Published online Dec 27, 2023. doi: 10.4240/wjgs.v15.i12.2792
Peer-review started: October 30, 2023
First decision: November 8, 2023
Revised: November 14, 2023
Accepted: December 8, 2023
Article in press: December 8, 2023
Published online: December 27, 2023
Processing time: 58 Days and 3.9 Hours
Postoperative pancreatic fistula (POPF) is one of the most serious complications after pancreaticoduodenectomy (PD), and the choice of pancreaticojejunostomy (PJ) is considered a key factor affecting the occurrence of POPF. Numerous anastomotic methods and their modifications have been proposed, and there is no method that can completely avoid the occurrence of POPF. Based on our team’s experience in pancreatic surgery and a review of relevant literature, we describe a novel invagination procedure for PJ using double purse string sutures, which has resulted in favourable outcomes.
To describe the precise procedural steps, technical details and clinical efficacy of the novel invagination procedure for PJ.
This study adopted a single-arm retrospective cohort study methodology, involving a total of 65 consecutive patients who underwent PD with the novel invagination procedure for PJ, including the placement of a pancreatic stent, closure of the residual pancreatic end, and two layers of purse-string suturing. Baseline data included age, sex, body mass index (BMI), pancreatic texture, pancreatic duct diameter, operation time, and blood loss. Clinical outcomes included the operation time, blood loss, and incidence of POPF, postoperative haemorrhage, delayed gastric emptying, postoperative pulmonary infection, postoperative abdominal infection, and postoperative pulmonary infection.
The mean age of the patients was 59.12 (± 8.08) years. Forty males and 25 females were included, and the mean BMI was 21.61 kg/m2 (± 2.74). A total of 41.53% of patients had a pancreatic duct diameter of 3 mm or less. The mean operation time was 263.83 min (± 59.46), and the mean blood loss volume was 318.4 mL (± 163.50). Following the surgical intervention, only three patients showed grade B POPF (4.62%), while no patients showed grade C POPF. Five patients (5/65, 7.69%) were diagnosed with postoperative haemorrhage. Six patients (6/65, 9.23%) experienced delayed gastric emptying. Four patients (4/65, 6.15%) developed postoperative pulmonary infection, while an equivalent number (4/65, 6.15%) exhibited postoperative abdominal infection. Additionally, two patients (2/65, 3.08%) experienced postoperative pulmonary infection.
The novel invagination technique for PJ is straightforward, yields significant outcomes, and has proven to be safe and feasible for clinical application.
Core Tip: A novel invagination procedure for pancreaticojejunostomy (PJ) was proposed in this article, leading to significant improvements in outcomes. The incidence of postoperative pancreatic fistula with this method was only 4.65%. This standardized PJ method is a dependable and secure surgical technique that has high clinical significance and should be implemented widely in clinical settings.
- Citation: Li J, Niu HY, Meng XK. Novel invagination procedure for pancreaticojejunostomy using double purse string sutures: A technical note. World J Gastrointest Surg 2023; 15(12): 2792-2798
- URL: https://www.wjgnet.com/1948-9366/full/v15/i12/2792.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i12.2792
Pancreaticoduodenectomy (PD) currently represents the treatment of choice for benign or malignant pancreatic and periampullary malignant tumours[1]. In recent years, with continuous improvements in surgical techniques and perioperative management, the mortality rate associated with PD has been reduced to 5%, but the postoperative complication rate is still as high as 50%[2,3]. Postoperative pancreatic fistula (POPF) is the most serious complication in patients who undergo PD, with a reported incidence of 10%-30% in the literature[4]. Specifically, the occurrence of pancreatic fistulas contributes to prolonged hospitalization and significantly increased costs and can even cause death[5]. Multiple anastomotic techniques and their modifications have been suggested, such as pancreaticogastrostomy, duct-to-mucosa anastomosis, and invagination pancreaticojejunostomy (PJ). However, none of these methods can entirely prevent the occurrence of POPF.
The efficacy and safety of these methods have been the subjects of discussion for several decades, but the results have significantly varied across studies[6]. A randomized clinical trial of pancreatogastrostomy (PG) vs. PJ showed no difference in the rate of POPF, but there were more postoperative bleeding events with PG[7]. The most widely used procedure in PD, duct-to-mucosa PJ, poses technical challenges during PD, especially in patients with a soft pancreas and nondilated main pancreatic ducts[8]. However, in high-risk patients with a soft pancreas in a low-volume centre, invagination PJ may reduce the risk of clinically relevant POPF compared with duct-to-mucosa PJ. For one reason, it is easy to mobilize and invaginate the pancreatic stump into the jejunum during invagination PJ[9]. Furthermore, the difficulty of PJ does not depend on the main pancreatic duct diameter. Therefore, this may be an ideal technique applicable for all patients[10].
Herein, based on our team’s experience in pancreatic surgery and the relevant literature, we describe a novel, convenient, and simple invagination technique, referred to as the novel invagination procedure for PJ. In this anastomotic method, the pancreatic stump was closed with continuous sutures, and a double purse-string technique was used in PJ. To date, this technique has been successfully applied in over 60 cases, yielding favourable outcomes.
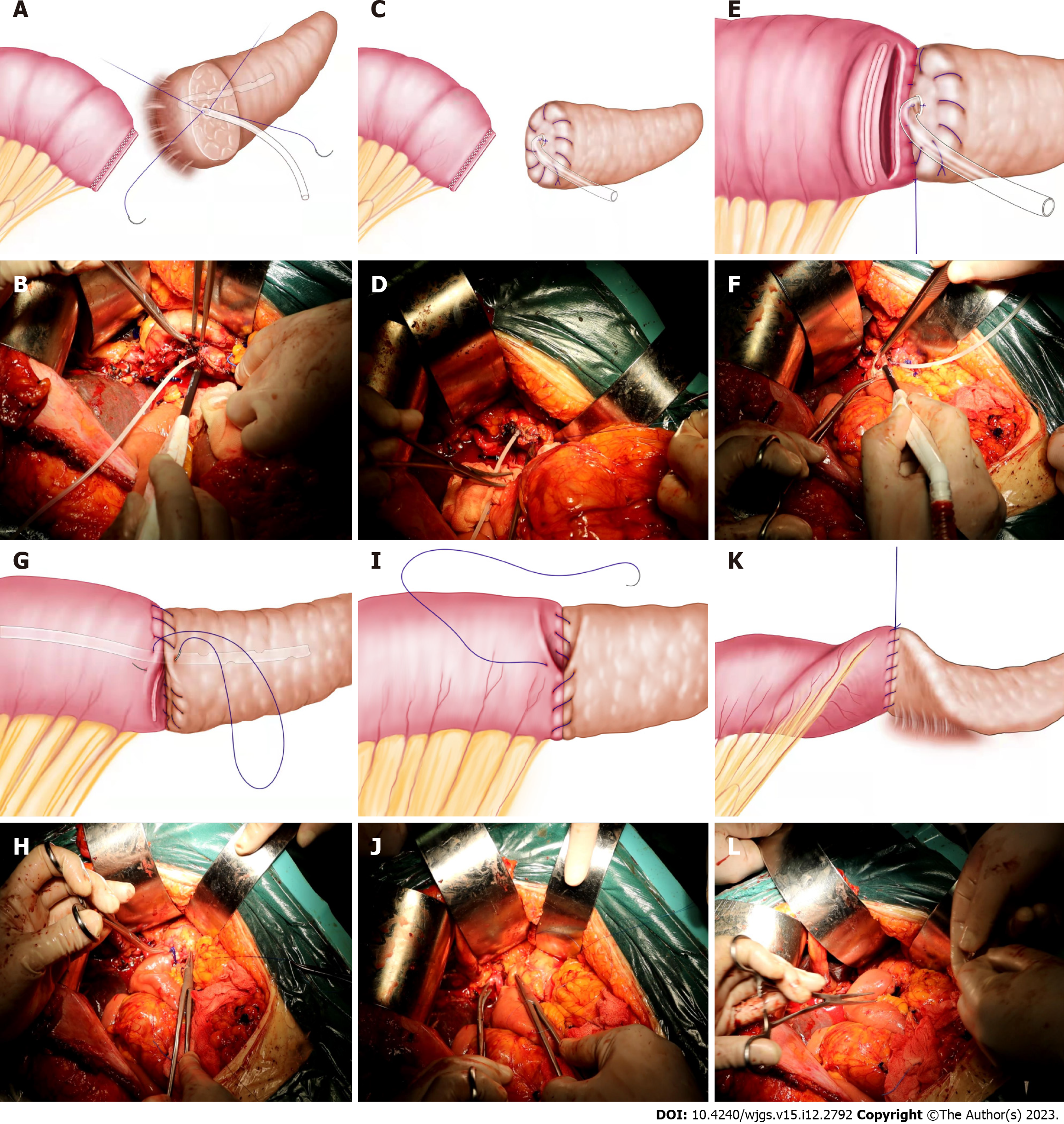
Placement of the pancreatic stent: After carefully achieving haemostasis at a distance of 2 cm from the free end of the pancreatic duct, the main pancreatic duct was delicately incised using tissue scissors. Subsequently, a silicone tube with comparable dimensions to the residual main pancreatic duct was inserted as a supportive conduit. To facilitate pancreatic fluid drainage, the lateral wall of the supportive conduit was punctured with three to four small apertures. The pancreatic stent was fixed traverse to the abdominal and dorsal aspects of the supportive conduit using 4-0 absorbable sutures, passing through the main pancreatic duct and the surrounding pancreatic tissue to ensure secure attachment (Figure 1A and B).
Closure of the residual pancreatic end: The surrounding residual pancreatic tissue of the main pancreatic duct was meticulously sutured using a 4-0 Prolene thread passed through the pancreatic parenchyma, traversing the pancreatic capsule in a continuous locking pattern. This procedure effectively sealed the residual end of the pancreas (Figure 1C and D).
First layer of purse-string suturing: Using a 4-0 Prolene thread, the needle was inserted inwards from the interior of the pancreatic parenchyma. After traversing the pancreatic tissue, the needle emerged at a distance of 2 cm from the residual end of the pancreas. Using the same needle, a corresponding vertical edge of the jejunal posterior wall was punctured 2 cm from the duodenal margin, penetrating through the muscular layer of the jejunum and exiting 0.5 cm away. Maintaining a needle distance of 0.5 cm, the suture was gradually tightened, ensuring a snug fit between the residual pancreatic end and the jejunal wall. This continuous suturing technique was repeated for 6-8 stitches, completing the posterior anastomosis of the pancreatic-duodenal junction. A small incision was made in the corresponding end of the jejunum, opposite to the pancreatic stent, using an electric scalpel (Figure 1E and F). The size of the incision was adjusted to allow smooth insertion of the residual pancreatic end into the jejunum. The pancreatic stent was then inserted approximately 5 cm into the jejunal lumen, and continuous suturing using the same technique was performed for anterior anastomosis of the pancreatic-duodenal junction (Figure 1G and H).
Secondary layer of purse-string suturing: Using a 4-0 Prolene thread, a continuous purse-string suture was applied again 0.5 cm from the first anastomotic site, ensuring complete envelopment and adherence of the jejunum around the residual pancreatic end. Starting from the jejunal end, the needle traversed through the muscular layer of the jejunum and emerged 0.5 cm from the first anastomotic site. Using the same needle, the pancreatic capsule was penetrated at a corresponding point 0.5 cm away from the first anastomotic site, passing through the pancreatic parenchyma and exiting 0.5 cm from the needle entry point. After tightening the suture, posterior anastomosis of the pancreatic-duodenal junction was completed (Figure 1I and J). Following a similar approach, the anterior muscular layer of the jejunum was continuously sutured to the corresponding pancreatic parenchyma. The suture was gradually tightened, and upon completion of the knotting, the second layer of purse-string sutures was completed, thus concluding the pancreatic-duodenal anastomotic process (Figure 1K and L). Upon the completion of continuous purse-string suturing between the residual pancreatic end and the jejunal muscular layer, the muscular layer of the jejunal creates an "invaginated cuff", resembling an inwardly folded sleeve, allowing the residual pancreatic end to be fully encapsulated within this "cuff". Finally, bilioenteric and gastroenteric anastomoses were created, achieving reconstruction of the gastrointestinal tract.
The mean age of the patients was 59.12 (± 8.08) years. Forty males and 25 females were included, and the mean body mass index was 21.61 kg/m2 (± 2.74). A total of 41.53% of patients had a pancreatic duct diameter of 3 mm or less. The mean operation time was 263.83 min (± 59.46), and the mean blood loss volume was 318.4 mL (± 163.50) (Table 1). All patients underwent internal stent placement within the pancreatic duct.
| Parameters | n = 65 |
| Age (yr) | 59.12 ± 8.08 |
| Sex (%) | |
| Male | 40 (61.54) |
| Female | 25 (38.46) |
| Body mass index (kg/m2) | 21.61 ± 2.74 |
| Pancreatic texture | |
| Soft | 26 (34.67) |
| Hard | 39 (52.00) |
| Pancreatic duct diameter | |
| < 3 mm | 27 (41.53) |
| ≥ 3 mm | 38 (58.46) |
| Operation time (min) | 263.83 ± 59.46 |
| Blood loss (mL) | 318.40 ± 163.50 |
After undergoing surgery, three (3/65, 4.62%) patients showed grade B POPF, while no patients showed grade C POPF. Five patients (5/65, 7.69%) were diagnosed with postoperative haemorrhage. Six patients (6/65, 9.23%) were diagnosed with delayed gastric emptying. Four patients (4/65, 6.15%) showed postoperative pulmonary infection, four patients (4/65, 6.15%) showed postoperative abdominal infection, and two patients (2/65, 3.08%) showed postoperative pulmonary infection.
PD is the main surgical procedure for benign or malignant tumours around the head of the pancreas, the lower bile duct and ampulla. The procedure involves the removal of numerous organs and reconstruction of various digestive tract segments, including the pancreas, biliary tract, and gastrointestinal tract, and is associated with a high risk of postoperative complications, with an incidence of 30%-60%[11]. In fact, POPF remains the most common complication after pancreatic surgery, occurring in up to 30% of patients, even in high-volume centres[12,13]. PJ, as an independent risk factor for the development of POPF after PD, is considered the most controllable factor, and choosing to forego the procedure is the key to effectively preventing POPF[8,14]. Several PJ methods and their modifications, including pancreaticogastrostomy, duct-to-mucosa PJ and invagination PJ, have been proposed to reduce the incidence of POPF[15,16]. However, none of the PJ techniques have achieved significant results[17]. Based on its unique advantages and relatively low incidence of POPF, invagination PJ has been shown to be a safe and reliable procedure[18]. However, there have been discussions regarding the practical use of invagination PJ, including the problem associated with cutting sutures. Haemorrhage of the pancreatic stump due to immersion of the stump in the intestinal cavity and problems such as leakage of pancreatic fluid between sutures caused by the use of intermittent sutures have not been adequately addressed.
In this study, we used a novel invagination procedure to completely invaginate the pancreatic stump into the jejunal lumen. Remarkably, only three patients exhibited grade B POPF, with no instances of grade C POPF observed. Postoperative haemorrhage was diagnosed in five patients. Delayed gastric emptying was identified in six patients. Four patients developed postoperative pulmonary infection, while four patients experienced postoperative abdominal infection. Additionally, two patients displayed postoperative pulmonary infection. The data in this study showed that the novel invagination procedure is safe and simple to perform, irrespective of the pancreatic stump condition.
Compared to previous PJ methods, this procedure has the following differences: (1) The surface of the pancreatic remnant exhibits numerous small arteries and pancreatic duct branches. By focusing on the main pancreatic duct as the core, the residual glandular tissue is closed with continuous sutures, thereby preventing pancreatic fluid leakage at the pancreatic-enteric anastomotic site. Simultaneously, this approach reduces the exposed surface area of the pancreatic remnant, enhancing its resilience and minimizing the risks of POPF and haemorrhage. Furthermore, there is no risk of cutting damage to the fragile pancreatic tissue during the pancreatic-enteric anastomotic process; (2) by employing continuous purse-string sutures, the gaps between the anastomotic sites are eliminated, thereby reducing the risk of pancreatic fluid leakage. Additionally, continuous suturing ensures consistent tension without the need for repeated knotting, thus reducing the overall procedural time; (3) during the double purse-string procedure for pancreatic-enteric anastomosis, the pancreatic parenchyma is intimately connected to the muscular layer of the jejunum through a transfixing suture technique, ensuring close apposition between the pancreatic remnant and the jejunum; (4) the double purse-string procedure effectively reduces tension at the anastomotic site while preserving the intact blood supply to the pancreatic remnant, thereby meeting the histological requirements for optimal tissue healing; and (5) during the suturing process, the assistant ensures tight closure of the sutures by applying moderate knotting force, thereby minimizing the cutting effect of the sutures on the pancreatic parenchyma. By utilizing a fine needle and sparse suturing technique, the damage to the pancreatic parenchyma caused by the sutures is reduced. The use of continuous sutures for pancreatic-enteric anastomosis significantly reduces the accumulation of pancreatic fluid and its corrosive effect on the anastomosis.
From the perspective of pancreatic-enteric anastomotic healing, regardless of the specific technique employed, the primary components consist of mucosal healing, which is achieved when the inner layer of the jejunal mucosa covers the pancreatic remnant, and fibrous healing between the outer layer of the jejunal serosa and the pancreatic remnant[14,19]. While duct-to-mucosa anastomosis achieves direct pancreatic-enteric alignment, an inadequate pancreatic duct length can compromise its blood supply, thereby affecting the healing rate of the anastomosis[20,21]. On the other hand, there are no restrictions on the diameter of the main pancreatic duct when performing the novel invagination procedure. Leveraging the rapid regenerative capacity of the jejunal mucosa allows permanent biological healing along the pancreatic duct and is conducive to supporting the tube and the residual pancreatic tissue.
In conclusion, based on the preliminary results, this PJ method is safe and reliable, has high value for clinical application, and can be used as a standardized surgical method in clinical practice.
Postoperative pancreatic fistula (POPF) is the most formidable complication following pancreaticoduodenectomy (PD). Among the risk factors influencing the occurrence of POPF, the pancreaticojejunostomy (PJ) method stands out as a significant, modifiable factor that serves as a pivotal aspect in preventing POPF.
To detail the surgical procedure and technical intricacies of the novel invagination technique for PJ and assess its safety and efficacy.
Through the innovative optimization of PJ, reduce the incidence of postoperative complications and enhance the long-term prognosis for patients.
This study employed a single-arm retrospective cohort study methodology to assess the effectiveness and safety of a novel invagination technique for PJ during PD.
Following application of the novel invagination technique for PJ, only three patients demonstrated grade B POPF, and no instances of grade C POPF were observed.
The novel invagination procedure for PJ demonstrates safety, reliability, and significant clinical applicability, thereby qualifying as a standardized surgical approach in clinical practice.
With the establishment of a standardized and homogeneous PJ method, a multicentre randomized controlled study can be conducted to further clarify its advantages, and animal experiments can subsequently be employed to elucidate the specific mechanisms and principles.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Chinese Society of Surgery; Chinese Society of Organ Transplantation; Chinese Society of Parenteral and Enteral Nutrition; Chinese Research Hospital Association Committee of Minimally Invasive Surgery; Chinese Research Hospital Association Committee of Pancreas.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chmura SJ, United States; Marubashi S, Japan S-Editor: Qu XL L-Editor: Webster JR P-Editor: Zhao S
| 1. | Hong D, Li H, Liu X, Jiang P, Yu G, Liu J, Liu Y, Lau WY. Incidence of postoperative pancreatic fistula after using a defined pancreaticojejunostomy technique for laparoscopic pancreaticoduodenectomy: A prospective multicenter study on 1033 patients. Int J Surg. 2022;101:106620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 2. | Schneider M, Hackert T, Strobel O, Büchler MW. Technical advances in surgery for pancreatic cancer. Br J Surg. 2021;108:777-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 3. | PARANOIA Study Group:; Writing group:, Halle-Smith JM, Pande R, Hall L, Hodson J, Roberts KJ; Steering committee:, Arshad A, Connor S, Conlon KCP, Dickson EJ, Giovinazzo F, Harrison E, de Liguori Carino N, Hore T, Knight SR, Loveday B, Magill L, Mirza D, Mitta A, Pandanaboyana S, Perry RJ, Pinkney T, Samra J, Siriwardena AK, Satoi S, Skipworth J, Stättner S, Sutcliffe RP, Tingstedt B, Roberts KJ. Perioperative interventions to reduce pancreatic fistula following pancreatoduodenectomy: meta-analysis. Br J Surg. 2022;109:812-821. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Enderes J, Pillny C, Matthaei H, Manekeller S, Kalff JC, Glowka TR. Clinically Relevant Pancreatic Fistula after Pancreaticoduodenectomy: How We Do It. Biology (Basel). 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Lubrano J, Bachelier P, Paye F, Le Treut YP, Chiche L, Sa-Cunha A, Turrini O, Menahem B, Launoy G, Delpero JR. Severe postoperative complications decrease overall and disease free survival in pancreatic ductal adenocarcinoma after pancreaticoduodenectomy. Eur J Surg Oncol. 2018;44:1078-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Petrova E, Suurmeijer JA, Mackay TM, Bolm L, Lapshyn H, Honselmann KC, van Santvoort HC, Koerkamp BG, Wellner UF, Keck T, Besselink MG; Dutch Pancreatic Cancer Group and DGAV StuDoQ|Pancreas. Outcome of pancreatic anastomoses during pancreatoduodenectomy in two national audits. Surgery. 2021;170:1799-1806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Andrianello S, Marchegiani G, Malleo G, Masini G, Balduzzi A, Paiella S, Esposito A, Landoni L, Casetti L, Tuveri M, Salvia R, Bassi C. Pancreaticojejunostomy With Externalized Stent vs Pancreaticogastrostomy With Externalized Stent for Patients With High-Risk Pancreatic Anastomosis: A Single-Center, Phase 3, Randomized Clinical Trial. JAMA Surg. 2020;155:313-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 94] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 8. | Wang W, Zhang Z, Gu C, Liu Q, Liang Z, He W, Chen J, Lai J. The optimal choice for pancreatic anastomosis after pancreaticoduodenectomy: A network meta-analysis of randomized control trials. Int J Surg. 2018;57:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 9. | Senda Y, Shimizu Y, Natsume S, Ito S, Komori K, Abe T, Matsuo K, Sano T. Randomized clinical trial of duct-to-mucosa versus invagination pancreaticojejunostomy after pancreatoduodenectomy. Br J Surg. 2018;105:48-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 10. | Kobayashi S, Otsubo T, Koizumi S. Novel Modified Blumgart Technique to Reduce Postoperative Pancreatic Fistula After Pancreaticojejunostomy-Compressed Pancreatic Stump (COMPAS) Anastomosis. J Gastrointest Surg. 2021;25:1082-1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Olakowski M, Grudzińska E, Mrowiec S. Pancreaticojejunostomy-a review of modern techniques. Langenbecks Arch Surg. 2020;405:13-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 12. | Ecker BL, McMillan MT, Asbun HJ, Ball CG, Bassi C, Beane JD, Behrman SW, Berger AC, Dickson EJ, Bloomston M, Callery MP, Christein JD, Dixon E, Drebin JA, Castillo CF, Fisher WE, Fong ZV, Haverick E, Hollis RH, House MG, Hughes SJ, Jamieson NB, Javed AA, Kent TS, Kowalsky SJ, Kunstman JW, Malleo G, Poruk KE, Salem RR, Schmidt CR, Soares K, Stauffer JA, Valero V, Velu LKP, Watkins AA, Wolfgang CL, Zureikat AH, Vollmer CM Jr. Characterization and Optimal Management of High-risk Pancreatic Anastomoses During Pancreatoduodenectomy. Ann Surg. 2018;267:608-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 117] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 13. | Chiarello MM, Brisinda G. A Commentary on "Incidence and risk factors for postoperative pancreatic fistula in 2089 patients treated by radical gastrectomy: A prospective multicenter cohort study in China" (Int J Surg 2022;98:106219). Int J Surg. 2022;98:106239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 14. | Rivas L, Zettervall SL, Ju T, Olafson S, Holzmacher J, Lin PP, Vaziri K. The Effect of Pancreaticojejunostomy Technique on Fistula Formation Following Pancreaticoduodenectomy in the Soft Pancreas. J Gastrointest Surg. 2019;23:2211-2215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Xiang Y, Wu J, Lin C, Yang Y, Zhang D, Xie Y, Yao X, Zhang X. Pancreatic reconstruction techniques after pancreaticoduodenectomy: a review of the literature. Expert Rev Gastroenterol Hepatol. 2019;13:797-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Gupta V, Kumar S, Gupta V, Joshi P, Rahul R, Yadav RK, Dangi A, Chandra A. Blumgart's technique of pancreaticojejunostomy: Analysis of safety and outcomes. Hepatobiliary Pancreat Dis Int. 2019;18:181-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Kawaida H, Kono H, Hosomura N, Amemiya H, Itakura J, Fujii H, Ichikawa D. Surgical techniques and postoperative management to prevent postoperative pancreatic fistula after pancreatic surgery. World J Gastroenterol. 2019;25:3722-3737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 85] [Cited by in RCA: 119] [Article Influence: 19.8] [Reference Citation Analysis (4)] |
| 18. | Ratnayake CBB, Wells CI, Kamarajah SK, Loveday B, Sen G, French JJ, White S, Pandanaboyana S. Critical appraisal of the techniques of pancreatic anastomosis following pancreaticoduodenectomy: A network meta-analysis. Int J Surg. 2020;73:72-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Casciani F, Bassi C, Vollmer CM Jr. Decision points in pancreatoduodenectomy: Insights from the contemporary experts on prevention, mitigation, and management of postoperative pancreatic fistula. Surgery. 2021;170:889-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 20. | Bai X, Zhang Q, Gao S, Lou J, Li G, Zhang Y, Ma T, Xu Y, Liang T. Duct-to-Mucosa vs Invagination for Pancreaticojejunostomy after Pancreaticoduodenectomy: A Prospective, Randomized Controlled Trial from a Single Surgeon. J Am Coll Surg. 2016;222:10-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 21. | Dumitrascu T, Popescu I. Outcomes of Duct-to-Mucosa vs. Invagination Pancreatojejunostomy: Toward a Personalized Approach for Distal Pancreatic Stump Anastomosis in Central Pancreatectomy? J Pers Med. 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |