Published online Feb 27, 2021. doi: 10.4240/wjgs.v13.i2.141
Peer-review started: November 12, 2020
First decision: December 12, 2020
Revised: December 24, 2020
Accepted: January 14, 2021
Article in press: January 14, 2021
Published online: February 27, 2021
Processing time: 83 Days and 14 Hours
Gastrointestinal (GI) and liver diseases contribute to substantial inpatient morbidity, mortality, and healthcare resource utilization. Finding ways to reduce the economic burden of healthcare costs and the impact of these diseases is of crucial importance. Thirty-day readmission rates and related hospital outcomes can serve as objective measures to assess the impact of and provide further insights into the most common GI ailments.
To identify the thirty-day readmission rates with related predictors and outcomes of hospitalization of the most common GI and liver diseases in the United States.
A cross-sectional analysis of the 2012 National Inpatient Sample was performed to identify the 13 most common GI diseases. The 2013 Nationwide Readmission Database was then queried with specific International Classification of Diseases, Ninth Revision, Clinical Modification codes. Primary outcomes were mortality (index admission, calendar-year), hospitalization costs, and thirty-day readmission and secondary outcomes were predictors of thirty-day readmission.
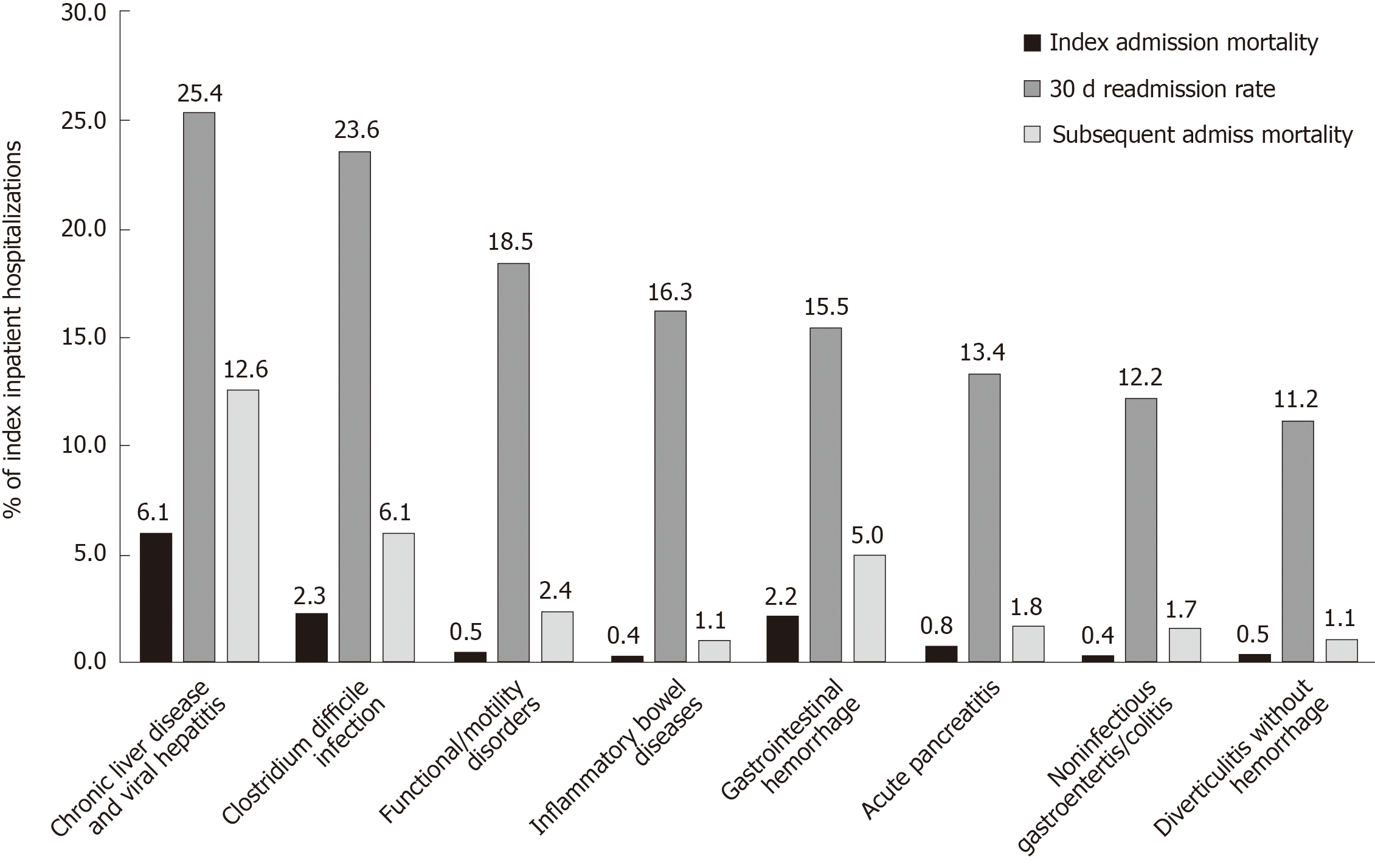
For the year 2013, the thirteen most common GI diseases contributed to 2.4 million index hospitalizations accounting for about $25 billion. The thirty-day readmission rates were highest for chronic liver disease (25.4%), Clostridium difficile (C. difficile) infection (23.6%), functional/motility disorders (18.5%), inflammatory bowel disease (16.3%), and GI bleeding (15.5%). The highest index and subsequent calendar-year hospitalization mortality rates were chronic liver disease (6.1% and 12.6%), C. difficile infection (2.3% and 6.1%), and GI bleeding (2.2% and 5.0%), respectively. Thirty-day readmission correlated with any subsequent admission mortality (r = 0.798, P = 0.001). Medicare/Medicaid insurances, ≥ 3 Elixhauser comorbidities, and length of stay > 3 d were significantly associated with thirty-day readmission for all the thirteen GI diseases.
Preventable and non-chronic GI disease contributed to a significant economic and health burden comparable to chronic GI conditions, providing a window of opportunity for improving healthcare delivery in reducing its burden.
Core Tip: Using the 2013 Nationwide Readmission Database, we sought to elucidate the hospital outcomes, including hospitalization costs, mortality rates, readmission rates, and factors contributing to readmission for the 13 most common gastrointestinal (GI)-related diseases. The results of our study highlight the large economic and healthcare burden for these 13 GI-related diseases and identify factors associated with early readmissions. Our study also reveals that preventable and non-chronic GI diseases such as Clostridium difficile, GI hemorrhage, and acute pancreatitis contribute a significant proportion of the overall costs, mortality, and readmission burden. Our data underscore a crucial opportunity for providers to aim at targeting preemptive care to reduce the initial and subsequent readmissions for these preventable GI-related diseases.
- Citation: Krishna SG, Chu BK, Blaszczak AM, Balasubramanian G, Hussan H, Stanich PP, Mumtaz K, Hinton A, Conwell DL. Hospital outcomes and early readmission for the most common gastrointestinal and liver diseases in the United States: Implications for healthcare delivery. World J Gastrointest Surg 2021; 13(2): 141-152
- URL: https://www.wjgnet.com/1948-9366/full/v13/i2/141.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i2.141
The United States spends nearly 18% of Gross Domestic Product annually on healthcare expenses[1]. In 2013 alone, personal health care spending on digestive diseases and cirrhosis amounted to over $100 billion, with greater than 60% of these costs arising from inpatient care and treatment[2]. Gastrointestinal (GI) diseases are also associated with significant morbidity and mortality, including poorer quality of life and a greater amount of work and activity limitations[3]. Nearly 10% of deaths in the United States have GI disease as the underlying cause where the top ten all-cause mortality includes cirrhosis of the liver, Clostridium difficile (C. difficile) colitis, and gastrointestinal hemorrhage[3]. Several of these diseases have been associated with high rates of readmission, which is not only expensive but also an indicator of inferior quality of care and increased rates of 1-year mortality[4-6]. Finding ways to reduce the economic burden of healthcare costs and the impact of disease on morbidity and mortality is of vital importance.
While there are currently several population-based studies examining readmission data for specific GI and liver disease, there are very few population-based studies evaluating overall readmission rates and their impact for the most common GI and liver diseases as a whole. Hence, we sought to examine the thirty-day readmission rates, mortality and predictors of thirty-day readmission for the most common GI and liver diseases in the United States.
The Nationwide Readmissions Database (NRD) from 2013 was utilized for study development and analysis utilizing the International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis and procedure codes. This database is a part of the Healthcare Cost Utilization Project State Inpatient Databases. The unique aspect of this database is its ability to track patients with patient-specific linkage numbers statewide in all nonfederal acute care hospitals over the course of one year. This database provides unweighted information for roughly 14 million discharges per year and is based on weighting to represent the United States national readmission rates, and it accounts for nearly 36 million discharges annually[7].
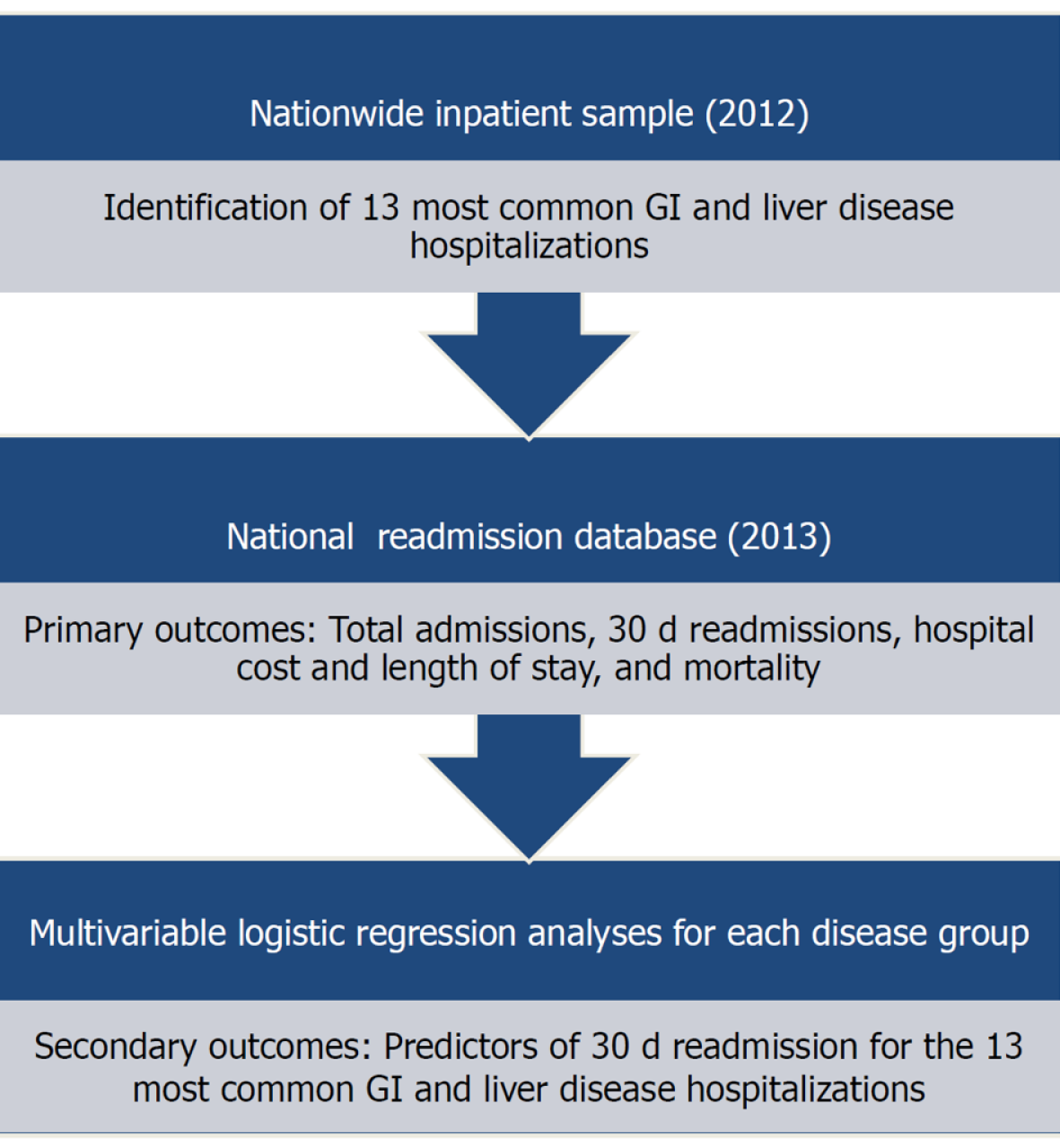
The study schema is represented in Figure 1. Hospitalizations for the 13 most common gastrointestinal diseases were identified based on data from the 2012 Nationwide Inpatient Sample and included GI hemorrhage, cholelithiasis with cholecystitis, acute pancreatitis, intestinal obstruction, appendicitis, chronic liver disease (CLD) including viral hepatitis, diverticulitis without hemorrhage, non-infectious gastroenteritis, obesity, C. difficile infection, GI infection, functional/motility disorder, and inflammatory bowel disease (IBD)[7]. The corresponding ICD-9 codes found in Supplementary Table 1 were used to query the 2013 NRD database. Patients were excluded from index admissions analysis if they were (1) 17 years old or younger, or (2) pregnant at the index admission. Further exclusion criteria were employed for analyzing thirty-day readmissions, including (1) death during the index admission, or (2) discharged in December 2013 since they could not be followed for thirty-day.
Institutional Review Board approval is not necessary for a population-based public data set based on The Ohio State University Data and Specimen Policy and Human Subjects Research Policy.
For each index admission, patient characteristics were gathered, including age, sex, median income quartile based on zip code, and insurance status based on primary payer (Medicaid, Medicare, private insurance, other) indicated on discharge record. Comorbidity classification was carried out using the Agency for Healthcare Research and Quality-Elixhauser Index classifying patients as having less than 3 or greater than or equal to 3 comorbidities for risk adjustment[8]. Hospital characteristics were also collected, including hospital size (small, medium, large) based on the Healthcare Cost Utilization Project developed algorithm and hospital location and teaching status as a single variable (rural, urban nonteaching, and urban teaching hospital). Lastly, length-of-stay was classified as less than or equal to 3 d, 3 to 7 d or greater than 7 d for index admission and disposition to home/home health/against medical advice or other was indicated.
The primary outcome measures were calculated for each of the 13 conditions: total index admissions, thirty-day readmission rate, mean length of stay, mean hospitalization cost of index hospitalization, and frequency and percent mortality at index admission and any subsequent admission during that calendar-year. The secondary outcomes were predictors of thirty-day readmissions for each of the most common GI and liver diseases.
Index admission characteristics, including the total number of admissions, mean length of stay, mean cost, and mortality rate were calculated for the 13 most common GI diseases in addition to thirty-day readmission and calendar-year mortality rates; data were presented with their corresponding 95% confidence intervals. Thirteen different multivariable logistic regression models were fit to evaluate predictors of thirty-day readmission for each of the most common GI and liver diseases. The models adjusted for all patient demographics and hospital characteristics and results were represented using odds ratios (ORs) and 95% confidence intervals. To examine the relationship between thirty-day readmission rates and any subsequent mortality within the calendar-year, Pearson’s correlation (r) with corresponding significance was calculated. Statistical significance was defined by P < 0.05. SAS 9.4 (SAS, Cary, NC, United States) was used for all analyses. All results are weighted and account for the complex survey design to represent national estimates.
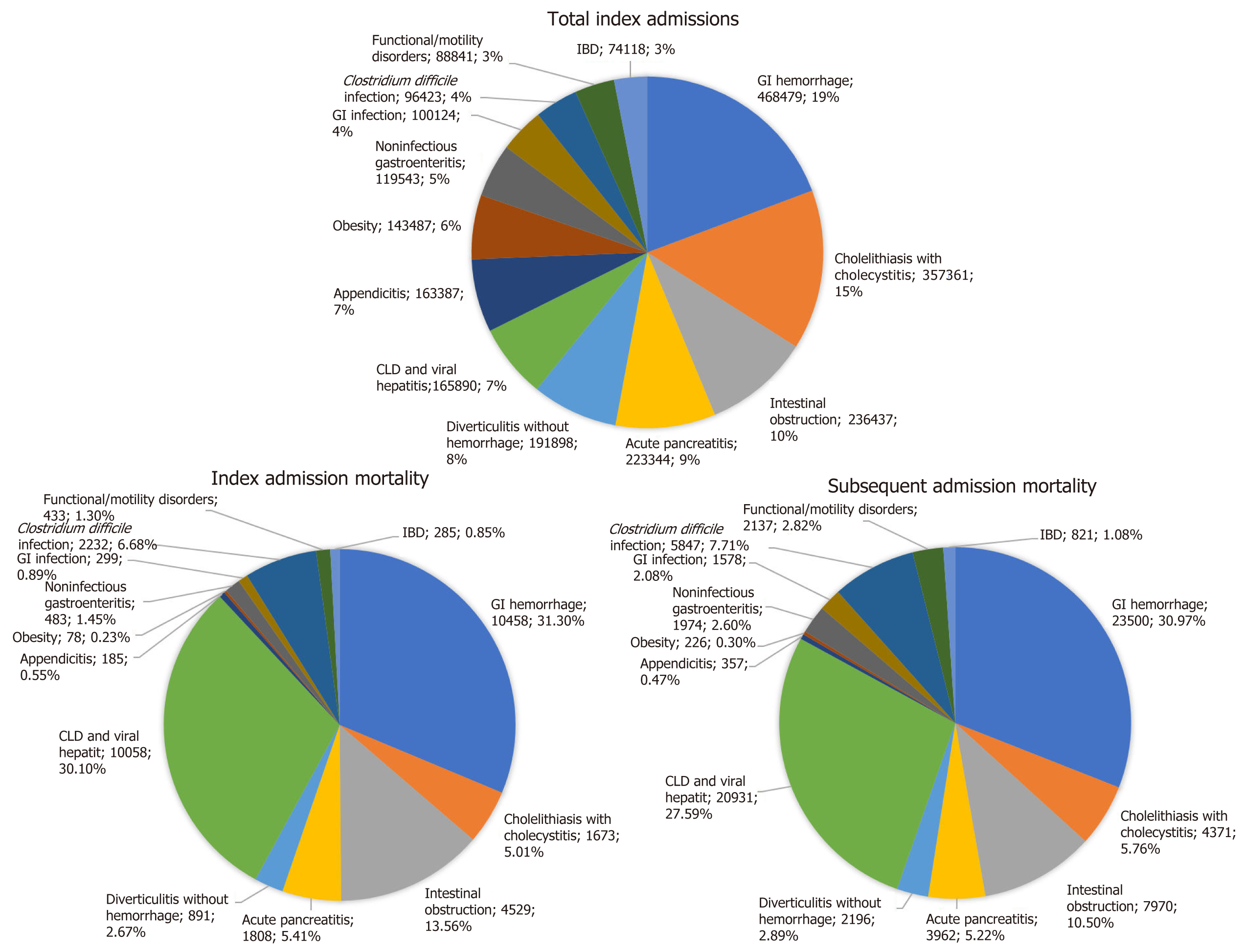
The 13 most common GI diseases accounted for 2.4 million (m) index admissions in 2013, with the most frequent being GI hemorrhage (0.47 m), cholelithiasis with cholecystitis (0.36 m), intestinal obstruction (0.24 m), and acute pancreatitis (0.22 m); (Table 1 and Figure 2). In total, this accounted for 25 billion dollars in healthcare-associated costs (Table 1 and Figure 2). CLDs and viral hepatitis had the highest index and subsequent calendar-year hospitalization associated mortality rate (6.07% and 12.62%, respectively), followed by C. difficile infection (2.32% and 6.06%, respectively) and GI hemorrhage (2.32% and 6.06%, respectively) (Table 1 and Figure 2). Together, CLD and viral hepatitis, GI hemorrhage, C. difficile infection, and intestinal obstruction accounted for 81.6% of all index hospitalization mortality and 76.8% of all subsequent hospitalization-related mortality (one-calendar year) (Figure 2). CLDs and viral hepatitis and C. difficile infection experienced the most prolonged mean duration of index hospitalization of 6 d (Table 1). Obesity and CLDs incurred the highest cost of index hospitalization (Table 1).
| Total index admissions (frequency) | Mean index admission LOS (d) | Mean index admission cost ($) | Index admission mortality (frequency) | Index admission mortality (%) | Subsequent admission mortality (frequency) | Subsequent admission mortality (%) | 30-d readmission rate (%) | |
| Gastrointestinal hemorrhage | 468479 (453166, 483792) | 4.35 (4.30, 4.40) | 9932 (9745, 10119) | 10458 (9962, 10954) | 2.23 (2.15, 2.31) | 23500 (22520, 24479) | 5.02 (4.88, 5.15) | 15.51 (15.28, 15.73) |
| Cholelithiasis with cholecystitis | 357361 (343813, 370909) | 3.88 (3.84, 3.92) | 11983 (11794, 12172) | 1673 (1514, 1833) | 0.47 (0.43, 0.51) | 4371 (4085, 4656) | 1.22 (1.16, 1.29) | 9.28 (9.08, 9.48) |
| Acute pancreatitis | 223344 (216001, 230687) | 4.76 (4.70, 4.83) | 10127 (9906, 10348) | 1808 (1655, 1962) | 0.81 (0.74, 0.88) | 3962 (3711, 4214) | 1.77 (1.67, 1.87) | 13.42 (13.11, 13.72) |
| Intestinal obstruction | 236437 (228766, 244109) | 5.69 (5.62, 5.76) | 11583 (11347, 11819) | 4529 (4262, 4795) | 1.92 (1.81, 2.02) | 7970 (7584, 8356) | 3.37 (3.23, 3.51) | 8.80 (8.59, 9.02) |
| Appendicis | 163387 (156767, 170006) | 2.84 (2.80, 2.89) | 10399 (10207, 10592) | 185 (141, 230) | 0.11 (0.09, 0.14) | 357 (296, 418) | 0.22 (0.18, 0.26) | 5.23 (5.03, 5.44) |
| Chronic liver disease and viral hepatitis | 165890 (157352, 174428) | 6.12 (5.95, 6.29) | 14848 (13854, 15842) | 10058 (9429, 10687) | 6.07 (5.86, 6.28) | 20931 (19694, 22169) | 12.62 (12.29, 12.95) | 25.40 (24.93, 25.86) |
| Diverticulitis without hemorrhage | 191898 (184081, 199716) | 4.69 (4.63, 4.74) | 9986 (9792, 10180) | 891 (791, 990) | 0.46 (0.41, 0.52) | 2196 (2033, 2358) | 1.14 (1.06, 1.22) | 11.23 (10.96, 11.50) |
| Noninfectious gastroenteritis/colitis | 119543 (113494, 125593) | 3.23 (3.19, 3.27) | 6391 (6270, 6512) | 483 (406, 559) | 0.40 (0.34, 0.47) | 1974 (1804, 2145) | 1.65 (1.51, 1.79) | 12.24 (11.91, 12.58) |
| Obesity | 143487 (127160, 159813) | 2.07 (2.00, 2.14) | 12731 (12150, 13312) | 78 (43, 112) | 0.05 (0.03, 0.08) | 226 (117, 336) | 0.16 (0.09, 0.23) | 5.34 (5.01, 5.67) |
| Clostridium difficile infection | 96427 (91904, 100951) | 6.18 (6.08, 6.28) | 10137 (9833, 10442) | 2232 (2061, 2404) | 2.32 (2.15, 2.48) | 5847 (5475, 6219) | 6.06 (5.76, 6.37) | 23.64 (23.10, 24.19) |
| Gastrointestinal infection | 100124 (95396, 104853) | 3.22 (3.17, 3.26) | 6359 (6230, 6488) | 299 (242, 357) | 0.30 (0.24, 0.36) | 1578 (1421, 1736) | 1.58 (1.43, 1.72) | 10.79 (10.45, 11.13) |
| Functiona/motility disorders | 88841 (83923, 93759) | 3.94 (3.83, 4.05) | 7777 (7568, 7986) | 433 (362, 504) | 0.49 (0.41, 0.57) | 2137 (1943, 2330) | 2.41 (2.23, 2.58) | 18.51 (18.03, 19.00) |
| Inflammatory bowel diseases | 74118 (70135, 78101) | 5.16 (5.06, 5.27) | 10500 (10147, 10853) | 285 (224, 345) | 0.38 (0.30, 0.47) | 821 (710, 933) | 1.11 (0.97, 1.25) | 16.32 (15.78, 16.87) |
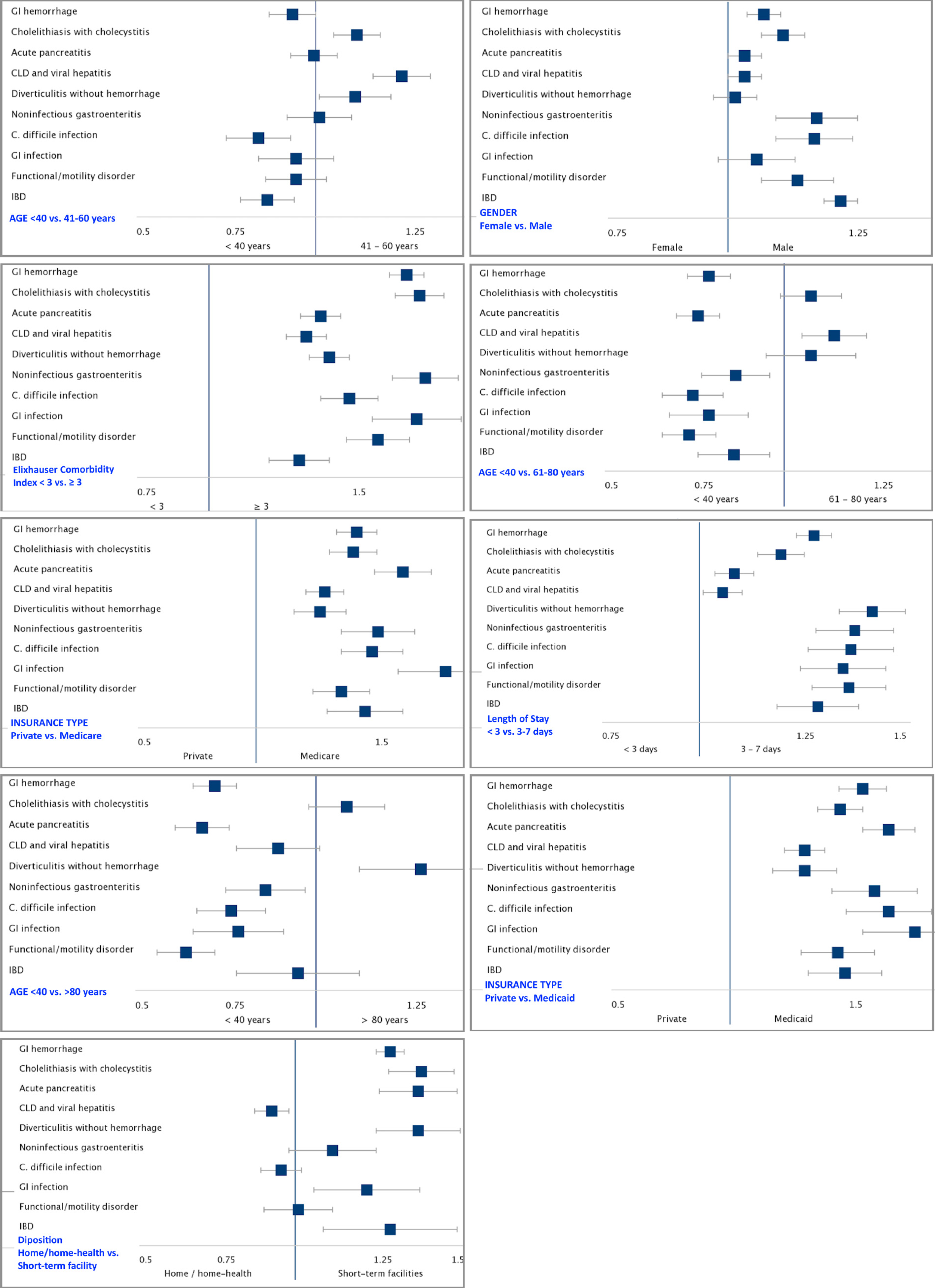
The diseases with the highest thirty-day readmission rates were CLDs and viral hepatitis (25.40%), C. difficile infection (23.64%), and functional/motility disorders (18.51%), Figure 3. Multivariable models for thirty-day readmission after admission for each of the most common GI and liver diseases (Figure 4 and Supplementary Tables 2-5) revealed that Medicare (OR range: 1.19-1.81) and Medicaid (OR range: 1.16-1.66) insurance, Agency for Healthcare Research and Quality-Elixhauser Index of 3 or greater (OR range: 1.18-1.75) and hospitalization duration greater than 3 d (OR: 1.05-5.78) were associated with early readmissions. Compared to younger age groups (≤ 40 years), increasing age was associated with thirty-day readmissions for diverticulitis without hemorrhage, cholelithiasis with cholecystitis, and CLD and viral hepatitis. Disposition of patients to other than home or home-health was associated with early readmissions for GI hemorrhage, cholelithiasis with cholecystitis, acute pancreatitis, diverticulitis without hemorrhage, GI infection, and IBD (Figure 4). In addition, there was a strong positive correlation (r = 0.798) between thirty-day readmission rate and subsequent mortality (P = 0.001; Supplementary Figure 1).
In this analysis of a national inpatient database, we found that emergent conditions such as GI hemorrhage, cholecystitis due to cholelithiasis, intestinal obstruction, and acute pancreatitis were most frequent and accounted for nearly 60% of all index hospitalizations. In terms of inpatient deaths, CLD and GI bleeding together contributed to approximately 60% of index hospitalization and readmission-related mortality. Notably, the mortality rate due to CLD and viral hepatitis during index and subsequent admissions was more than twice higher than any other disease state. Unfortunately, mortality rates due to acute reversible disorders such as C. difficile infection and GI hemorrhage, albeit elevated, nearly tripled during subsequent hospitalizations (from 2% to 5%-6% of admissions). While chronic GI diseases such as those involving the liver, functional/motility disorders, and IBD had high thirty-day readmission rates (15%-25%), a significant opportunity existed to decrease readmission rates (13%-23%) in preventable and non-chronic GI diseases such as C. difficile infection, GI hemorrhage, and acute pancreatitis. In addition, readmissions within thirty-day correlated with increasing rates of mortality during subsequent hos-pitalizations in the same calendar-year.
Gastrointestinal hemorrhage, CLD and viral hepatitis, intestinal obstruction, and C. difficile infection attributed to an alarming 81.64% of all index admission mortality and 76.77% of all subsequent admission mortality. The mortality associated with CLD and viral hepatitis was the highest among the GI diseases examined at 6.07% of index admissions and 12.62% at any subsequent hospitalization. Medical complications following a diagnosis of liver disease are well known, including decompensated cirrhosis, fulminant liver failure, hepatocellular carcinoma, sepsis, acute renal failure, variceal bleeding, and hepatic encephalopathy[9]. The overall mortality burden from CLD and viral hepatitis are expected to continue to increase. In the case of cirrhosis, observational studies have demonstrated a higher burden of mortality with United States annual deaths from cirrhosis increased by 65% from 1999 to 2016, largely driven due to alcoholic cirrhosis and NAFLD[10,11]. Similarly, an assessment of the global burden of viral hepatitis from the global burden of disease study 2013 also demonstrated global viral hepatitis deaths increased from 0.89 million to 1.45 million, an increase far outpacing other communicable diseases[12]. Hospitalizations with a primary diagnosis of GI hemorrhage accounted for 1 of 5 index admissions and 1 of 3 deaths at index or subsequent (same calendar-year) hospitalization. The mortality rate for GI hemorrhage was amongst the highest, notably incurring twice the index mortality rate at any subsequent hospitalization within one-calendar year. Our study encompassed all categories of GI bleed and did not distinguish between the types and sources of GI bleed. A review of the primary literature revealed similarly high mortality rates in other studies. In-hospital mortality rates for non-variceal Upper GI hemorrhage were approximately 2.1% in a 2009 nationwide database analysis[13]. A nationwide study of lower GI bleeding in the United Kingdom revealed in-hospital mortality of 3.4% with a 7.0% subsequent readmission mortality rate, and these findings are comparable to our study[14]. Another alarming finding is the high mortality rates of C. difficile infection. Mortality is initially at 2.32% for index admission; however, mortality quickly jumps to 6.06% for readmissions. The high morbidity and mortality associated with C. difficile infections are well known[15,16]. Prior studies of the nationwide inpatient sample from 1993-2003 revealed a case fatality rate of around 3%-4% for discharged patients with a primary diagnosis of C. difficile[17]. The high initial and subsequent mortality rates for preventable and non-chronic GI diseases such as C. difficile and GI bleeding underscore a key opportunity for providers to focus on preventative care to reduce initial and subsequent readmissions.
Costs for hospitalizations with GI diseases are significant. Mean index admission costs are $15000 for CLD and viral hepatitis, $12000 for cholelithiasis with cholecystitis, and $10000 for preventable GI diseases such as GI hemorrhage, C. difficile infection and acute pancreatitis. In comparison, the average hospitalization costs were $8000 for chronic obstructive pulmonary disease exacerbation, $10000 for Pneumonia, and $11000 for congestive heart failure exacerbation (CHF) in 2013 adjusted dollars[18]. Total index admission costs for GI hemorrhage were $4.6 billion, followed by $4.2 billion in cholelithiasis with cholecystitis. Total costs for C. difficile infection in index admissions were approximately $1 billion and $2.4 billion for CLD and viral hepatitis, whereas, in large part due to sheer numbers, total index admissions cost was roughly $10 billion each for pneumonia and CHF exacerbations.
The average national length of stay is approximately 4.5 d[19]. Among the thirteen most common GI diseases examined, 5 have a longer duration of stay than the national average and seven are below. Although not uniformly consistent, conditions with higher index mortality rates were generally paired with a longer initial length of stay. Among the four diseases with the highest index admission mortality (GI Hemorrhage, CLD and viral hepatitis, C. difficile, and intestinal obstruction), three of which had LOS higher than the national average. Our data suggest that there is a correlation between length of stay and mortality rate. However, our analysis does not examine patients in different stages of a disease state. We suspect that patients with higher mortality burden exist in more severe disease states, thus leading to more prolonged hospital admissions.
Readmission rates for GI diseases ranged from 5% to 25%. Chronic GI diseases such as CLD and IBD had high readmission rates, but preventable and non-chronic GI diseases such as C. difficile, GI hemorrhage, and acute pancreatitis also presented with significant readmission rates (13%-23%). Thirty-day readmission rates for GI diseases were comparable to other disease categories in previously examined database analysis: CHF exacerbations 23%, chronic obstructive pulmonary disease exacerbation 20.1%, 18.1% septicemia, and 14.2% for acute myocardial infarction[20].
Age, gender, income, hospital size, type of hospital, and disposition were not uniformly predictors of thirty-day readmission for all thirteen diseases examined. However, our analyses showed that patients with Elixhauser comorbidity indices ≥ 3, a longer length of stay, and Medicare/Medicaid were significantly more likely to be readmitted in the conditions examined. Patients with multiple comorbidities are often known to be at increased risk of readmission due to their overall poor baseline health status, which is congruent with findings from other studies[21-23]. As our analysis is unable to stratify the severity of a patient's illness, we believe that longer length of stay serves as a surrogate marker for the severity of a patient’s illness; longer hospitaliz-ation indicates more critically ill patients who are more prone to readmission. Our data should not be interpreted as evidence for reducing the length of stay as we are unable to compare patient disease severity and duration of stay due to the absence of objective clinical severity data.
Possessing Medicare and/or Medicaid were also predictors of readmission. Detailed analysis as to why Medicare and Medicaid patients had higher rates of readmission is challenging to discern while utilizing the NRD. Further studies should examine the reasons for readmissions in this population and to investigate strategies to reduce readmissions.
Disposition of patients to other than home or home-health was associated with early readmissions for GI hemorrhage, acute pancreatitis, cholelithiasis with cholecystitis, diverticulitis without hemorrhage, GI infection, and IBD. However, there was no association with C. difficile. Increasing age was also associated with early readmissions for diverticulitis, cholelithiasis with cholecystitis and CLD and viral hepatitis.
Our multivariable analyses show that factors such as disposition, age, type of insurance, length of stay, and comorbidities are predictors of readmission risks. Our analyses highlight an area of improvement for hospitals, discharging providers, and outpatient providers to not only recognize patients at increased risk for readmission with the aforementioned predictors but also to develop better post-discharge care coordination in patients with these conditions to reduce their readmissions. As the readmission rate is correlated with increased mortality, there is a clear window of opportunity to reduce the readmission rates, especially for preventable and non-chronic diseases. In the case of C. difficile, frequent antibiotic use, particularly clindamycin, cephalosporins and fluoroquinolones, and long-term proton-pump inhibitor use can increase the risk of recurrent C. difficile and should be carefully monitored post-discharge[24]. Newer medications such as Bezlotoxumab, a Food and Drug Administration approved monoclonal antibody against toxin B, offer cost-effective therapeutic option in reducing the incidence of recurrent C. difficile in high-risk patient populations[25,26]. In acute pancreatitis, alcohol consumption, medications, hypertriglyceridemia, and gallstones are known triggers[27]. Readmissions of acute pancreatitis can occur due to uncontrolled symptom management, recurrence of acute pancreatitis, and post pancreatitis complications such as pancreatic necrosis and pseudocyst formation[28]. Readmission reduction strategies can include appropriate management of pain symptoms and close monitoring and treatment of underlying etiologies. Patients with alcohol-induced pancreatitis should have close management of alcohol use disorder with appropriate counseling and consideration of pha-rmacologic therapies[29,30]. In cases of severe hypertriglyceridemia, in addition to non-pharmacologic therapies such as weight loss and dietary changes, statin therapies were associated with a reduction in the number of patients developing pancreatitis[31]. There is some evidence that routine plasmapheresis may also reduce the incidence of recurrent pancreatitis, though there remains a paucity of data, and additional data is needed[32]. For patients with GI hemorrhage, strategies to reduce index admission and readmission include strict adherence to proton-pump inhibitors therapy, avoidance of NSAIDs, and treatment of underlying infections such as Helicobacter pylori. Patients on oral anticoagulation should have frank conversations with their providers weighing the risks and benefits of anticoagulation, as well as using validated scoring systems such as HAS-BLED scores in the case of atrial fibrillation[33].
There were inherent limitations with nationwide databases that rely on accurate ICD-9 coding[34,35]. The NRD is based on administrative data and lacks clinical variables, which preclude our ability to stratify patients based on the severity of their disease state. Important measures such as race/ethnicity and geographic location were removed as they were considered as patient identifiers. We also did not examine specific disease states or specific conditions associated with some of these GI diseases as predictors of early readmission. Furthermore, the NRD does not link patients for more than a single calendar-year. Finally, our analysis did not focus on predictors of mortality since it has been previously examined in prior papers[3].
In conclusion, readmissions are associated with increased mortality in patients with common GI diseases. While a majority of GI readmissions are associated with chronic diseases, especially CLD and viral hepatitis, a significant proportion is accounted for by preventable and non-chronic disease states including, GI hemorrhage and C. difficile infection. The data contained herein supports the need for improved healthcare quality and preventative medicine to decrease the overall GI burden. This analysis also demonstrates that targeted research, quality improvement, and preventative healthcare strategies for hospitalized adult patients can likely reduce the global GI disease burden.
Gastrointestinal (GI) related diseases account for over $100 billion in healthcare expenditures in the United States.
Currently, few population-based studies are evaluating key hospital metrics such as thirty-day readmission rates, mortality and predictors of thirty-day readmissions for the most common GI diseases as a whole. Obtaining this information can provide further insights for clinicians and key stakeholders in recognizing the impact of these diseases and identifying opportunities for improved healthcare delivery.
We aimed to find the most common GI-related illnesses and calculate the total index admissions, thirty-day readmission rates, mean length of stay, mean hospitalization costs, and the mortality rates for each of these diseases. We also sought to assess predictors of thirty-day readmissions for these conditions.
The Nationwide Inpatient Sample (2012) identified the 13 most common GI and Liver disease hospitalizations, which included GI hemorrhage, cholelithiasis with cholecystitis, acute pancreatitis, and Clostridium difficile (C. difficile) infection. The 2013 Nationwide Readmission Database was then queried with each disease to obtain hospital outcomes and readmission data. Multivariable logistic regression analyses for each disease group identified predictors for thirty-day readmission.
The thirteen GI diseases accounted for 2.4 million index hospitalizations and $25 billion in healthcare-associated costs. Chronic conditions such as those involving the liver, functional/motility disorders and inflammatory bowel disease were associated with high readmission rates, mortality rates and hospitalization costs. However, potentially preventable and non-chronic GI ailments such as GI hemorrhage, acute pancreatitis and C. difficile infection were also linked with considerable readmission rates, mortality rates and hospitalization costs. Patient variables such as type of insurance, presence of ≥ 3 Elixhauser comorbidities, and length of stay > 3 d were predictors of thirty-day readmission for all the thirteen GI diseases.
GI-related diseases contribute to substantial inpatient morbidity, mortality and healthcare resource utilization. Our study highlighted the sizeable portion of readmissions, mortality rates and hospitalization costs attributed to potentially preventable and non-chronic GI diseases such as C. difficile infection, gastrointestinal bleeding, and acute pancreatitis.
Our study identifies a need for improved healthcare quality and a stronger emphasis on preventative medicine to decrease the overall GI burden, especially with preventable and non-chronic GI diseases.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: American College of Gastroenterology; American Society for Gastrointestinal Endoscopy; and American Gastroenterological Association.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cao ZF, Tashkandi E S-Editor: Zhang L L-Editor: A P-Editor: Zhang YL
| 1. | Centers for Medicare and Medicaid Services. National Health Expenditure Data. 2019. Available from: https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical. |
| 2. | Dieleman JL, Baral R, Birger M, Bui AL, Bulchis A, Chapin A, Hamavid H, Horst C, Johnson EK, Joseph J, Lavado R, Lomsadze L, Reynolds A, Squires E, Campbell M, DeCenso B, Dicker D, Flaxman AD, Gabert R, Highfill T, Naghavi M, Nightingale N, Templin T, Tobias MI, Vos T, Murray CJ. US Spending on Personal Health Care and Public Health, 1996-2013. JAMA. 2016;316:2627-2646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 777] [Cited by in RCA: 749] [Article Influence: 83.2] [Reference Citation Analysis (0)] |
| 3. | Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ, Gangarosa LM, Thiny MT, Stizenberg K, Morgan DR, Ringel Y, Kim HP, DiBonaventura MD, Carroll CF, Allen JK, Cook SF, Sandler RS, Kappelman MD, Shaheen NJ. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012; 143: 1179-1187. e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1355] [Cited by in RCA: 1467] [Article Influence: 112.8] [Reference Citation Analysis (1)] |
| 4. | Fagan KJ, Zhao EY, Horsfall LU, Ruffin BJ, Kruger MS, McPhail SM, O'Rourke P, Ballard E, Irvine KM, Powell EE. Burden of decompensated cirrhosis and ascites on hospital services in a tertiary care facility: time for change? Intern Med J. 2014;44:865-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Chopra T, Neelakanta A, Dombecki C, Awali RA, Sharma S, Kaye KS, Patel P. Burden of Clostridium difficile infection on hospital readmissions and its potential impact under the Hospital Readmission Reduction Program. Am J Infect Control. 2015;43:314-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418-1428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3684] [Cited by in RCA: 3914] [Article Influence: 244.6] [Reference Citation Analysis (0)] |
| 7. | Healthcare Cost and Utilization Project. NRD Overview 2020. Agency for Healthcare Research and Quality. Available from: https://www.hcup-us.ahrq.gov/nrdoverview.jsp. |
| 8. | Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6456] [Cited by in RCA: 7797] [Article Influence: 288.8] [Reference Citation Analysis (0)] |
| 9. | Leber B, Spindelboeck W, Stadlbauer V. Infectious complications of acute and chronic liver disease. Semin Respir Crit Care Med. 2012;33:80-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 77] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 10. | Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ. 2018;362:k2817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 337] [Cited by in RCA: 580] [Article Influence: 82.9] [Reference Citation Analysis (1)] |
| 11. | Hirode G, Vittinghoff E, Wong RJ. Increasing Clinical and Economic Burden of Nonalcoholic Fatty Liver Disease Among Hospitalized Adults in the United States. J Clin Gastroenterol. 2019;53:765-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Stanaway JD, Flaxman AD, Naghavi M, Fitzmaurice C, Vos T, Abubakar I, Abu-Raddad LJ, Assadi R, Bhala N, Cowie B, Forouzanfour MH, Groeger J, Hanafiah KM, Jacobsen KH, James SL, MacLachlan J, Malekzadeh R, Martin NK, Mokdad AA, Mokdad AH, Murray CJL, Plass D, Rana S, Rein DB, Richardus JH, Sanabria J, Saylan M, Shahraz S, So S, Vlassov VV, Weiderpass E, Wiersma ST, Younis M, Yu C, El Sayed Zaki M, Cooke GS. The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet. 2016;388:1081-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1042] [Cited by in RCA: 989] [Article Influence: 109.9] [Reference Citation Analysis (0)] |
| 13. | Abougergi MS, Travis AC, Saltzman JR. The in-hospital mortality rate for upper GI hemorrhage has decreased over 2 decades in the United States: a nationwide analysis. Gastrointest Endosc 2015; 81: 882-8. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 176] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 14. | Oakland K, Guy R, Uberoi R, Hogg R, Mortensen N, Murphy MF, Jairath V; UK Lower GI Bleeding Collaborative. Acute lower GI bleeding in the UK: patient characteristics, interventions and outcomes in the first nationwide audit. Gut. 2018;67:654-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 15. | Miller MA, Hyland M, Ofner-Agostini M, Gourdeau M, Ishak M; Canadian Hospital Epidemiology Committee. Canadian Nosocomial Infection Surveillance Program. Morbidity, mortality, and healthcare burden of nosocomial Clostridium difficile-associated diarrhea in Canadian hospitals. Infect Control Hosp Epidemiol. 2002;23:137-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 144] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 16. | Kwon JH, Olsen MA, Dubberke ER. The morbidity, mortality, and costs associated with Clostridium difficile infection. Infect Dis Clin North Am. 2015;29:123-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 143] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 17. | Ricciardi R, Rothenberger DA, Madoff RD, Baxter NN. Increasing prevalence and severity of Clostridium difficile colitis in hospitalized patients in the United States. Arch Surg. 2007;142:624-31; discussion 631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 206] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 18. | Pfuntner A, Wier LM, Steiner C. Costs for Hospital Stays in the United States, 2010. HCUP Statistical Brief #146. January 2013. Agency for Healthcare Research and Quality. Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb146.pdf. |
| 19. | Weiss AJ, Elixhauser A. Overview of Hospital Stays in the United States, 2012. HCUP Statistical Brief #180. October 2014. Agency for Healthcare Research and Quality. Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb180-Hospitalizations-United-States-2012.pdf. |
| 20. | Fingar KR, Barrett ML, Jiang HJ. A Comparison of All-Cause 7-Day and 30-Day Readmissions, 2014. HCUP Statistical Brief #230. October 2017. Agency for Healthcare Research and Quality. Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb230-7-Day-Versus-30-Day-Readmissions.jsp. |
| 21. | Donzé J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:f7171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 152] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 22. | Librero J, Peiró S, Ordiñana R. Chronic comorbidity and outcomes of hospital care: length of stay, mortality, and readmission at 30 and 365 days. J Clin Epidemiol. 1999;52:171-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 224] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 23. | Siddique SM, Mehta SJ, Lewis JD, Neuman MD, Werner RM. Rates of Hospital Readmission Among Medicare Beneficiaries With Gastrointestinal Bleeding Vary Based on Etiology and Comorbidities. Clin Gastroenterol Hepatol 2019; 17: 90-97. e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, McFarland LV, Mellow M, Zuckerbraun BS. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478-98; quiz 499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1179] [Cited by in RCA: 1187] [Article Influence: 98.9] [Reference Citation Analysis (0)] |
| 25. | Singh T, Bedi P, Bumrah K, Singh J, Rai M, Seelam S. Updates in Treatment of Recurrent Clostridium difficile Infection. J Clin Med Res. 2019;11:465-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 26. | Alonso CD, Mahoney MV. Bezlotoxumab for the prevention of Clostridium difficile infection: a review of current evidence and safety profile. Infect Drug Resist. 2019;12:1-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Whitlock TL, Repas K, Tignor A, Conwell D, Singh V, Banks PA, Wu BU. Early readmission in acute pancreatitis: incidence and risk factors. Am J Gastroenterol. 2010;105:2492-2497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 28. | Vipperla K, Papachristou GI, Easler J, Muddana V, Slivka A, Whitcomb DC, Yadav D. Risk of and factors associated with readmission after a sentinel attack of acute pancreatitis. Clin Gastroenterol Hepatol. 2014;12:1911-1919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 29. | Nordback I, Pelli H, Lappalainen-Lehto R, Järvinen S, Räty S, Sand J. The recurrence of acute alcohol-associated pancreatitis can be reduced: a randomized controlled trial. Gastroenterology. 2009;136:848-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 160] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 30. | Swift RM, Aston ER. Pharmacotherapy for alcohol use disorder: current and emerging therapies. Harv Rev Psychiatry. 2015;23:122-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 31. | Preiss D, Tikkanen MJ, Welsh P, Ford I, Lovato LC, Elam MB, LaRosa JC, DeMicco DA, Colhoun HM, Goldenberg I, Murphy MJ, MacDonald TM, Pedersen TR, Keech AC, Ridker PM, Kjekshus J, Sattar N, McMurray JJ. Lipid-modifying therapies and risk of pancreatitis: a meta-analysis. JAMA. 2012;308:804-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 32. | Piolot A, Nadler F, Cavallero E, Coquard JL, Jacotot B. Prevention of recurrent acute pancreatitis in patients with severe hypertriglyceridemia: value of regular plasmapheresis. Pancreas. 1996;13:96-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 82] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2971] [Cited by in RCA: 3360] [Article Influence: 224.0] [Reference Citation Analysis (0)] |
| 34. | Attenello FJ, Mack WJ. Pitfalls of administrative database analysis are evident when assessing the 'weekend effect' in stroke. Evid Based Med. 2017;22:35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Hashimoto RE, Brodt ED, Skelly AC, Dettori JR. Administrative database studies: goldmine or goose chase? Evid Based Spine Care J. 2014;5:74-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 110] [Article Influence: 10.0] [Reference Citation Analysis (0)] |