Published online Apr 27, 2022. doi: 10.4240/wjgs.v14.i4.271
Peer-review started: November 17, 2021
First decision: December 27, 2021
Revised: December 28, 2021
Accepted: April 4, 2022
Article in press: April 4, 2022
Published online: April 27, 2022
Processing time: 157 Days and 20.8 Hours
The main purpose of a radiologist’s expertise in evaluation of anal fistula magnetic resonance imaging (MRI) is to benefit patients by decreasing the incontinence rate and increasing the healing rate. Any loss of vital information during the transfer of this data from the radiologist to the operating surgeon is unwarranted and is best prevented. In this regard, two methods are suggested. First, a short video to be attached with the standardized written report high
Core Tip: There is loss of vital information when a fistula-in-ano magnetic resonance imaging (MRI) report from the radiologist is interpreted by the operating surgeon. To prevent this loss, a novel method is suggested: sending a small video highlighting vital fistula parameters along with the written MRI report. Also, another vital parameter is the amount of external sphincter involvement by the fistula. This parameter is not included in the MRI report and can be evaluated from the height of penetration of the external anal sphincter (HOPE) by the fistula. This parameter (HOPE) is distinct from the ‘height of internal opening’ and would help prevent damage to the external anal sphincter during surgery.
- Citation: Garg P, Kaur B, Yagnik VD, Dawka S. Including video and novel parameter-height of penetration of external anal sphincter-in magnetic resonance imaging reporting of anal fistula. World J Gastrointest Surg 2022; 14(4): 271-275
- URL: https://www.wjgnet.com/1948-9366/full/v14/i4/271.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i4.271
Anal fistulas are associated with a high rate of recurrence and risk to the anal continence mechanism. The operating surgeons need to understand the exact position of the anal fistula and its relation to the anatomical structures in order to achieve high cure rate especially in complex anal fistulas. Magnetic resonance imaging (MRI) is the gold standard investigation used for anal fistulas. Usually, the MRI is interpreted by the radiologists who then send a written report to the operating surgeon and the surgeon performs the surgery after reading the radiologist’s report. Formats have been suggested for reporting the MRI in fistulas[1,2]. However, utility of MRI to the operating surgeon can be improved immensely if the two features discussed below (inclusion of an MRI video and addition of HOPE parameter) are added to MRI report (Table 1).
| Parameters | Example |
| Primary tract | The primary fistula tract |
| External opening | Is opening in perianal skin at 7 o’clock position |
| Course and location | It extends superiorly in right ischiorectal fossa from 7 to 8 o’clock position |
| Length | For a length of 6.35 cm |
| Location and height of penetration of EAS (HOPE) | and penetrates the EAS at 8 o’clock position involving approximately two-thirds of the EAS. It then bends inferiorly and |
| Intersphincteric tract | follows an intersphincteric route from 8 to 6 o’clock |
| Location and height Internal opening | and opens in the anal canal at the level of dentate line |
| Secondary extension- intersphincteric/ ischiorectal fossa/supralevator | There are no secondary extensions of primary tract |
| Secondary tract | There are no secondary tracts, |
| External opening | |
| Course and location | |
| Associated abscess | No associated abscess |
| Supralevator or suprasphincteric tract | And supralevator tract |
| Sphincter anatomy | The sphincters look normally preserved |
| Classification | Parks grade -II, SJUH1 grade III |
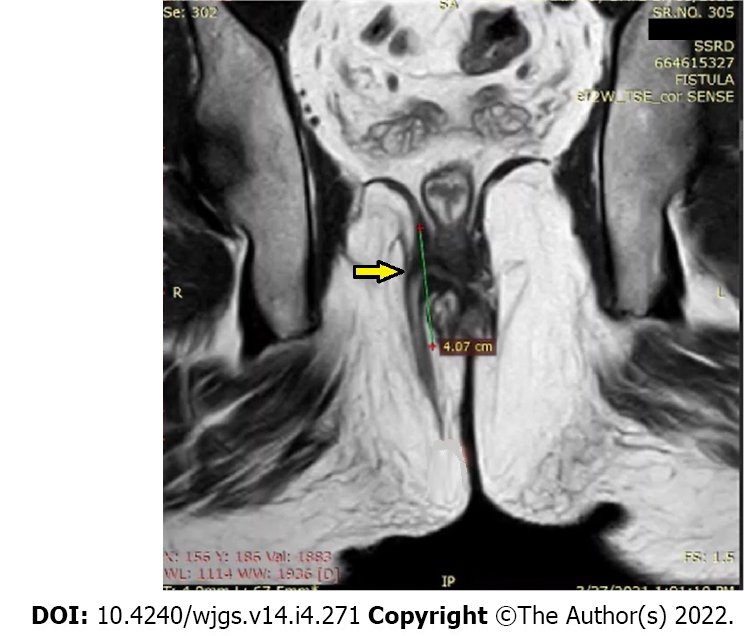
First, when only a written report is sent by the radiologist who has analyzed the MRI scans, then a lot of important information is lost. This happens because the three-dimensional picture created in the radiologist’s mind by the detailed visual analysis of the MRI scans cannot be replicated in the surgeon’s mind just by reading the text in the radiologist’s report. This loss of three-dimensional visual data can be prevented by sending a small video highlighting all relevant parameters along with the written report. Second, as discussed, the two main concerns in anal fistulas are recurrence and incontinence[3]. It is a known fact that the recurrence risk of fistula is directly related to surgeon’s knowledge about the precise location of fistula tract’s internal opening (where the fistula opens into the anal canal)[4,5]. On the other hand, the accurate assessment of the amount of external anal sphincter (EAS) involvement is key to prevent sphincter damage (incontinence)[6]. The importance of reporting the location of the internal opening has now been established[7], but the other equally important parameter, HOPE (height of penetration of external anal sphincter by the fistula) parameter is not reported by the radiologists (Figure 1). The EAS is mainly responsible for anal continence. HOPE parameter conveys the extent of involvement of the EAS to the operating surgeon and is thus pivotal to avoid damaging the EAS. The studies have demonstrated that when the surgeon performing the surgery is unsure of the accurate extent of EAS involvement, then the fistulotomy procedure is generally avoided and remains largely underutilized, even in simple anal fistulas, due to fear of incontinence in the mind of surgeons[8]. Fistulotomy is the simplest procedure for low anal fistulas and is associated with the maximum cure rate (93%-99%) and no other procedure has been shown to have success rate comparable to fistulotomy[6,8]. Therefore, lack of knowledge of HOPE (EAS involvement) leads to a lower healing rate which can be prevented by proper MRI reporting.
As the origin of most fistulas is at the level of the dentate line, the location of the internal opening in most of them is at that level only. The location of the internal opening does not accurately correspond to the amount of involvement of the EAS as penetration of the EAS by the fistula is often at a different level (Figure 1 and Video 1). Therefore, HOPE is the parameter which should be reported separately for helping the operating surgeon to precisely assess the amount of involvement of the EAS.
The level of understanding of fistula anatomy is greatly enhanced in the surgeon’s mind when a small video of MRI scan showing the fistula characteristics is send along with the written report (Video 1). The key points regarding the fistula characteristics can be highlighted by using a pointer in the video (Video 1). The fistula parameters which should be mentioned and highlighted in the video have been listed in Table 2. The MRI report should also be standardized as shown in Table 1. An example of a final written report (of the fistula shown in Video 1 has been included at the bottom of Table 1 to clarify the format).
| Axial Section T2-weighted |
| 1 External opening- location |
| 2 Define primary tracts |
| Location and course – Ischiorectal fossa/ Intersphincteric and clock-dial position |
| Location and ‘height’ of penetration of external anal sphincter (HOPE)- Point of penetration of external anal sphincter |
| Intersphincteric course |
| Location and height of internal opening- clock-dial position and whether it is at dentate line or higher |
| 3 Secondary tracts |
| 4 Associated abscesses |
| 5 Supralevator extension |
| 6 Additional internal opening |
| 7 Sphincter anatomy |
| Axial section-STIR |
| 1 Confirm findings of Axial-T2 |
| 2 Additional areas with inflammation |
| Coronal T2-weighted |
| 1 Confirm findings of Axial-T2 |
| 2 Length of tract |
| 3 Supralevator or suprasphincteric tract |
| 4 Confirm the ‘height’ of penetration of external anal sphincter (HOPE) by the fistula tract – Indicates the amount of external sphincter involved |
| 5 Confirm the ‘height’ of the site of internal opening |
| 6 Extent of fistula tract in anterior fistulas- relation with urethra |
| 7 Sphincter anatomy |
| Coronal section- STIR |
| 1 Confirm findings of Coronal-T2 |
| 2 Good to detect thin Intersphincteric collections |
| Biplanar (Axial T-2 weighted + Coronal T-2 weighted) |
| 1 Confirm the ‘height’ of the site of penetration of external sphincter by the fistula tract – Indicates the amount of external sphincter involved |
| 2 Confirm the ‘height’ of the site of internal opening |
| Sagittal section |
| 1 Extent of fistula tract in posterior fistulas- Relation with sacrococcygeal spine, presacral space |
| 2 Extent of fistula tract in anterior fistulas- Relation with urethra |
As can be seen, the novel parameter reported in this study, HOPE (height of penetration of external anal sphincter by the fistula tract) has also been incorporated in the video (Video 1) as well as the report format (Table 1) (Figure 1). This parameter (HOPE) conveys the amount of EAS involved by the fistula tract (Figure 1).
The study concept was reviewed and approved by the Hospital-Institute Ethics Committee.
This paper describes two novel additions to the MRI reporting of anal fistulas. The first is inclusion of a video along with the standardized written report (Tables 1 and 2, Video 1). This would prevent loss of vital three-dimensional data about the disease when the information is being transferred from the radiologist to the operating surgeon and would significantly enhance the surgeon’s understanding of the fistula anatomy. Second, when the HOPE parameter (height of penetration of external anal sphincter by the fistula) is incorporated in the video as well as written report, the risk of EAS damage would be drastically reduced and the success rate of the surgical procedure would also be enhanced. Therefore, HOPE should be reported as a separate parameter apart from the location of the internal opening. This format of MRI reporting (including a video) can also be stored on PACS (picture archiving and communication system)[9,10]. PACS provide storage and convenient access to medical images from where the clinician can see the report, images as well as the video as per their convenience[9,10].
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Society of Colon Rectum Surgeons; American Society of Gastrointestinal Endoscopic Surgeons; Endoscopic and Laparoscopic Surgeons of Asia; Association of Surgeons of India.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ankrah AO, Netherlands; Ma C, China S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Tuncyurek O, Garces-Descovich A, Jaramillo-Cardoso A, Durán EE, Cataldo TE, Poylin VY, Gómez SF, Cabrera AM, Hegazi T, Beker K, Mortele KJ. Structured vs narrative reporting of pelvic MRI in perianal fistulizing disease: impact on clarity, completeness, and surgical planning. Abdom Radiol (NY). 2019;44:811-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Ho E, Rickard MJFX, Suen M, Keshava A, Kwik C, Ong YY, Yang J. Perianal sepsis: surgical perspective and practical MRI reporting for radiologists. Abdom Radiol (NY). 2019;44:1744-1755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Włodarczyk M, Włodarczyk J, Sobolewska-Włodarczyk A, Trzciński R, Dziki Ł, Fichna J. Current concepts in the pathogenesis of cryptoglandular perianal fistula. J Int Med Res. 2021;49:300060520986669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 4. | Mei Z, Wang Q, Zhang Y, Liu P, Ge M, Du P, Yang W, He Y. Risk Factors for Recurrence after anal fistula surgery: A meta-analysis. Int J Surg. 2019;69:153-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 100] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 5. | Sygut A, Mik M, Trzcinski R, Dziki A. How the location of the internal opening of anal fistulas affect the treatment results of primary transsphincteric fistulas. Langenbecks Arch Surg. 2010;395:1055-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 6. | Garg P, Kaur B, Goyal A, Yagnik VD, Dawka S, Menon GR. Lessons learned from an audit of 1250 anal fistula patients operated at a single center: A retrospective review. World J Gastrointest Surg. 2021;13:340-354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (3)] |
| 7. | Halligan S, Tolan D, Amitai MM, Hoeffel C, Kim SH, Maccioni F, Morrin MM, Mortele KJ, Rafaelsen SR, Rimola J, Schmidt S, Stoker J, Yang J. ESGAR consensus statement on the imaging of fistula-in-ano and other causes of anal sepsis. Eur Radiol. 2020;30:4734-4740. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Garg P. Is fistulotomy still the gold standard in present era and is it highly underutilized? Int J Surg. 2018;56:26-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 9. | Glazer DI, Zhao AH, Lacson R, Burk KS, DiPiro PJ, Kapoor N, Khorasani R. Use of a PACS Embedded System for Communicating Radiologist to Technologist Learning Opportunities and Patient Callbacks. Curr Probl Diagn Radiol. 2021;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Huang HK. Medical imaging, PACS, and imaging informatics: retrospective. Radiol Phys Technol. 2014;7:5-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |