 16-34 d. No patient was admitted to the ICU. OC had longer mean DoH than LC (26.3 vs 7.0, P = 0.277) (Table 3).
| Fistulous communication | N (fem) | Site of perforation | Preoperative diagnosis | Laparoscopic cholecystectomy (converted) | Open cholecystectomy | Conservative | Added procedures | ||
| Fundus | Body | Neck | |||||||
| Abdominal wall | 11 (8) | 3 | 3 | 3 | 9 | 3 (1) | 7 | 1 | 1 ERCP |
| Gastric | 4 (4) | - | - | 1 | 2 | 2 | 1 | 1 | |
| Duodenum | 3 (1) | - | - | - | 3 | 2 (2) | 2 | 1 | 1 ERCP |
| Colon | 2 (1) | 2 | - | - | 2 | 0 | 2 | 0 | 1 ERCP |
| Pleura | 1 (0) | - | - | - | 1 | 1 | 0 | 0 | 1 pleural tube |
| Total | 20 (13)1 | 5 | 3 | 31 | 161 | 8 (3) | 12 | 3 | 4 |
A total of 35 patients were included from two cohort studies, with a mean age of 62.45 years, of which 60% were female (Table 4). Similar to case reports/series, the most common comorbidities were cardiovascular diseases (n = 7) and diabetes mellitus (n = 7). The most frequent site of perforation was the gallbladder’s body (n = 16) followed by the fundus (n = 14). Less than half (n = 13) were diagnosed pre-operatively. One study favored OC (n = 17/20) with a higher mean of DoH (10.60 d), while the other study favored LC (n = 14/15) with a shorter mean of DoH (1.69 d), although this was from a larger sample, and not only fistulous GBP.
Both cohort studies included had a moderate risk of bias. This was due to concerns in the domains of bias due to confounding, and bias in the measurement of outcomes due to the lack of blinding (Supplementary Table 2)[10,42]. Except for two case reports and one case series which had an overall low risk of bias, the rest presented a moderate risk of bias. This was most commonly due to the patient(s) selection, as it did not represent the whole experience of the investigator’s center (Supplementary Table 3)[26-41].
In patients from case reports/series (Table 3), there was a similar proportion of patients presenting any complication post-OC and post-LC (28.6% vs 12.5%; P = 0.569). LC had a higher proportion of need for another intervention compared to OC, although this outcome was not statistically significant. The mortality proportion was higher in OC than in LC (14.3% vs 0.0%; P = 0.467), but this was given by only one patient. DoH were higher in patients undergoing OC than LC (mean 26.3 d vs 6.6 d), although this outcome was not statistically significant (P = 0.277). Patients receiving conservative treatment did not present any morbidity or mortality.
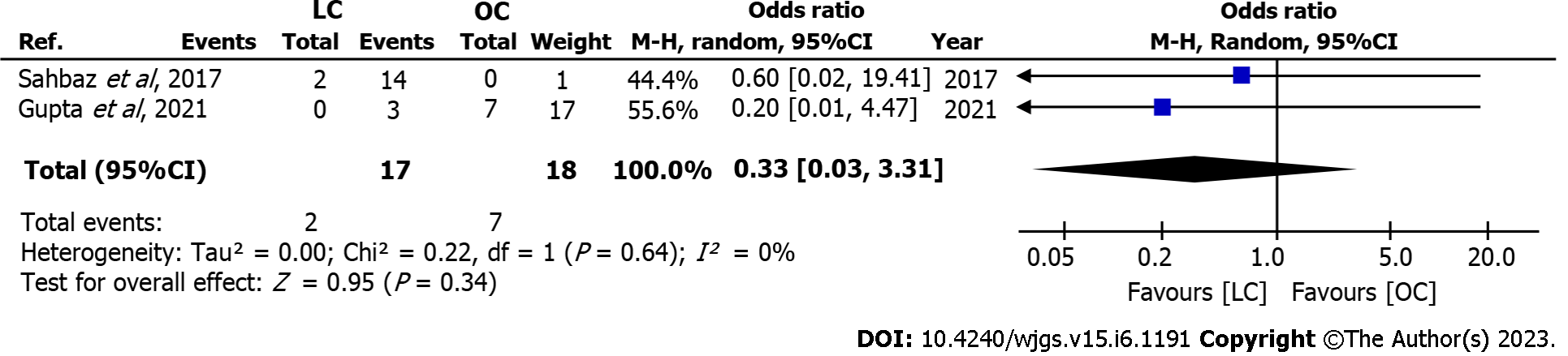
In patients from included cohort studies, no mortality was observed in either intervention. Two patients in the LC group and seven in the OC group presented a complication after the intervention. However, there was no clear association between higher rates of complications of a given intervention (odds ratio = 0.33, 95% confidence interval: 0.03-3.31; I2= 0%, P = 0.64). Three LC were converted to OC and none of the OC needed another intervention (Figure 2).
This systematic review summarizes the management of patients with Niemeir type I GBP (perforation with a fistulous tract). A fistulous communication may be formed as a result of chronic GBP with various structures. There is a higher prevalence in women, and the abdominal wall is the most common site, followed by hollow viscera (stomach, duodenum, and colon), and the pleural cavity in one case[36,42-44]. There was no statistically significant difference between OC and LC; however, LC tended to have fewer DoH, in both case reports/series and cohorts.
The first report of this rare complication was described in 1670 by Thilesus[42]. In 1890, Courvoisier reported 169 cases of spontaneous cholecystocutaneous fistulae[45]. The most commonly reported cutaneous communication occurred in the right upper quadrant; however, the left upper quadrant, right iliac fossa, periumbilical, anterior chest wall, and gluteal region have also been described[32,40,42,46-48]. The ideal imagining modalities for the diagnosis are ultrasonography followed by CT with a fistulography. Clinical management includes analgesic therapy, antimicrobials, and individualized surgical treatment. OC and LC are both described as ideal surgical options for scheduled interventions. Complete excision of the fistulous tract is the recommended surgical treatment. Conservative approaches such as percutaneous cholecystectomy with drain insertion may be considered for high-risk patients or in palliative care settings[13,49].
Gastric and duodenum fistulae were the most common internal communications. This is due to their anatomical proximity to the gallbladder. US and CT are helpful in diagnosis, most of these being identified preoperatively; however, 22% of hollow visceral communications were transoperative findings[50]. OC was the preferred approach, with a conversion rate of 37.5% in LC (n = 3/8).
The cholecystocolic fistulae were also reported. These have been associated with other pathologies such as a history of gastric surgery, diverticular disease, trauma, or gallbladder carcinoma. Most of the patients are asymptomatic; however, diarrhea, right upper abdominal pain, fever, and jaundice can be present, and rarely hemorrhage, sepsis, or extraperitoneal abscess[44,46]. Savvidou et al[38] proposed a triad of pneumobilia, chronic diarrhea, and vitamin K malabsorption to be pathognomonic of a chlolecystocolic fistula. The clinical presentation of both reported cases had watery diarrhea and weight loss in common. Cholecystectomy with resection of the fistulous tract is the standard treatment, although in difficult cases a partial colonic resection may be required[30,46].
The reported cholecystopleural fistula was diagnosed by US and CT. The patient presented with malaise, vomiting, and dyspnea. The presence of Escherichia coli in the thoracentesis confirmed the imaging diagnosis. A laparoscopic approach with fistulous communication resection was decided to avoid negative pressure drainage with a chest tube[17]. A thoracic vs abdominal approach for the resection is still controversial[26].
The predominant site of GBP for fistulous communication was equal between the fundus (n = 19) and body (n = 19). The healing of the gallbladder due to the chronicity of the pathology may influence this, as the fundus has been described as the most common site of perforation due to the lowest vascular supply[5].
A chronic GBP with fistulous communication with the bile duct may be classified as Niemeier type I, but is more commonly known as the Mirizzi syndrome. A chronic inflammation is caused by a calculus stuck in the Hartmann or neck of the gallbladder, creating a fistula with the biliary tract. Mirizzi syndrome should be considered separately and recommendations made independently, as it requires urgent surgical intervention due to the obstruction of the biliary tract and its implications[51-53]. Niemeier type I can be scheduled when the patient’s clinical state allows it, and even be managed conservatively in unstable patients.
More studies detailing GBP characteristics and management are needed to update current guidelines. No difference was established between OC and LC, with half the cases in recent years managed conventionally. To choose the optimal surgical technique, the surgeon must evaluate the advantages and disadvantages of the therapeutic options, the resources available in their environment, and their expertise. In patients with multiple co-morbidities and a high risk of trans- and post-operative complications, conservative medical treatment should be considered.
More cohort studies are needed to ascertain the effect estimates of the outcomes. Cohorts need to include subgroup analysis to delve across specific groups with GBP. The current cohorts do not specify the organ/structure of fistulous communication, limiting a proposal of management options based on organ/structure. Many of the corresponding authors did not respond to emails, or could not provide the specific data needed. A strength of this systematic review and meta-analysis is the rigorous methodology performed across all the steps of the review (search strategy-data analysis).
Open and LC are adequate options for surgical management of Neimeier type I GBP, with no significant differences in complications, DoH, or need for other interventions.
Gallbladder perforation (GBP) is rare and its management remains controversial.
Authors are experts in the field, and have a high interest in GBP management.
To determine the best management options for GBP.
A systematic review with rigorous search strategies.
Open cholecystectomy was associated with higher mortality and days of hospital stay.
Although each case needs to be individually analyzed and considered according to the surgeons expertise, laparoscopic cholecystectomy (LC) is a viable option.
Open cholecystectomy and LC are both adequate surgical management options for GBP.
We would like to thank Dr. Bipadabhanjan Mallick and Dr. Assamoi Brou Fulgence Kassi for their collaboration in answering emails and providing us with the needed data for the elaboration of this systematic review and meta-analysis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Mexico
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rasa HK, Turkey; Seretis C, Greece S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Wu RR
| 1. | Derici H, Kara C, Bozdag AD, Nazli O, Tansug T, Akca E. Diagnosis and treatment of gallbladder perforation. World J Gastroenterol. 2006;12:7832-7836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 116] [Cited by in RCA: 139] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 2. | Kochar K, Vallance K, Mathew G, Jadhav V. Intrahepatic perforation of the gall bladder presenting as liver abscess: case report, review of literature and Niemeier's classification. Eur J Gastroenterol Hepatol. 2008;20:240-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Hussain T, Adams M, Ahmed M, Arshad N, Solkar M. Intrahepatic perforation of the gallbladder causing liver abscesses: case studies and literature review of a rare complication. Ann R Coll Surg Engl. 2016;98:e88-e91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Taneja S, Sharma A, Duseja AK, Kalra N, Chawla Y. Spontaneous perforation of gallbladder with intrahepatic bilioma. J Clin Exp Hepatol. 2011;1:210-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Morris BS, Balpande PR, Morani AC, Chaudhary RK, Maheshwari M, Raut AA. The CT appearances of gallbladder perforation. Br J Radiol. 2007;80:898-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, Kozaka K, Endo I, Deziel DJ, Miura F, Okamoto K, Hwang TL, Huang WS, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Noguchi Y, Shikata S, Ukai T, Higuchi R, Gabata T, Mori Y, Iwashita Y, Hibi T, Jagannath P, Jonas E, Liau KH, Dervenis C, Gouma DJ, Cherqui D, Belli G, Garden OJ, Giménez ME, de Santibañes E, Suzuki K, Umezawa A, Supe AN, Pitt HA, Singh H, Chan ACW, Lau WY, Teoh AYB, Honda G, Sugioka A, Asai K, Gomi H, Itoi T, Kiriyama S, Yoshida M, Mayumi T, Matsumura N, Tokumura H, Kitano S, Hirata K, Inui K, Sumiyama Y, Yamamoto M. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:41-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 769] [Cited by in RCA: 689] [Article Influence: 98.4] [Reference Citation Analysis (0)] |
| 7. | Sugrue M, Sahebally SM, Ansaloni L, Zielinski M, Coccolini F. In response to the article entitled "The Parkland grading scale for cholecystitis" by Madni et al. In Madni TD, Leshikar DE, Minshall CT, Nakonezny PA, Cornelius CC, Imran JB, Clark AT, Williams BH, Eastman AL, Minei JP, Phelan HA. The Parkland grading scale for cholecystitis. In Am J Surg; 2017 Jun 6. doi.org/10.1016/j.amjsurg.2017.05.017. Am J Surg. 2019;217:193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Niemeier OW. Acute Free Perforation of the Gall-Bladder. Ann Surg. 1934;99:922-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 175] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 9. | Angeles-Mar HJ, Garcia-Campa M, Elizondo-Omaña RE, Guzmán-López S, Martinez-Garza JH, Quiroga-Garza A. Letter to the Editor concerning: Gallbladder perforation: A single-center experience in north India and a step-up approach for management. Hepatobiliary Pancreat Dis Int. 2022;21:617-618. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Gupta V, Chandra A, Gupta V, Patel R, Dangi A, Pai A. Gallbladder perforation: A single-center experience in north India and a step-up approach for management. Hepatobiliary Pancreat Dis Int. 2022;21:168-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Angeles-Mar HJ, Elizondo-Omaña RE, Guzmán-López S, Quiroga-Garza A. Early laparoscopic cholecystectomy in acute gallbladder perforation-Single-centre experience. J Minim Access Surg. 2022;18:324-325. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Krishnamurthy G, Ganesan S, Ramas J, Damodaran K, Khanna A, Patta R. Early laparoscopic cholecystectomy in acute gallbladder perforation: Single-centre experience. J Minim Access Surg. 2021;17:153-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Quiroga-Garza A, Alvarez-Villalobos NA, Angeles-Mar HJ, Garcia-Campa M, Muñoz-Leija MA, Salinas-Alvarez Y, Elizondo-Omaña RE, Guzmán-López S. Localized gallbladder perforation: a systematic review of treatment and prognosis. HPB (Oxford). 2021;23:1639-1646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Singh K, Singh A, Vidyarthi SH, Jindal S, Thounaojam CK. Spontaneous Intrahepatic Type II Gallbladder Perforation: A Rare Cause of Liver Abscess - Case Report. J Clin Diagn Res. 2013;7:2012-2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Nikumbh T, Bhandarwar A, Sanap S, Wagholikar G. Laparoscopic management of intra-hepatic gallbladder perforation. J Minim Access Surg. 2020;16:77-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Kundan M, Chintamani, Kumari A. Gall Bladder Perforation: Still an Enigma in Tropics. Ind J Surg. 2019;81:277-283. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Lee MT, Hsi SC, Hu P, Liu KY. Biliopleural fistula: a rare complication of percutaneous transhepatic gallbladder drainage. World J Gastroenterol. 2007;13:3268-3270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Cunningham LW, Grobman M, Paz HL, Hanlon CA, Promisloff RA. Cholecystopleural fistula with cholelithiasis presenting as a right pleural effusion. Chest. 1990;97:751-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Delcò F, Domenighetti G, Kauzlaric D, Donati D, Mombelli G. Spontaneous biliothorax (thoracobilia) following cholecystopleural fistula presenting as an acute respiratory insufficiency. Successful removal of gallstones from the pleural space. Chest. 1994;106:961-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2603] [Cited by in RCA: 4474] [Article Influence: 1118.5] [Reference Citation Analysis (33)] |
| 21. | McGinn T, Wyer PC, Newman TB, Keitz S, Leipzig R, For GG; Evidence-Based Medicine Teaching Tips Working Group. Tips for learners of evidence-based medicine: 3. Measures of observer variability (kappa statistic). CMAJ. 2004;171:1369-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 371] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 22. | Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7683] [Cited by in RCA: 10881] [Article Influence: 1209.0] [Reference Citation Analysis (2)] |
| 23. | Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23:60-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1008] [Cited by in RCA: 1538] [Article Influence: 219.7] [Reference Citation Analysis (0)] |
| 24. | IBM Corp. IBM SPSS Statistics for Windows, Version 25.0. 2017. [cited 20 March 2023]. Available from: https://www.ibm.com/products/spss-statistics. |
| 25. | The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan) (Computer program), Version 5.3. [cited 20 March 2023]. Available from: https://training.cochrane.org/online-learning/core-software/revman. |
| 26. | Garza Báez P, Muñoz Leija D, Fernandez Reyes BA, Quiroga Garza A, Negreros Osuna AA. Gallbladder perforation with cholecystopleural fistula: a case report. Int Surg J. 2021;8:3141-3143. [DOI] [Full Text] |
| 27. | Victor NS, Paul N, Munjurpattu AJ, Raju RS. Masquerade: an unusual presentation of gall bladder perforation as umbilical fistula. BMJ Case Reports. 2021;14:e243862. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Pol MM, Vyas S, Singh P, Rathore, YS. Spontaneous cholecystocutaneous fistula: empirically treated for a missed diagnosis, managed by laparoscopy. BMJ Case Reports. 2019;12:e228138. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Patel G, Jain A, Kumar RB, Singh N, Karim T, Mishra R. Gallbladder perforation: a prospective study of its divergent appearance and management. Euroasian J Hepatogastroenterol. 2019;9:14. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Mallick B, Bhattacharya A, Gupta P, Rathod S, Dahiya D, Dutta U. Cholecystocolic fistula diagnosis with hepatobiliary scintigraphy: A case report. JGH Open. 2019;3:91-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Kassi ABF, Koffi E, Yénon KS, Bombet-Kouamé C. Cholecystoparietal Fistula Revealed by an Epigastric Abscess. Case Rep Gastroenterol. 2017;11:225-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Kohli DR, Anis M, Shah T. Cholecystoenteric Fistula Masquerading as a Bleeding Subepithelial Mass. ACG Case Rep J. 2017;4:e125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Mughal Z, Green J, Whatling PJ, Patel R, Holme TC. Perfoation of the gallbladder: 'bait' for the unsuspecting laparoscopic surgeon. Ann R Coll Surg Engl. 2017;99:e15-e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Varshney P, Dhaked SK, Gothwal S, Songra B, Mathur S. Gallbladder perforation presenting as abdominal and chest wall abscess. J Case Rep. 2014;4:1-3. [DOI] [Full Text] |
| 35. | Gupta V, Benerjee S, Garg H, Vyas S. Spontaneous cholecysto-antral-cutaneous fistula: a consequence of neglected calculus cholecystitis. Singapore Med J. 2012;53:e201-e203. [PubMed] |
| 36. | Date RS, Thrumurthy SG, Whiteside S, Umer MA, Pursnani KG, Ward JB, Mughal MM. Gallbladder perforation: case series and systematic review. Int J Surg. 2012;10:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 37. | Sayed L, Sangal S, Finch G. Spontaneous cholecystocutaneous fistula: a rare presentation of gallstones. J Surg Case Rep. 2010;2010:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 38. | Savvidou S, Goulis J, Gantzarou A, Ilonidis G. Pneumobilia, chronic diarrhea, vitamin K malabsorption: a pathognomonic triad for cholecystocolonic fistulas. World J Gastroenterol. 2009;15:4077-4082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 39. | Marwah S, Godara R, Sandhu D, Karwasra R. Spontaneous gallbladder perforation presenting as abdominal wall abscess. Int J Surg. 2007;12. |
| 40. | Baron TH, Farnell MB, Leroy AJ. Endoscopic transpapillary gallbladder drainage for closure of calculous gallbladder perforation and cholecystoduodenal fistula. Gastrointest Endosc. 2002;56:753-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 41. | Carragher AM, Jackson PR, Panesar KJ. Subcutaneous herniation of gall-bladder with spontaneous cholecystocutaneous fistula. Clin Radiol. 1990;42:283-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 42. | Sahbaz NA, Peker KD, Kabuli HA, Gumusoglu AY, Alis H. Single center experience in laparoscopic treatment of gallbladder perforation. Wideochir Inne Tech Maloinwazyjne. 2017;12:372-377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 43. | Rinzivillo NMA, Danna R, Leanza V, Lodato M, Marchese S, Basile F, Zanghì GN. Case Report: Spontaneous cholecystocutaneous fistula, a rare cholethiasis complication. F1000Res. 2017;6:1768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 44. | Glenn F, Reed C, Grafe WR. Biliary enteric fistula. Surg Gynecol Obstet. 1981;153:527-531. [PubMed] |
| 45. | Courvoisier L. Kasuistisch-statistische Beiträge Zur Pathologie und Chirurgie Der Gallenwege. Dtsch Med Wochenschr. 1892;18:554. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 46. | Costi R, Randone B, Violi V, Scatton O, Sarli L, Soubrane O, Dousset B, Montariol T. Cholecystocolonic fistula: facts and myths. A review of the 231 published cases. J Hepatobiliary Pancreat Surg. 2009;16:8-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 106] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 47. | Nicholson T, Born MW, Garber E. Spontaneous cholecystocutaneous fistula presenting in the gluteal region. J Clin Gastroenterol. 1999;28:276-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 48. | Thiruchandran G, Joyce M, Baggott PJ. A rare case of gallbladder fistulation with a 60-year-old appendicectomy scar. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 49. | Kasper P, Kaminiorz J, Schramm C, Goeser T. Spontaneous cholecystocutaneous fistula: an uncommon complication of acute cholecystitis. BMJ Case Rep. 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 50. | Chowbey PK, Bandyopadhyay SK, Sharma A, Khullar R, Soni V, Baijal M. Laparoscopic management of cholecystoenteric fistulas. J Laparoendosc Adv Surg Tech A. 2006;16:467-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 84] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 51. | Lee CK, Ramcharan DN, Alaimo KL, Velez V, Risden AE, Klein DH, Garcia O, Joshi V, Jorge JM. Cholecystoduodenal Fistula Evading Imaging and Endoscopic Retrograde Cholangiopancreatography: A Case Report. Cureus. 2021;13:e20049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 52. | Kehr H. Die in Meiner Klinik Geubte Technik Der Gallensteinoperationen Mit Einem Hinweis Auf Die Indikationen Und Die Dauererfolge. Munchen, Germany: JF Lehman, 1905. [DOI] [Full Text] |
| 53. | Beltran MA, Csendes A, Cruces KS. The relationship of Mirizzi syndrome and cholecystoenteric fistula: validation of a modified classification. World J Surg. 2008;32:2237-2243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 104] [Article Influence: 6.5] [Reference Citation Analysis (1)] |