Published online Dec 27, 2022. doi: 10.4240/wjgs.v14.i12.1425
Peer-review started: August 19, 2022
First decision: September 4, 2022
Revised: September 17, 2022
Accepted: October 25, 2022
Article in press: October 25, 2022
Published online: December 27, 2022
Processing time: 129 Days and 21.6 Hours
Tailgut cyst is a congenital enterogenous cyst that rarely undergoes malignant transformation. Its clinical manifestations mainly correlate to the mass effect caused by the development of cysts and the infections that originate from these. Furthermore, the complete resection of this cyst is curative. We report our diagnostic and treatment experience with one case of malignant transformation of a perianal tailgut cyst, which was initially misdiagnosed as perianal abscess.
A 72-year-old woman visited our institution with complaints of a refractory nonhealing lesion on the right hip, which repeatedly broke and suppurated for more than 70 years, and aggravated in 4 mo. The patient was given a diagnosis of refractory perianal abscess with repeated incision and drainage procedures. Computed tomography of the pelvic cavity revealed a giant perianal cyst. Subsequent biopsy revealed a tumor with moderate-to-severe glandular epithelial dysplasia, and suggested that this was derived from the developmental cysts in the posterior rectal space. After further clarifying the nature and extent of the tumor by magnetic resonance imaging, total cystic resection was performed. Postoperative histopathological examination confirmed the malignancy, dictating the investigators to add postoperative chemotherapy to the treatment regimen.
The malignant transformation of perianal tailgut cysts is very uncommon, and this should be differentiated from perianal abscess. Complete surgical removal is curative, and postoperative pathology may determine the necessity of additional postoperative chemotherapy or radiotherapy, which may be beneficial for preventing local recurrence and metastasis.
Core Tip: We report our diagnostic and treatment experience with a unique case of malignant transformation of perianal tailgut cyst. Since perianal tailgut cysts are difficult to differentiate from other perianal diseases, the reported case was initially misdiagnosed as perianal abscess with repeated incision and drainage procedures. The patient underwent complete resection and received salvage chemotherapy for 3 mo after the surgery.
- Citation: Fang Y, Zhu Y, Liu WZ, Zhang XQ, Zhang Y, Wang K. Malignant transformation of perianal tailgut cyst: A case report. World J Gastrointest Surg 2022; 14(12): 1425-1431
- URL: https://www.wjgnet.com/1948-9366/full/v14/i12/1425.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i12.1425
Tailgut cysts are developmental congenital enterogenous cysts that mostly occur in the retrorectal or presacral space[1]. The clinical features include the mass effect caused by the development of cysts, and the infection that originates from these[2]. Magnetic resonance imaging (MRI) can display the typical cyst appearance, which is crucial for distinguishing the cyst from perianal abscess. Complete resection of the cyst is curative and clinically preferred[3]. Postoperative histopathological analysis is routinely performed to pathologically confirm the diagnosis and mainly rule out the chance of malignancy. Clinically, this entity is not complicated in its diagnosis and treatment. We report a case of malignant transformation after the perianal tailgut cyst was misdiagnosed as perianal abscess, in which total resection was performed and postoperative chemotherapy was added.
A 72-year-old woman was transferred to our hospital with complaints of a tumor on the right hip, which repeatedly broke and suppurated for more than 70 years, and aggravated in 4 mo.
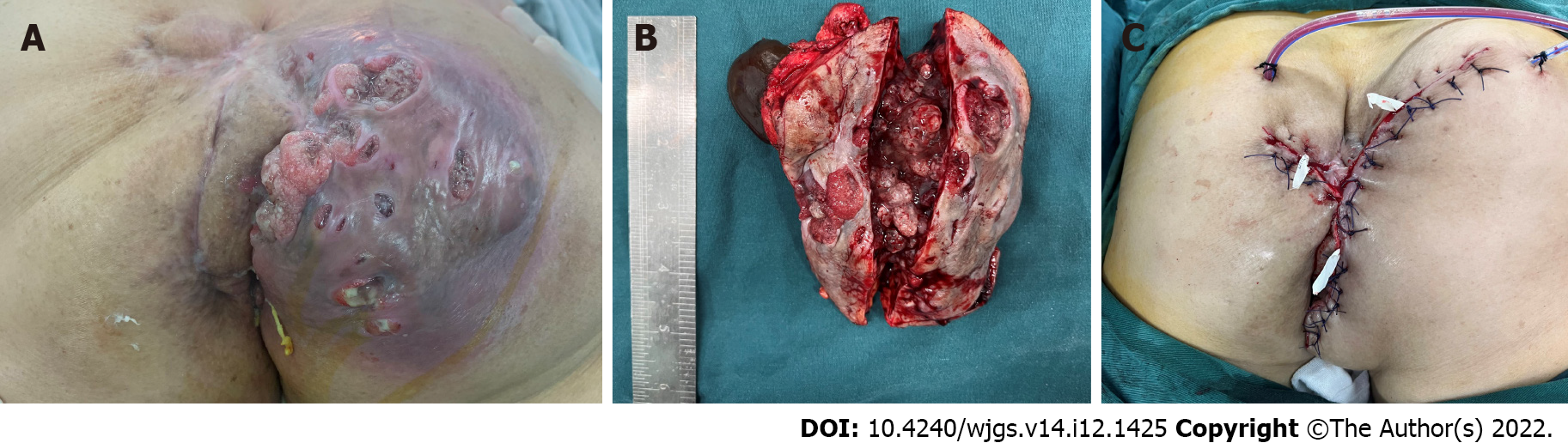
The patient was born with a 5 mm × 5 mm mass under the right hip, which covered the skin. Perianal distending pain and discomfort were experienced by the patient with the gradual increase of the tumor. At a local hospital, the patient was diagnosed with perianal abscess due to its fluctuating feature. During the incision and drainage procedures, copious brownish pus was repeatedly drained out from the mass. In particular, during the recent 4 mo, the mass progressively become larger, with multiple ulcers on its surface, cauliflower-like objects at its base, and jelly-like liquid inside.
The patient had a history of hypertension, and her daily blood pressure was maintained at approximately 120/60 mmHg with regular oral medication.
The patient denied any family history of malignancy.
The physical examination did not unveil any significant finding, except for the 5 cm ulcerative mass under the right hip.
The patient had a slightly elevated carbohydrate antigen 7-24 of 23.04 U/mL, but no abnormalities were detected in other blood and urine analyses.
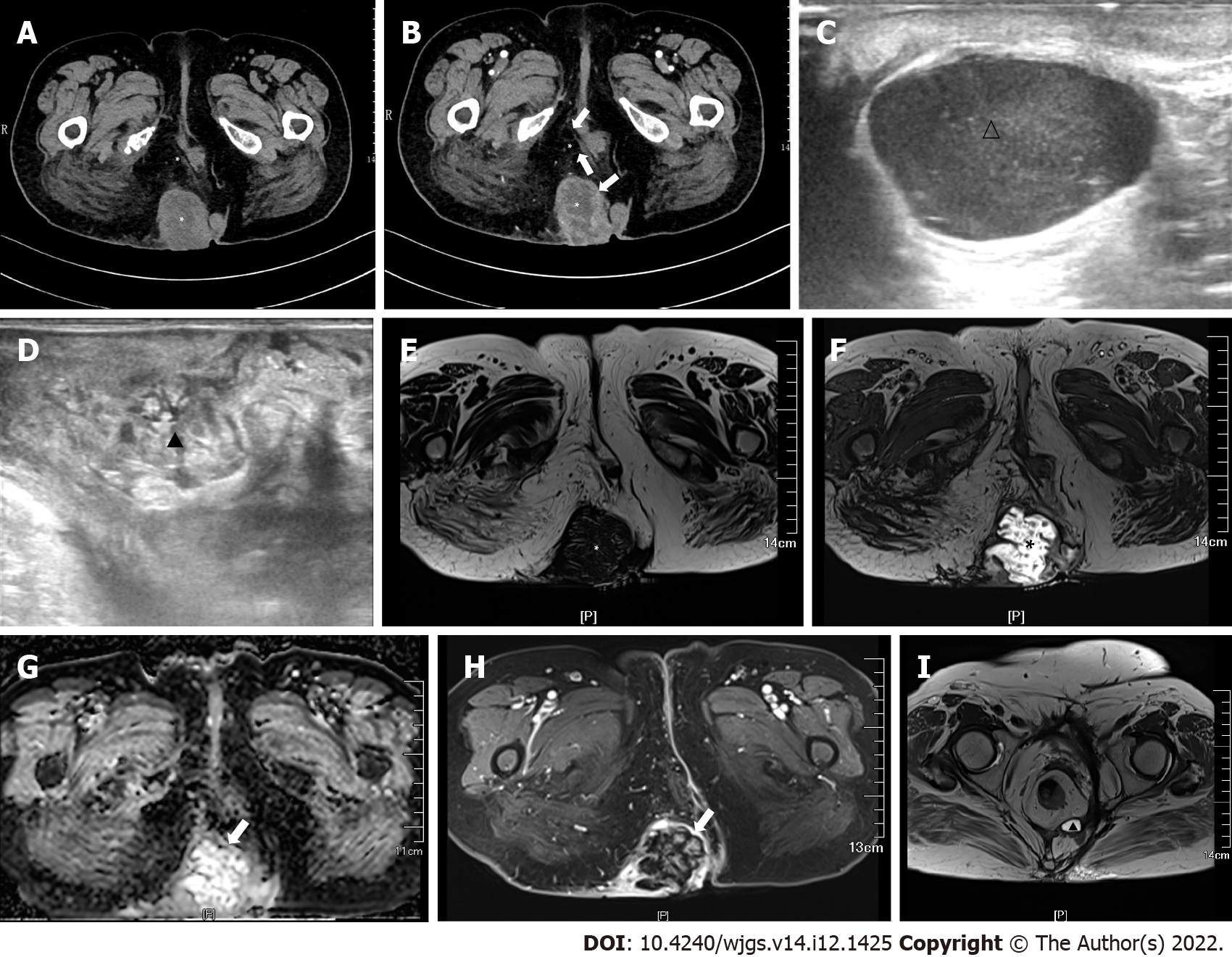
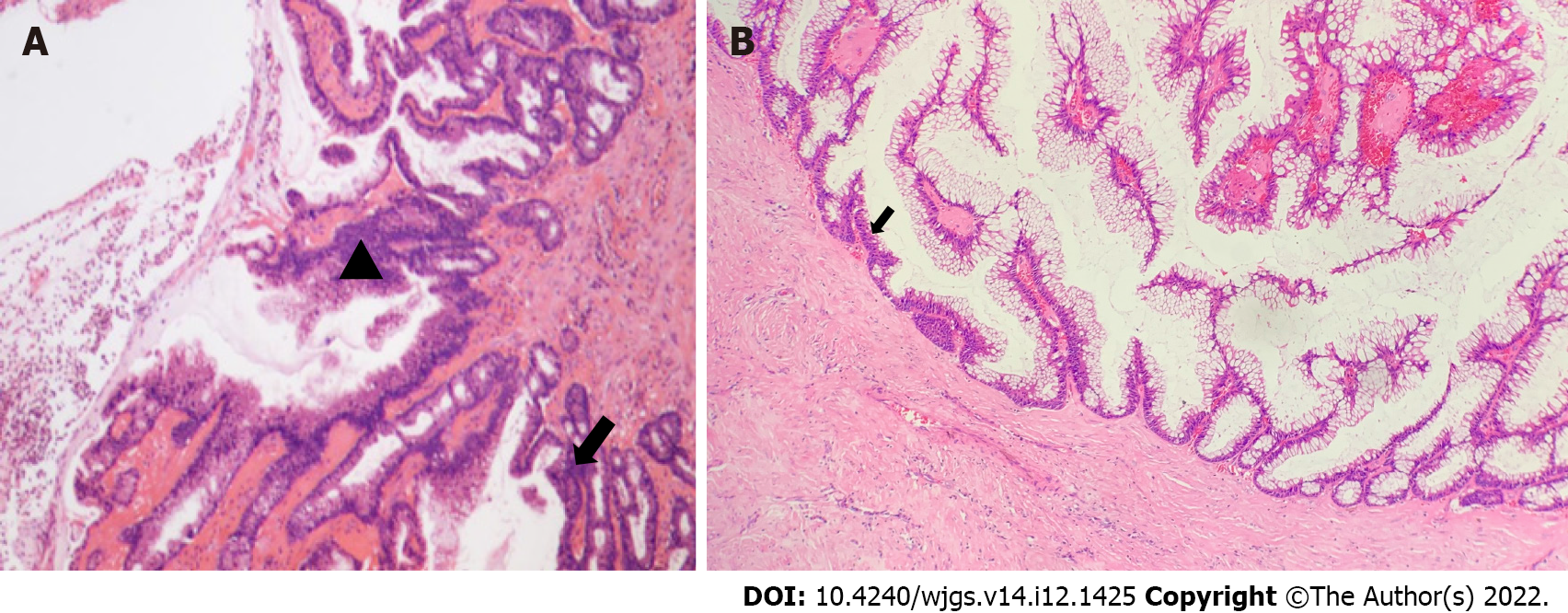
Computed tomography (CT) revealed a multilocular cystic soft tissue mass in the right hip, which extended into the sacrococcygeal region, with an enhanced edge and a size of 6.0 cm × 5.8 cm × 9.5 cm (Figure 1A and B). In order to establish a diagnosis, biopsy was performed on the cystic mass. The results revealed a tumor with moderate-to-severe glandular epithelial dysplasia, and suggested the origin of developmental cysts in the posterior rectal space (Figure 2A). After the patient was transferred to our hospital, intestinal lesions were further excluded by proctoscopy. Endorectal ultrasonography further revealed multiple hypoechoic areas (diameter: 1.0-2.5 cm), with clear boundaries in the sacrococcygeal region, and uneven echo areas in the right hip with unclear boundaries (Figure 1C and D). MRI revealed an abnormal hypointense T1 and hyperintense T2 signal shadow in irregular quasi-circular lesion, and diffusion-weighted imaging (DWI) revealed a size of 107 mm in the sagittal position with wall enhancement (Figure 1E-H).
Through the discussion of the multidisciplinary team, enterogenous cyst with malignant transformation was suggested as the preliminary diagnosis. The patient underwent a transperineal operation, during which the tailgut cyst was identified to extend into the posterior rectal space, and reach the sacral vertebrae at the 4th-5th levels above the tip of the coccyx. Since the sacrococcyx fascia was considered to be the origin of the cyst and attached to the coccyx, a part of this was resected to expose the surgical field. After radically resecting the cystic lesion with the surrounding tissues without injuring the posterior rectal wall, endorectal ultrasonography was performed to confirm that no cystic remnants were present, and a free-flap procedure to reconstruct the extensive resection site was performed by co-operating with the plastic surgery team (Figure 3). The operation lasted for approximately 270 min, with an unexpected intraoperative blood loss of more than 600 mL. The patient was hospitalized for 36 d for postoperative recovery.
Postoperatively, pathological examination revealed a diagnosis of malignant transformation of the perianal tailgut cyst, and this was identified as mucinous adenocarcinoma, with a size of 6.5 cm × 4.0 cm × 6.0 cm, without local infiltration (Figure 2B). Histologically, tumorous cells were found 0.2 cm away from the resection margin, confirming a pathological R0 resection. Further immune-histological examinations were paneled, as follows: MLH1 (+), MSH2 (+), MSH6 (+), PMS2 (+), P53S100 (-), CD34 (-), D2-40 (-), Ki-67 (70%), CDH-17 (+), CDX-2 (+), CK7 (+), CK20 (+), and SATB-2 (+).
Pathologically, the patient was given a final diagnosis of malignant transformation of the perianal tailgut cyst.
Three months after the surgery, MRI revealed a small cyst under the right levator ani (Figure 1I), and the carbohydrate antigen 7-24 decreased to normal. According to the postoperative pathology, oral salvage chemotherapy with capecitabine 1000 mg, twice per day, for eight cycles, was added, and an MRI examination was recommend every 3 mo to monitor the change in size of the cyst.
After the 3rd cycle of chemotherapy with capecitabin, the patient did not have any special complaints or discomfort.
As a rare congenital disease, tailgut cyst originates from the tailgut and neurenteric canal[4], and most likely occurs in the retrorectal or presacral space[1]. Clinically, this disease is more commonly observed in middle-aged females with the presentation of a mass lesion, with or without infection[2]. Malignancy infrequently occurs in presacral tailgut cysts, at a rate of less than 8%, and when this occurs, it may most likely be adenocarcinoma or carcinoid[3]. For the present case, the patient presented with an infected and inflammatory mass, with the dissemination of cells from the cyst wall as the result of repeated incision, and this might have been the main cause of the local recurrence that contributed to the malignant transformation[5].
The present report emphasizes the differentiation of a perianal tailgut cyst from a perianal abscess. For perianal abscess in the retrorectal space, when it exhibits the reluctance to complete healing due to the discharge of residual pus, when no anal fistula is found, or when this recurs multiple times after repeated surgical treatment, tailgut cyst should be suspected and completely resected for further pathological diagnosis. Since the specimens obtained from the biopsy often contain merely the inflamed fibrous tissue without the epithelia, or merely one type of epithelium, which may not consequently support any diagnosis[6], the biopsy of the cystic lesion is not recommended.
Pathohistologically, the cyst would be filled with brown and jelly-like fluid from the wall of the tailgut cyst[6], which would be partially or completely covered with intestinal epithelium, and this may contain columnar cells, squamous cells, and transitional cells with mucus secretion function[2], while the smooth muscle fibers in the cyst wall would be disorganized without the nerve plexus[7]. The canceration of caudal cysts is mostly focal, allowing for a thorough postoperative histopathological analysis of the resected specimen to be mandated, in order to confirm the diagnosis and rule out malignant tumors. Unlike perianal abscesses, tailgut cysts possess a multilocular nature, which demands preoperative endorectal ultrasonography, or pelvic MRI or CT imaging studies[8]. MRI can reveal the typical cyst appearance as low attenuation on T1 and high-attenuation on T2, and DWI can allow for the tailgut cyst to be distinguished from a perianal abscess[9]. Furthermore, although the importance of MRI in the diagnosis of tailgut cysts has been emphasized, endorectal ultrasonography is more convenient and accessible than MRI, especially in operations for complete cyst resection[10].
For the risk of malignant transformation of a cyst, surgical resection is the first choice for the treatment of tailgut cysts[3], and the surgical approach should be selected according to the location of the cyst shown in the imaging studies. Since the incidence of canceration of the tailgut cyst remains low, there is still a risk of local recurrence and distant metastasis. At present, three cases of local recurrence and two cases of distant metastasis have been reported[11-14]. Among these cases (Table 1), a patient with pseudomyxoma peritonei benefited from chemotherapy. After 3 mo, MRI revealed a small cyst under the right levator ani, which might putatively be correlated to the local implantation of cyst wall cells caused by the partial rupture of the cyst wall during the operation. Since the preoperative carbohydrate antigen 724 was also slightly elevated, with a Ki-67 index of 70%, oral capecitabine chemotherapy was given to the patient, who refused to undergo a reoperation for the relatively tiny lesion, as a salvage chemotherapy. In addition, close follow-up with MRI study was recommended. Indeed, a study suggested that postoperative adjuvant radiotherapy be recommended for patients with canceration of the tailgut cyst and remnant lesions for incomplete lesion resection, in order to achieve good outcomes, with or without chemotherapy[15].
| Ref. | Gender | Age (yr) | Pathology | Cause of chemotherapy | Scheme | Follow-up | PMID |
| Akira et al[14], 1998 | Female | 66 | Moderately differentiated adenocarcinoma | Elevated carcinoembryonic antigen level | Oral tegafur, 200 mg daily | 3.2 yr | 9872560 |
| Luis et al[13], 2009 | Female | 37 | Mucinous adenocarcinoma | Resection was complete, but not en bloc | Intraperitoneal mitomycin C and doxorubicin plus systemic 5-fluorouracil and leucovorin | 3.0 yr | 19856666 |
| Zhao et al[5], 2015 | Female | 44 | Moderately differentiated adenocarcinoma | Elevated carcinoembryonic antigen level | Intracapsular tumor necrosis factor and raltitrexed plus systemic oxaliplatin 3-cycles (130 mg/m2) | 9.0 wk | 26656372 |
In summary, perianal caudal cysts are difficult to differentiate from other perianal diseases, especially perianal abscesses. Due to the risk of cancerization of the cyst, multi-disciplinary treatment should be emphasized clinically.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Jiang Y, China; Piltcher-da-Silva R, Brazil; Tajiri K, Japan; Tangsuwanaruk T, Thailand; Tsujinaka S, Japan; S-Editor: Liu GL L-Editor: Wang TQ P-Editor: Liu GL
| 1. | Sung MT, Ko SF, Niu CK, Hsieh CS, Huang HY. Perirenal tailgut cyst (cystic hamartoma). J Pediatr Surg. 2003;38:1404-1406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Dahan H, Arrivé L, Wendum D, Docou le Pointe H, Djouhri H, Tubiana JM. Retrorectal developmental cysts in adults: clinical and radiologic-histopathologic review, differential diagnosis, and treatment. Radiographics. 2001;21:575-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 153] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Broccard SP, Colibaseanu DT, Behm KT, Mishra N, Davis P, Maimone KL, Mathis KL, Stocchi L, Dozois EJ, Merchea A. Risk of malignancy and outcomes of surgically resected presacral tailgut cysts: A current review of the Mayo Clinic experience. Colorectal Dis. 2022;24:422-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Hjermstad BM, Helwig EB. Tailgut cysts. Report of 53 cases. Am J Clin Pathol. 1988;89:139-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 193] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 5. | Zhao XR, Gao C, Zhang Y, Yu YH. The Malignant Transformation of Retrorectal Cystic Hamartomas With Blood Irregular Antibodies Positive: A Case Report. Medicine (Baltimore). 2015;94:e2253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Prasad AR, Amin MB, Randolph TL, Lee CS, Ma CK. Retrorectal cystic hamartoma: report of 5 cases with malignancy arising in 2. Arch Pathol Lab Med. 2000;124:725-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 92] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Hufkens AS, Cools P, Leyman P. Tailgut cyst: report of three cases and review of the literature. Acta Chir Belg. 2019;119:110-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Li Z, Lu M. Presacral Tumor: Insights From a Decade's Experience of This Rare and Diverse Disease. Front Oncol. 2021;11:639028. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Shetty AS, Loch R, Yoo N, Mellnick V, Fowler K, Narra V. Imaging of tailgut cysts. Abdom Imaging. 2015;40:2783-2795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Visscher AP, Felt-Bersma RJ. Endoanal ultrasound in perianal fistulae and abscesses. Ultrasound Q. 2015;31:130-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Liessi G, Cesari S, Pavanello M, Butini R. Tailgut cysts: CT and MR findings. Abdom Imaging. 1995;20:256-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Erdrich J, Schaberg KB, Khodadoust MS, Zhou L, Shelton AA, Visser BC, Ford JM, Alizadeh AA, Quake SR, Kunz PL, Beausang JF. Surgical and molecular characterization of primary and metastatic disease in a neuroendocrine tumor arising in a tailgut cyst. Cold Spring Harb Mol Case Stud. 2018;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Zappa L, Godwin TA, Sugarbaker PH. Tailgut cyst, an unusual cause of pseudomyxoma peritonei. Tumori. 2009;95:514-517. [PubMed] |
| 14. | Maruyama A, Murabayashi K, Hayashi M, Nakano H, Isaji S, Uehara S, Kusuda T, Miyahara S, Kondo A, Yabana T. Adenocarcinoma arising in a tailgut cyst: report of a case. Surg Today. 1998;28:1319-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Martins P, Canotilho R, Peyroteo M, Afonso M, Moreira A, de Sousa A. Tailgut cyst adenocarcinoma. Autops Case Rep. 2020;10:e2019115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |