Published online Oct 27, 2023. doi: 10.4240/wjgs.v15.i10.2133
Peer-review started: May 18, 2023
First decision: August 10, 2023
Revised: August 22, 2023
Accepted: September 12, 2023
Article in press: September 12, 2023
Published online: October 27, 2023
Processing time: 162 Days and 7.9 Hours
A transjugular intrahepatic portosystemic shunt (TIPS) is widely placed to treat portal hypertension. Because the Viatorr® stent (W. L. Gore and Associates, Flagstaff, AZ, United States) is not available in all hospitals in China, the bare metal stent (BMS)/stent-graft combination technique is still popular for TIPS construction. Stent fracture is a complication after TIPS placement using this technique, with limited available literature focusing on it.
To assess the incidence of stent fracture after TIPS placement using the BMS/ stent-graft combination technique and to identify the risk factors for stent fracture. We proposed technique modifications to improve the clinical results of TIPS placement with the BMS/stent-graft combination technique.
We retrospectively analyzed the computed tomography (CT) data of all patients with portal hypertension who underwent the TIPS procedure between June 2011 and December 2021 in a single center. Patients implanted with the BMS/stent graft and had follow-up imaging data available were included. We identified patients with stent fracture and analyzed their characteristics. Multivariable logistic regression was applied to identify the potential predictors of stent fracture.
Of the 68 included patients, stent fracture occurred in seven (10.3%) patients. Based on CT images, the stent fractures were categorized into three types. Our study consisted of four (57.1%) type I fractures, one (14.3%) type II fracture, one (14.3%) type IIIa fracture, and one (14.3%) type IIIb fracture. After adjusting for covariates, multivariable logistic regression revealed that the risk factors for stent fracture were the implantation of a greater number of stents [adjusted odds ratio (aOR) = 22.2, 95% confidence interval (CI): 1.2-415.4, P = 0.038] and a larger proximal sagittal stent bending angle (aOR = 1.1, 95%CI: 1.0-1.3, P = 0.020).
Stent fracture occurred in approximately 10% of patients with portal hypertension who underwent TIPS with the BMS/stent-graft combination technique. The number of implanted stents and stent bending angle at the inferior vena cava end were predictors of stent fracture, which suggests that the incidence of stent fracture could potentially be reduced by procedural modifications.
Core Tip: The bare metal stent (BMS)/stent-graft combination technique for transjugular intrahepatic portosystemic shunt construction has an incidence of stent fractures of around 10%, which all occurred at the junction of BMS and the proximal end of the stent-graft. Fractures may be associated with the number of stents implanted and stent excessive bending. Hence, we recommend a greater overlap of the stent-graft with the BMS at the inferior vena cava (IVC) end of the shunt, and the selection of a position closer to the opening of the hepatic vein into the IVC as the starting puncture site to establish a shunt.
- Citation: Liu QJ, Cao XF, Pei Y, Li X, Dong GX, Wang CM. Stent fracture after transjugular intrahepatic portosystemic shunt placement using the bare metal stent/stent-graft combination technique. World J Gastrointest Surg 2023; 15(10): 2133-2141
- URL: https://www.wjgnet.com/1948-9366/full/v15/i10/2133.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i10.2133
The transjugular intrahepatic portosystemic shunt (TIPS) effectively controls portal hypertension and is especially important in patients with gastrointestinal bleeding or refractory ascites[1]. In China, TIPSs are frequently constructed using the bare metal stent (BMS)/stent-graft combination technique, in which a BMS is used to establish access between the hepatic and portal veins (PVs), and a stent graft is used to cover the liver parenchyma[2,3]. A stent fracture is a rare complication after TIPS placement using the BMS/stent-graft combination technique[4-8]. In addition to TIPS dysfunction, stent fracture may cause severe consequences such as tricuspid regurgitation if the fractured stent is displaced into the heart chamber[8].
In the present study, we retrospectively examined the clinical data of patients who underwent TIPS placement with the BMS/stent-graft combination technique to assess the incidence and analyze the potential causes of stent fracture. Based on this information, we proposed technique modifications to improve the clinical results of TIPS placement with the BMS/stent-graft combination technique.
The institutional review board of Peking University Third Hospital approved this retrospective study of data retrieved from electronic medical records. Ethical approval was granted by the Ethics Committee of Peking University Third Hospital, Beijing, China (No. M2022314). Patients who were admitted to Peking University Third Hospital between June 1, 2011 and December 31, 2021 and underwent TIPS placement with the BMS/stent-graft combination technique to treat complications of portal hypertension (e.g., gastrointestinal bleeding, refractory ascites) were included. Patients with no available follow-up computed tomography (CT) images were excluded.
The modified Child-Pugh classification was used to evaluate preoperative liver function. Liver function was categorized as Child-Pugh class A (Child-Pugh score 5-6, well-compensated disease), Child-Pugh class B (Child-Pugh score 7-9 points, significant functional compromise), or Child-Pugh class C (Child-Pugh score 10-15 points, decompensated disease)[9].
TIPS procedures were usually performed under local anesthesia. General anesthesia was used for patients with heavy bleeding and unstable blood circulation. A transjugular approach was used for all TIPS procedures. The RUPS-100 puncture device (Cook, Bloomington, IN, United States) was used in all patients.
Indirect portography was achieved by superior mesenteric arteriography or splenography. An angiography catheter was then selectively inserted into the left hepatic artery and retained as an indirect indicator of the left PV, which was the target vessel for puncture. Once the PV was successfully punctured, a pigtail angiographic catheter was introduced into the superior mesenteric vein to obtain an outline of the PV anatomy. The pressures in the PV and inferior vena cava (IVC) were recorded.
A guidewire (0.035 inch, Amplatz Super Stiff, Cordis Corporation, Fremont, CA, United States) was introduced and retained in the superior mesenteric vein. A 5 mm × 6 cm balloon was placed in the shunt for dilation. The length of the parenchymal segment of the shunt was recorded.
A 10-F sheath was advanced into the main stem of the PV. A 4-F Cobra catheter was introduced into the gastric coronary vein to identify the variceal veins and embolize them with coils or tissue adhesive.
A BMS was positioned between the left PV and IVC. With the deployment of the BMS, the liver parenchymal segment of the shunt (the narrow segment of the stent) was clearly displayed for stent-graft deployment. The portosystemic gradient (PSG) was measured. If the PSG was higher than needed, the shunt was dilated with a larger diameter balloon (> 5 mm). A stent graft with a corresponding diameter (Fluency®, Bard International, Inc., NJ, United States) was then deployed to exactly cover the parenchymal section of the shunt. If the PSG was lower than needed, a smaller diameter stent graft (Fluency®) with the same length as the parenchymal section was deployed. The final PSG was then recorded.
After the TIPS procedure, patients were followed up in the outpatient department. The patients’ symptoms, liver function, and shunt function were recorded. Color Doppler ultrasound and contrast-enhanced abdominal CT were used to evaluate the shunt blood flow dynamics and the status of the stents, especially the stent integrity. If ultrasound or CT revealed shunt dysfunction, digital subtraction angiography was performed, and the dysfunctional stent was corrected by shunt angioplasty and the implantation of another stent.
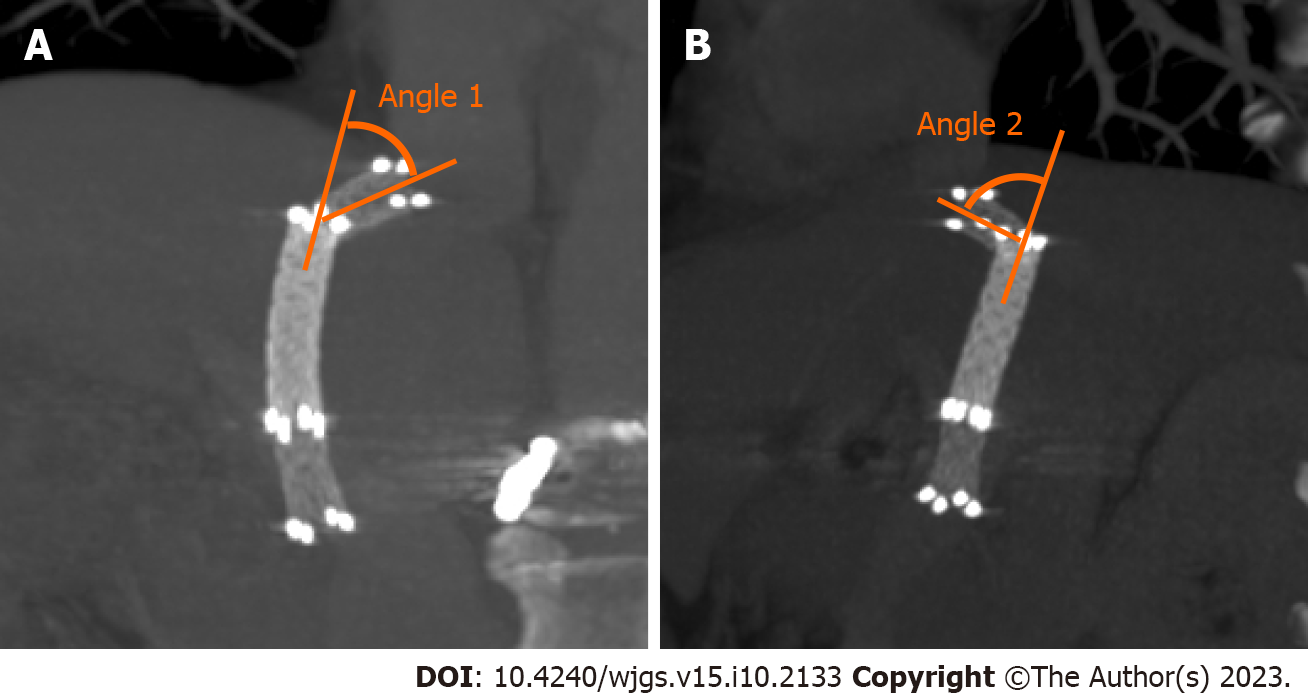
For construction of the TIPS, stents were placed between the IVC and the PV. The shunts were situated in a three-dimensional space within the liver, usually in an irregular three-dimensional configuration, rather than a simple two-dimensional orientation. CT images were analyzed to examine the proximal IVC segment of the shunt stents and to measure the bending angle of the stent axis of the end segment and the middle segment in both the coronal and sagittal planes, subsequently referred to as angle 1 and angle 2, respectively (Figure 1).
Patient characteristics, such as sex, age, Child-Pugh classification, number of deployed stents, stent bending angle of the proximal segment (angle 1 and angle 2), and revision operation details, were evaluated. Patients with stent fracture detected on follow-up CT were classified as the stent fracture group, while those without stent fracture were classified as the stent integrity group. Differences between the stent integrity group and stent fracture group were analyzed using Fisher’s exact test for categorical variables and the Mann-Whitney U test for continuous variables. Adjusted odds ratios (aORs) were computed by multivariable logistic regression to evaluate the associations between stent fracture and patient characteristics. The model was adjusted for covariates with clinical relevance and those found to be significant in univariate analyses. Two-sided P values of < 0.05 were considered statistically significant. Analyses were conducted using STATA/MP 14.0 software.
From June 1, 2011 to December 31, 2021, 137 patients underwent the TIPS procedure in the Department of Interventional Radiology and Vascular Surgery of Peking University Third Hospital. Among these 137 patients, 69 patients were excluded because of a lack of available postoperative CT images (63 patients) or TIPS placement with a single stent graft (six patients). Therefore, a final total of 68 patients were included in the analysis. The patient characteristics are summarized in Table 1. The median follow-up was 421 d (range: 1-2878 d), and the cohort included 38 (55.9%) men. The mean ± SD patient age was 60.7 ± 9.9 years (range: 33-82 years). A total of 151 stents were implanted, with an average of 2.2 stents implanted in each patient (range: 2-4). Eleven patients underwent revision surgery due to shunt dysfunction (stenosis/occlusion), including two in the stent fracture group and nine in the stent integrity group. All patients who underwent reoperation were implanted with a self-expanding BMS to restore shunt function.
| Characteristics | All | Integrity group | Fracture group | P valuea | |||
| No. patient | No. patient | No. patient | |||||
| Total | 68 | 100.0 | 61 | 89.7 | 7 | 10.3 | |
| Sex | |||||||
| Male | 38 | 55.9 | 34 | 89.5 | 4 | 10.5 | 0.633 |
| Female | 30 | 44.1 | 27 | 90.0 | 3 | 10.0 | |
| Age (yr) | |||||||
| ≤ 60 | 32 | 47.1 | 29 | 90.6 | 3 | 9.4 | 0.567 |
| > 60 | 36 | 52.9 | 32 | 88.9 | 4 | 11.1 | |
| Child-Pugh classification | |||||||
| A | 22 | 32.4 | 18 | 32.4 | 4 | 20.0 | 0.444 |
| B | 34 | 50.0 | 32 | 50.0 | 2 | 5.9 | |
| C | 12 | 17.6 | 11 | 17.6 | 1 | 8.3 | |
| Stent number | |||||||
| 2 | 55 | 80.9 | 51 | 92.7 | 4 | 7.3 | 0.095 |
| 3 | 11 | 16.2 | 9 | 81.8 | 2 | 18.2 | |
| 4 | 2 | 2.9 | 1 | 50.0 | 1 | 50.0 | |
| Reoperation | |||||||
| No | 59 | 86.8 | 54 | 91.5 | 5 | 8.5 | 0.230 |
| Yes | 9 | 13.2 | 7 | 77.8 | 2 | 22.2 | |
| Gradient | |||||||
| Portosystemic gradient (median, IQR) | 15.0 mmH2O (12.0-16.0) | 14.0 mmH2O (13.5-15.0) | 0.745 | ||||
| Stent angle | |||||||
| Angle 1 (median, IQR) | 1.0 (0-22.0) | 20.0 (3.5-35.0) | 0.151 | ||||
| Angle 2 (median, IQR) | 15.5 (0-33.8) | 39.5 (30.5-60.5) | 0.009 | ||||
The univariate Fisher’s exact test showed no significant differences between the stent fracture group and the stent integrity group in sex, age (> 60 years or ≤ 60 years), Child-Pugh classification, number of stents deployed, reoperation, or PSG (all P > 0.05). There was a tendency for angle 1 to be larger in the stent fracture group than in the stent integrity group, but this difference was not statistically significant (1.0 vs. 20.0, P = 0.151). Angle 2 was significantly larger in the stent fracture group than in the stent integrity group (15.5 vs. 39.5, P = 0.009, Table 1).
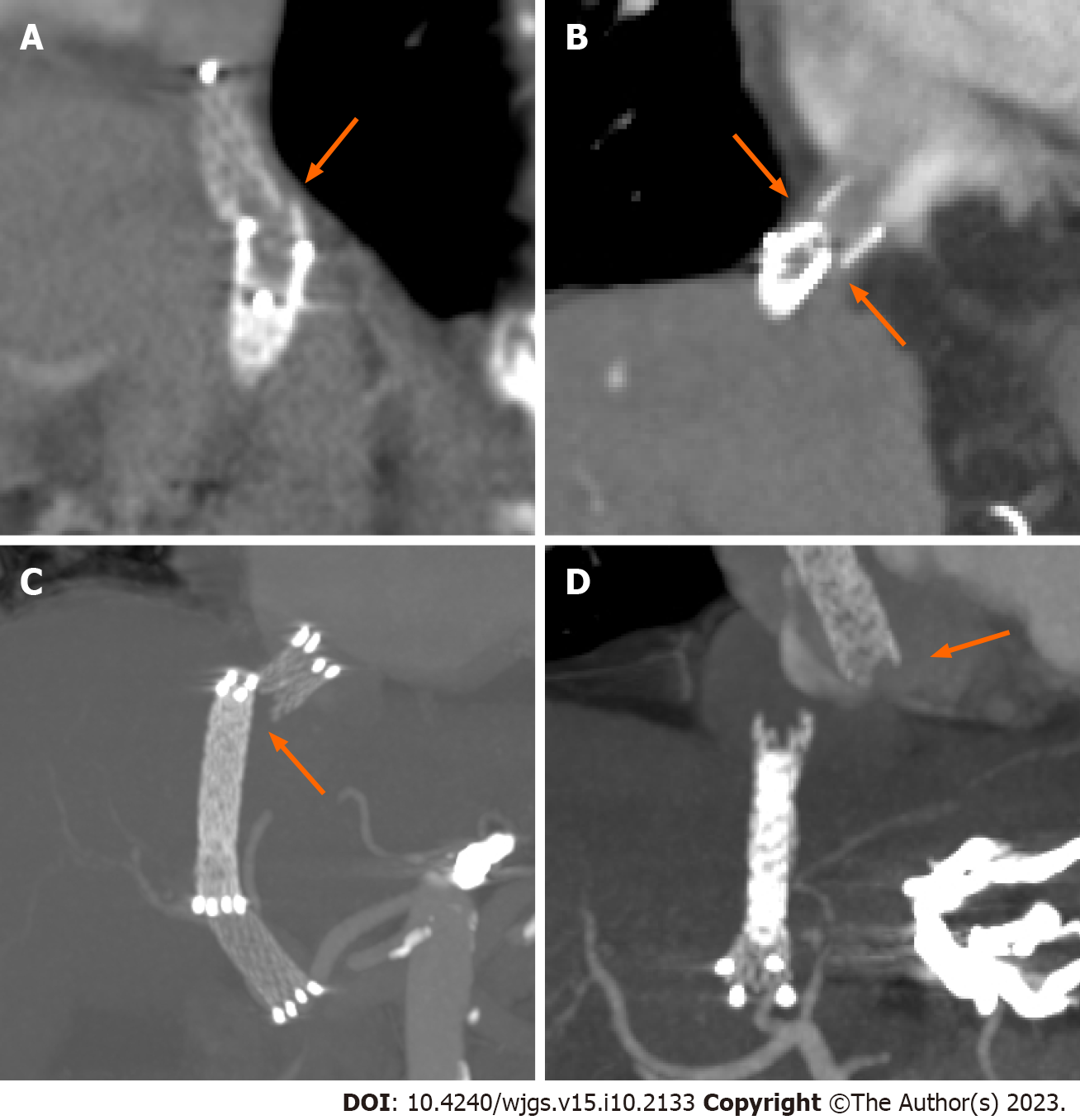
Follow-up CT revealed stent fractures in seven of 68 (10.3%) patients. The characteristics and outcomes of patients with stent fracture are summarized in Table 2. All stent fractures were located on the IVC side of the BMS. The median interval from TIPS construction to the detection of stent fracture was 512 d (range: 141-1, 406 d).
| Case | Age (yr) | Sex | Child-Pugh classification | Number of procedures | Fracture time (days after procedure) | Fracture type | Symptoms | Clinical outcome |
| 1 | 60 | Male | B | 1 | 159 | IIIb | None | Re-operation to implant a bare metal stent to connect the fractured stent |
| 2 | 63 | Female | A | 1 | 512 | I | Bleeding recurrence CT revealed shunt stenosis | Endoscopic hemostasis |
| 3 | 49 | Male | C | 2 | 675 | I | Bleeding recurrence CT revealed shunt stenosis | Re-operation using a bare metal stent to reconstruct the shunt |
| 4 | 70 | Female | A | 1 | 175 | I | None | Observation |
| 5 | 79 | Female | B | 1 | 141 | IIIa | None CT revealed shunt stenosis | Observation |
| 6 | 51 | Male | A | 1 | 1752 | I | None CT revealed shunt stenosis | Observation |
| 7 | 62 | Male | A | 2 | 1406 | II | None | Observation |
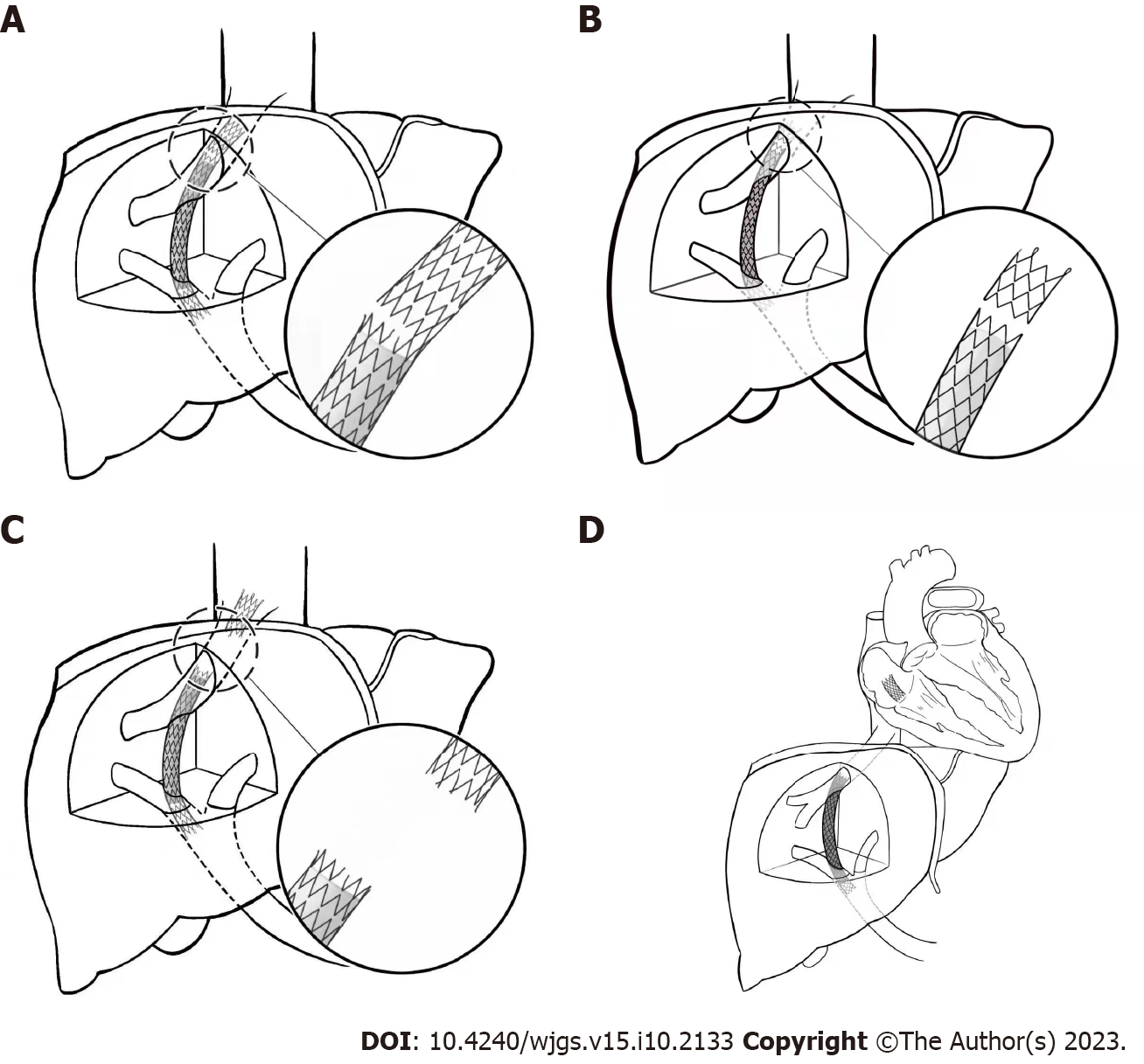
Based on follow-up CT images, the stent fractures were categorized into three types (Figure 2). Type I was defined as a partial fracture of the stent struts. Type II was defined as an annular fracture of the stent struts, resulting in stent transection without structural displacement of the stent. Type III was defined as stent transection with displacement of the fractured stent. Type III stent fractures were further categorized as type IIIa fractures with a small amount of displacement so that the fractured stent was still located in the original vascular structure (i.e., the hepatic vein or IVC) or type IIIb fractures with the fractured stent displaced out of the original vessel into adjacent structures (i.e., the superior vena cava or cardiac chamber). In the present study cohort, there were four (57.1%) type I fractures, one (14.3%) type II fracture, one (14.3%) type IIIa fracture, and one (14.3%) type IIIb fracture. All stent fractures were located at the junction of the BMS and the stent graft in the direction of the IVC (Figure 3).
After adjusting for relevant covariates (i.e., stent number, reoperation, and stent angle) in a multivariable logistic regression model, stent fractures were associated with the number of deployed stents [aOR = 22.2, 95% confidence interval (CI): 1.2-415.4, P = 0.038] and the size of angle 2 (aOR = 1.1, 95%CI: 1.0-1.3, P = 0.020) (Table 3).
The goal of TIPS placement is to relieve portal hypertension by establishing an artificial shunt between the PV and the systemic circulation. Because the Viatorr® stent (W. L. Gore and Associates, Flagstaff, AZ, United States) is not available in all hospitals in China, the BMS/stent-graft combination technique is still popular for TIPS construction. The BMS/stent-graft combination technique was designed to preserve the shunted portal branch blood flow and hepatic venous flow by using a BMS; this combination technique results in a lower risk of venous thrombosis compared with the single stent-graft technique. The BMS/stent-graft combination technique also enables the shunt flow and portal pressure to be adjusted precisely owing to the variation in the caliber of the stents. Compared with the single stent-graft procedure, the BMS/stent-graft combination technique is advantageous in that it protects liver function and has similar stent patency and hepatic encephalopathy rates[2]. However, although rare, stent fractures after TIPS placement can occur, which could decrease the stent patency rate or even cause severe consequences due to displacement of the fractured stent.
To the best of our knowledge, this is the first study to investigate the potential reasons for stent fracture after the TIPS procedure. The incidence of stent fracture was 10.3% during a median follow-up of 421 d. Based on the imaging features, we proposed a classification system and categorized stent fractures into three types. In our case series, type I fractures (57.1%) were the most common, followed by type III fractures (14.3% type IIIa and 14.3% type IIIb) and type II fractures (14.3%). This suggests that stent fracture occurred abruptly rather than progressively. That is, partial or complete circular fracture of the stent struts may decrease the local stress on the stent, which may relieve the external force that promotes the further development of stent fracture.
The predictive factors of stent fracture were the number of implanted stents and the stent bending angle at the IVC end. For every additional stent placed, the risk of stent fracture increased by 740%; for every additional angle of 2, the risk of stent fracture increased by 10%.
All stent fractures occurred at the IVC end at the junction of the stent graft and the BMS, and all fractured stents were BMSs. These findings are consistent with previously reported cases of stent fracture. The cause of stent fracture after the TIPS procedure was first reported in 2014 by Zabicki et al[4], who proposed that the main reason for stent fracture is an abnormal shunt shape caused by unique liver anatomy. Ding et al[5] reported that the fractured stents in their study did not have an excessive bending angle and speculated that stent fracture is caused by continuous tension generated at the proximal end of the overlapping part as a result of the motion at the junction of the trailing end of the stents. Komaki et al[6] suggested that stent fracture is related to the stent material and design. All the fractured stents reported in previous studies are open-loop self-expanding nickel-titanium alloy bare stents, which are the same as the fractured stents in our case series. We also found that the number of implanted stents and stent bending angle at the proximal end were predictors of stent fracture.
Our results showed that the risk of stent fracture significantly increased as the number of implanted stents increased. This may be related to the impacts of respiratory and cardiac motions on the tension of the stent at the IVC end. When using the BMS/stent-graft combination technique, as the number of implanted stents increases, the stress distributed on the stent becomes much more uneven, and the junction of the combined stents is more likely to become a fulcrum. The resultant increased tension on the overlapping part may result in stent fracture. The Viatorr® stent graft was approved for use in China in 2015. However, as Viatorr® stent-grafts are not yet available in all hospitals in China, the BMS/stent-graft combination technique is still used in many Chinese medical centers. Compared with TIPS placement using the Viatorr® stent-graft, the greater number of implanted stents in TIPS placement using the BMS/stent-graft combination technique might result in an increased incidence of stent fractures because of the uneven distribution of stent stress. To reduce the risk of stent fracture, we proposed the following technical modifications for the BMS/stent-graft combination technique.
First, surgeons should adjust the overlapping strategy of the BMS/stent-graft combination technique. To avoid excessive local tension on the BMS, it should be fully covered by the stent graft at the IVC end of the shunt to ensure that stress is uniformly distributed on the stents. In addition, the overlapping stents can increase the longitudinal supporting force, which can decrease the bending angle of the IVC end of the stent and reduce its risk of fracture. If possible, the shunt should be established using a closed-loop stent, which may relieve the uneven stress distribution.
Second, TIPS construction should be performed using a more precise positioning approach, such as anterior-posterior and lateral angiography. This may help prevent the proximal end of the stent from protruding excessively into the IVC, thereby reducing the stress on the stent caused by respiratory and cardiac motions.
Third, as excessive bending of the proximal end of the stent may result in stent fracture, the starting puncture point in the hepatic vein should be as close as possible to the IVC. Finally, the development of stents with better conformability and appropriate structure may help to avoid stent fractures.
This was a retrospective study of the clinical data of small sample of patients treated in one medical center. Large-scale prospective studies are needed to explore the exact mechanism and risk factors for stent fracture after TIPS placement using the BMS/stent-graft combination technique.
The widely used BMS/stent-graft combination technique for TIPS construction in China has an incidence of stent fractures of approximately 10%. All the stent fractures occurred at the junction of the BMS and the proximal end of the stent graft. Stent fractures may be associated with the number of stents implanted and excessive bending of the stent. To avoid stent fracture, we recommend a greater overlap of the stent graft with the BMS at the IVC end of the shunt and the selection of a position closer to the opening of the hepatic vein into the IVC as the starting puncture site to establish a shunt.
Transjugular intrahepatic portosystemic shunt (TIPS) placement is widely used to treat portal hypertension. In China, TIPSs are frequently constructed using the bare metal stent (BMS)/stent-graft combination technique.
Stent fracture is a rare complication after TIPS placement using the BMS/stent-graft combination technique and stent fracture may cause severe consequences.
To assess the incidence of stent fracture after TIPS placement using the BMS/stent-graft combination technique and identify the risk factors for stent fracture.
Retrospective cohort study.
Of the 68 included patients, stent fracture occurred in seven (10.3%) patients. The risk factors for stent fracture were the implantation of a greater number of stents [adjusted odds ratio (aOR) = 22.2, 95% confidence interval (CI): 1.2-415.4, P = 0.038] and a larger proximal sagittal stent bending angle (aOR = 1.1, 95%CI: 1.0-1.3, P = 0.020).
We found three types of stent fracture occurred in 10.3% of the sample patients. The number of implanted stents and the stent bending angle at the inferior vena cava end were the independent risk factor of stent fracture.
Our results suggested that the incidence of stent fracture could potentially be reduced by procedural modifications.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Goenka MK, India; Gupta T, India; Ueda H, Japan; van Leeuwen DJ, United States S-Editor: Qu XL L-Editor: A P-Editor: Yuan YY
| 1. | Patidar KR, Sydnor M, Sanyal AJ. Transjugular intrahepatic portosystemic shunt. Clin Liver Dis. 2014;18:853-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Wang CM, Li X, Fu J, Luan JY, Li TR, Zhao J, Dong GX. Construction of Transjugular Intrahepatic Portosystemic Shunt: Bare Metal Stent/Stent-graft Combination versus Single Stent-graft, a Prospective Randomized Controlled Study with Long-term Patency and Clinical Analysis. Chin Med J (Engl). 2016;129:1261-1267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Wang CM, Li X, Fu J, Luan JY, Li TR, Zhao J, Dong GX. Technological modification of transjugular intrahepatic portosystemic shunt: the precise covering of parenchymal shunt with stent-graft. Beijing Da Xue Xue Bao Yi Xue Ban. 2014;46:165-168. [PubMed] |
| 4. | Zabicki B, Ricke J, Dudeck O, Pech M. CT-assisted transfemoral intrahepatic portosystemic shunt in a long duration follow-up: A case report. Pol J Radiol. 2014;79:39-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Ding PX, Han XW, Hua ZH, Liu C. Stent Fracture and Fragment Migration to Chordae Tendineae of the Tricuspid Valve after Transjugular Intrahepatic Portosystemic Shunt Procedure. J Vasc Interv Radiol. 2017;28:1293-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Komaki T, Hiraki T, Uka M, Fujiwara H, Iguchi T, Kanazawa S. A Case of Stent Fracture After Transjugular Intrahepatic Portosystemic Shunt. Cardiovasc Intervent Radiol. 2018;41:976-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Guo S, Tang S. Stent fracture after transjugular intrahepatic portosystemic shunt:a case report and literature review. Zhongguo Yike Daxue Xuebao. 2020;49:379-381. [DOI] [Full Text] |
| 8. | Xiong F, Tan K, Cheng L, Luo Y, Zhao Z. A rare case of severe tricuspid regurgitation caused by detached stent falling into the right ventricle after transjugular intrahepatic portosystemic shunt. J Cardiothorac Surg. 2022;17:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Shetty K, Rybicki L, Carey WD. The Child-Pugh classification as a prognostic indicator for survival in primary sclerosing cholangitis. Hepatology. 1997;25:1049-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 74] [Article Influence: 2.6] [Reference Citation Analysis (0)] |