Published online Feb 27, 2021. doi: 10.4240/wjgs.v13.i2.116
Peer-review started: October 17, 2020
First decision: December 1, 2020
Revised: December 13, 2020
Accepted: December 23, 2020
Article in press: December 23, 2020
Published online: February 27, 2021
Processing time: 110 Days and 12.9 Hours
A clutch cutter is a scissor-type knife used in endoscopic submucosal dissection (ESD) for gastrointestinal tract tumors. The assistant during the ESD using a clutch cutter (ESD-C) needs to rotate the device and grasp the target tissue appropriately; therefore, the assistant’s skill may affect the technical outcomes of ESD-C.
To determine how assistant skill level affected the technical outcomes of gastric ESD-C using an ex vivo porcine training model.
In this pilot study, mock lesions of 15-30 mm in diameter were created in the middle or lower third of the porcine stomach. A total of 32 ESD-C procedures were performed by 16 trainees. Each trainee operator performed two ESD-C procedures; one ESD-C was assisted by an expert (ESD-C-E), and the other was assisted by a non-expert (ESD-C-NE). The total procedure time of the ESD was set as the primary outcome, and en bloc resection rate, complete procedure rate, perforation rate, and each procedure time/speed for mucosal incision or submucosal dissection were set as the secondary outcomes. In addition, we investigated factors associated with the difficulty of ESD including incompletion of ESD procedure, a long procedure time (≥ 20 min) or intraoperative perforation.
The median total procedure time of the ESD-C-E was significantly shorter than that of the ESD-C-NE (12.9 min vs 21.9 min, P = 0.001). The en bloc resection rate was 100% in both groups. Complete resection rates of the ESD-C-E and ESD-C-NE groups were 100% and 93.8%, respectively. No intraoperative perforation was observed in both groups. In the multivariate analysis, assistant skill was significantly associated with the difficulty of ESD, with the highest odds ratio of 16.5.
Assistance by an expert is an important factor when trainees perform ESD-C procedures.
Core Tip: The influence of assistant skill level on the technical outcomes of gastric endoscopic submucosal dissection with a scissor-type knife, clutch cutter (ESD-C) is unclear. We conducted an ex vivo porcine model study to compare the treatment outcomes of ESD-C assisted by an expert and those assisted by a non-expert. The median total procedure time of the ESD-C assisted by an expert was significantly shorter than that of the ESD-C assisted by a non-expert. Furthermore, assistant skill was significantly associated with the difficulty of ESD in multivariate analysis. Therefore, assistance by an expert is an important factor in ESD-C procedures.
- Citation: Esaki M, Horii T, Ichijima R, Wada M, Sakisaka S, Abe S, Tomoeda N, Kitagawa Y, Nishioka K, Minoda Y, Tsuruta S, Suzuki S, Akiho H, Ihara E, Ogawa Y, Gotoda T. Assistant skill in gastric endoscopic submucosal dissection using a clutch cutter. World J Gastrointest Surg 2021; 13(2): 116-126
- URL: https://www.wjgnet.com/1948-9366/full/v13/i2/116.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i2.116
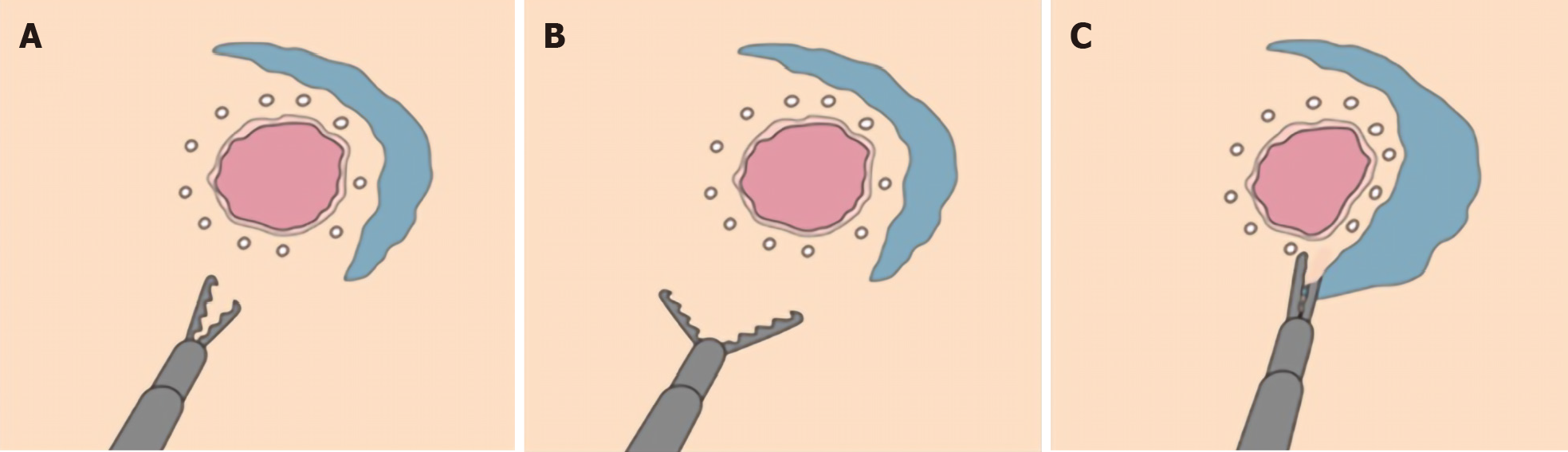
Endoscopic submucosal dissection (ESD) has been widely used as a local treatment for lesions in the gastrointestinal tract including the esophagus, stomach, duodenum, and colorectum[1-4]. Many devices, including endo-knives, have been developed to improve the ESD procedure[5-7]. Conventional ESD has been performed using two traditional knives: needle-type and insulated-tip knives. Subsequently, the clutch cutter (CC) (DP2618DT; Fujifilm Medical, Tokyo, Japan), a scissor-type electrosurgical knife, has been invented and used during ESD to facilitate the procedure[8-10]. The CC can catch and cut target tissues precisely using electrosurgical power. The exterior of the knife is insulated, which prevents unintentional perforations. The safety and efficacy of ESD using CC (ESD-C) and superiority of ESD-C over other devices, including needle and insulated-tip knives, have been reported[11-16]. ESD-C is characterized as a unique procedure using a scissor-type knife, which is different from ESD with other knives. The ESD-C procedure requires the technical skills of the assistant to rotate the device at an appropriate position and grasp the target tissue (Figure 1). These are not required for ESD using other knives such as needle-type and insulated-tip knives. Thus, it is considered that the skills of the assistant, as well as those of the operator, might impact the treatment outcomes of ESD-C[17,18]. However, it remains to be determined how the assistant’s skill level affects the outcomes of ESD since this could not be investigated in clinical practice due to the ethical issues of assuring the safety of the ESD procedure. In this study, to assess this question, we performed an ex vivo porcine model study to determine how the assistant’s skill level affects the technical outcomes of ESD-C.
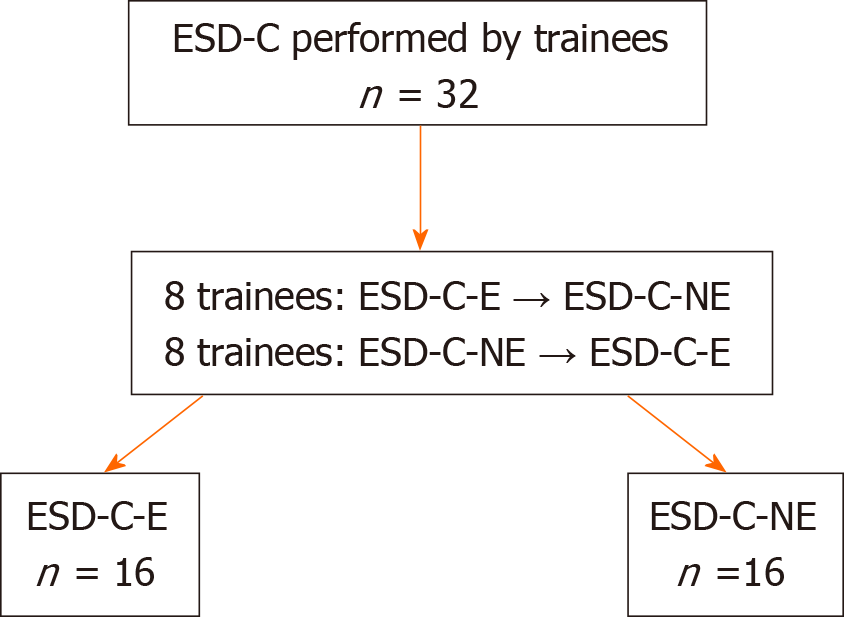
This was an ex vivo experimental study conducted during the Kitakyushu ESD Hands-on Seminar and Tokyo ESD Hands-on Seminar using porcine models. A total of 19 participants (16 operators and 3 assistants) were enrolled. All operators were gastrointestinal trainees with experience performing less than 20 ESD procedures. One assistant was defined as an expert who had experience in not only assisting but also operating in at least 50 ESD procedures. The remaining two assistants were defined as non-experts with experience in operating or assisting in no more than 10 ESD procedures. Each operator performed two ESD procedures, one of which was assisted by the expert (ESD-C-E) and the other was assisted by a non-expert (ESD-C-NE). The protocol of this study was approved by the Institutional Review Board at Kitakyushu Municipal Medical Center (ID: 20191076). Although this was an ex vivo animal model study, it was conducted in accordance with the guidelines the Animal Research Reporting in vivo Experiments as much as possible.
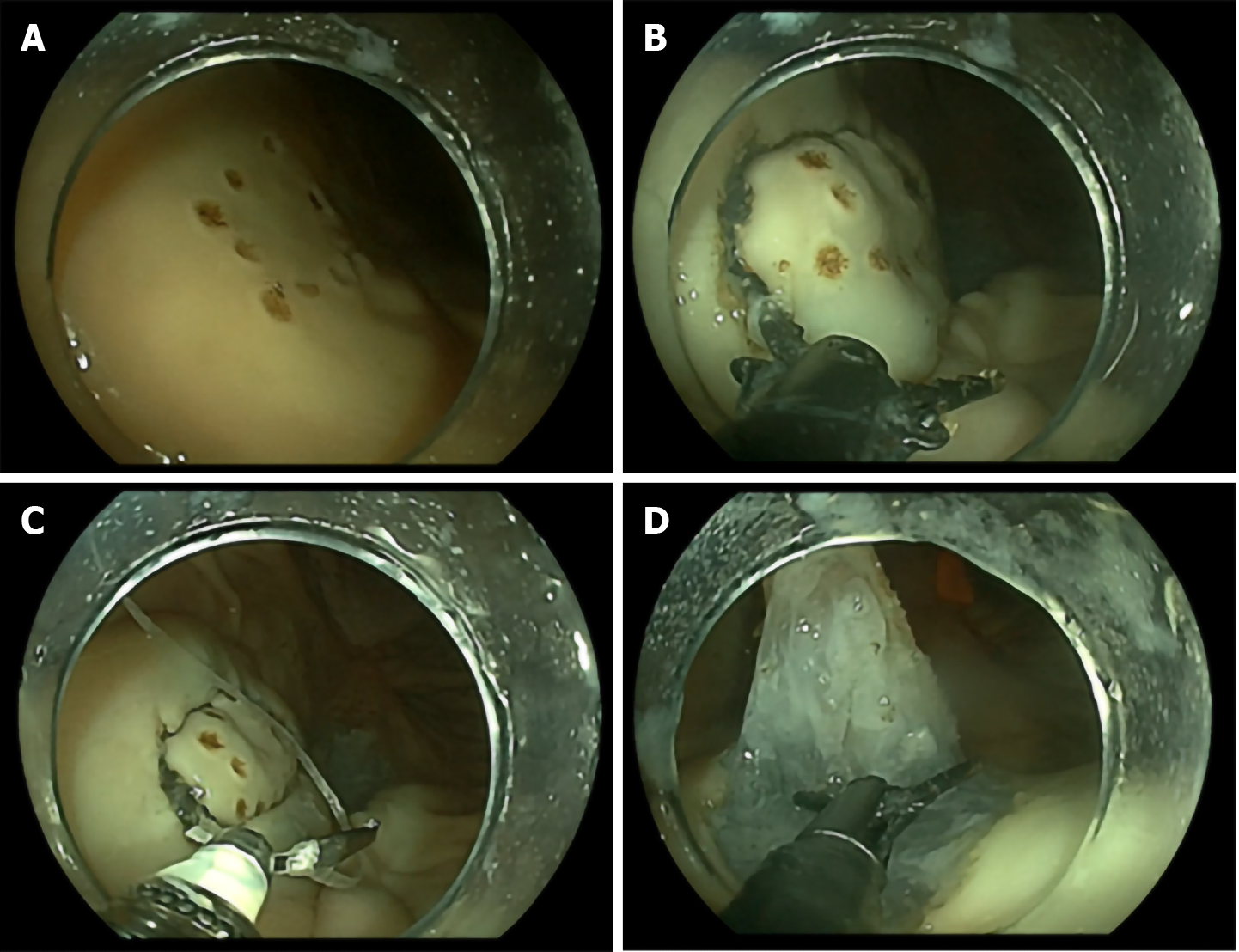
Living animals were not used in this study. The frozen porcine stomach was obtained from a local slaughterhouse and admitted to the experimental endoscopy room on the morning of the study to be used as the ex vivo porcine model. After rinsing the stomach with normal saline, the overtube (TOP, Tokyo, Japan) was inserted into the oral side of the porcine stomach, while its anal side was tied. The stomach was covered by the plate electrode and fixed to the plastic case. Mock lesions of 15-30 mm in diameter were created on the stomach by at least eight marking dots using the endo-knife (Figure 2A). These lesions were made on the anterior wall, greater curvature, or posterior wall in the middle or lower third of the stomach.
Sixteen trainees performed all the ESD-C procedures using an upper gastrointestinal endoscope (GIF-Q260J, Olympus, Tokyo, Japan, or EG-L600WR7, Fujifilm, Tokyo, Japan). The ESD-C was performed as previously described[8,12,15]. In brief, hyaluronic acid solution (MucoUp; Boston Scientific, Tokyo, Japan), supplemented with a small amount of indigo carmine, was first injected into the area around the lesions using an injection needle (SureLIFTERTM, Tokyo, Japan). Then a circumferential mucosal incision was made using a CC. The cutting line was adjusted by rotating the CC at an appropriate position. The target mucosal tissue was grasped, lifted up, and then cut using the CC with electrosurgical current (Figure 2B). After the circumferential mucosal incision was completed, the hemoclip, with dental floss, was attached to the proximal edge of the lesion for the hemoclip traction method, which was useful for submucosal dissection (Figure 2C)[19]. Subsequently, submucosal dissection was performed along the dissection line by the CC. The target submucosa was grasped, lifted up, and cut with appropriate rotation of the CC in a similar manner to the mucosal incision (Figure 2D). Additional injections of the hyaluronic acid solution with indigo carmine were administered when required. The mucosal incision and submucosal dissection were carried out using the VIO 300D electrosurgical unit (ERBE Elektromedizin; GmbH, Tubingen, Germany) in Endo Cut mode (Endocut Q, effect 2, cut interval 3, cut duration 1) and an electric water-jet pump (OFP-2; Olympus, Tokyo, Japan or JW-2; Fujifilm, Tokyo, Japan).
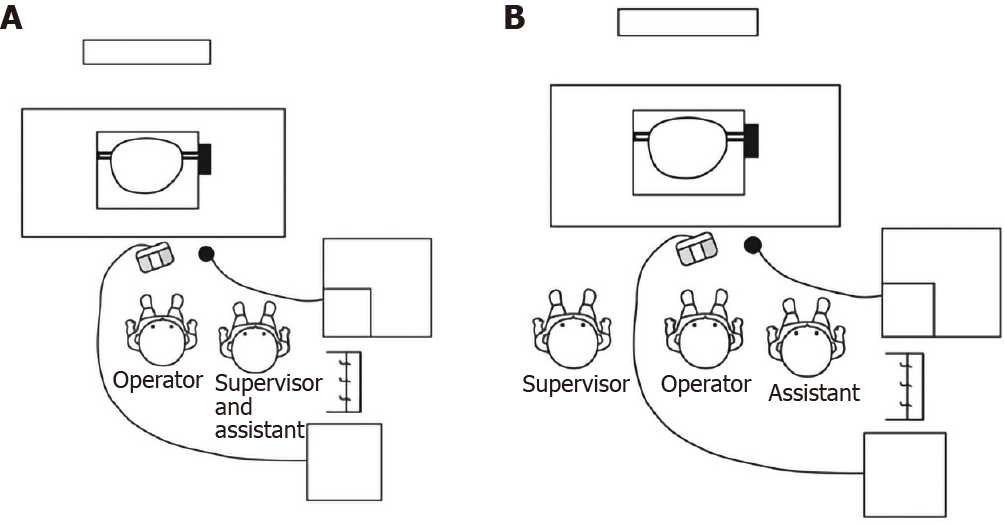
All 16 trainees performed two ESD-C procedures each. As a result, 32 ESD-C procedures were performed in total. One ESD-C was performed with an expert assistant who also guided the ESD procedure when required (ESD-C-E), and the other was performed with a non-expert assistant (ESD-C-NE). On a level playing field with the ESD-C-E group, one expert was positioned beside the operator (separate from the trainee assistant) to guide the ESD procedure in the ESD-C-NE group. The positioning of the staff and the instruments during the ESD-C-E and ESD-C-NE are shown in Figure 3A and B, respectively. Sixteen trainee operators were divided into two groups of eight each and classified as the ESD-C-E first group and ESD-C-NE first group, where the first ESD-C procedure was performed with the experts and non-experts, respectively (Figure 4). When it took more than 30 min to complete the ESD-C procedure, the supervisor judged whether the trainee could complete it by himself or herself and, if necessary, took the place of the trainee in both ESD-C-E and ESD-C-NE groups. The complete ESD was defined as the ESD-C procedure that was completed by the trainees themselves.
The primary outcome of this study was defined as the total procedure time (min). Secondary outcomes included the incision time (min), incision speed (mm/min), dissection time (min), dissection speed (mm2/min), en bloc resection rate (%), complete ESD rate (%), and perforation rate (%). The total procedure time was defined as the time from the beginning of the mucosal incision to the completion of submucosal dissection. The incision time was defined as the time from the beginning to the completion of the mucosal incision. The incision speed was defined as the circumferential length of the resected specimen/incision time (mm/min). Dissection time was defined as the time from the beginning to the completion of the submucosal dissection. Dissection speed was defined as the area of resected specimen/dissection time (mm2/min). The resected specimen was flattened on the plate, and the length (mm) of its long and short axes were measured using a ruler. The circumferential length (mm) and resected area (mm2) were calculated using these measurements. En bloc resection was defined as resection in one-piece. The complete procedure rate was the proportion of the trainees who completed the ESD-C themselves. Perforation was defined as the stomach wall defect made using the CC during any ESD-C procedure.
We also investigated the factors associated with the difficulty of ESD including tumor location, tumor position, assistant skill, and resected area. The difficulty of ESD was defined as incompletion of ESD procedure, a long procedure time (≥ 20 min) or intraoperative perforation. Tumor location was classified into the middle third or lower third. Tumor position was classified into greater curvature or non-greater curvature. The assistant skill was classified into expert and non-expert. The resected area was classified into < 500 mm2 and ≥ 500 mm2.
A descriptive statistical analysis of data using the median and interquartile range and mean ± SD was employed. The two groups were compared using Fisher’s exact test for categorical variables and the Mann-Whitney U test for continuous variables. Univariate and multivariate analyses were conducted for evaluating the factors associated with the difficulty of ESD. P < 0.05 was considered statistically significant. All statistical analyses were performed using the JMP Pro software program (ver. 13.0; SAS Institute Inc., Cary, NC, United States).
The characteristics of the mock lesions treated by ESD-C are shown in Table 1. Regarding the lesion locations, 20 lesions were located in the middle third and 12 in the lower third of the stomach. Regarding the lesion positions, 19 lesions were positioned on the greater curvature, 9 on the anterior wall, and 4 on the posterior wall of the stomach. There were no significant differences between the ESD-C-E and ESD-C-NE groups regarding the lesion locations and positions. Similarly, there was no significant difference in the median tumor size between the two groups (314.00 mm2 [219.80-515.16] vs 310.86 mm2 [175.84-407.42], P = 0.75, respectively).
| All, n = 32 | Expert, (ESD-C-E), n = 16 | Non-expert, (ESD-C-NE), | P value | |
| Location, n (%) | 0.72 | |||
| Middle third | 20 (62.5) | 9 (56.2) | 11 (68.8) | |
| Lower third | 12 (37.5) | 7 (43.8) | 5 (31.2) | |
| Position, n (%) | 0.61 | |||
| Anterior wall | 9 (28.1) | 4 (25.0) | 5 (31.2) | |
| Posterior wall | 4 (12.5) | 1 (6.2) | 3 (18.8) | |
| Greater curvature | 19 (59.4) | 11 (68.8) | 8 (50.0) | |
| Marking size, mm2 | 0.75 | |||
| mean ± SD | 391.64 ± 288.63 | 408.54 ± 264.49 | 374.74 ± 318.76 | |
| Median (IQR) | 310.86 (184.08-461.78) | 314.00 (219.80-515.16) | 310.86 (175.84-407.42) |
Treatment outcomes of ESD-C are shown in Table 2. Sixteen operators performed 32 ESD-Cs on the porcine stomach model. All ESD-Cs achieved an en bloc resection. However, one trainee was replaced by the expert during the procedure in the ESD-C-NE group. Total procedure time and incision time were significantly shorter in the ESD-C-E group than in the ESD-C-NE group (total procedure time: 12.93 min [10.79-15.33] vs 21.90 min [18.50-26.36], P = 0.001; incision time: 7.04 min [5.57-8.28] vs 11.7 min [10.75-13.23], P < 0.001). However, there was no significant difference in dissection times between the two groups.
| Expert (ESD-C-E), n = 16 | Non-expert, (ESD-C-NE), n = 16 | P value | |
| En bloc resection, n (%) | 16 (100) | 16 (100) | - |
| Complete procedure, n (%) | 16 (100) | 15 (93.8) | 1 |
| Perforation, n (%) | 0 (0) | 0 (0) | - |
| Total procedure time, min | |||
| mean ± SD | 13.90 ± 4.49 | 24.31 ± 11.24 | 0.001a |
| Median (IQR) | 12.93 (10.79-15.33) | 21.90 (18.50-26.36) | |
| Incision time, min | < 0.001a | ||
| Median (IQR) | 7.04 (5.57-8.28) | 11.70 (10.75-13.23) | |
| Dissection time, min | 0.07 | ||
| Median (IQR) | 3.20 (2.18-5.17) | 5.09 (3.50-9.91) | |
| Circumferential length, mm | 0.88 | ||
| Median (IQR) | 74.85 (68.62-93.11) | 75.46 (66.73-86.59) | |
| Resected area, mm2 | 0.78 | ||
| Median (IQR) | 437.50 (324.75-688.50) | 451.00 (304.00-589.00) | |
| Incision speed, mm/min | 0.001a | ||
| Median (IQR) | 11.24 (9.61-12.94) | 6.72 (5.63-9.13) | |
| Dissection speed, mm2/min | 0.019a | ||
| Median (IQR) | 137.30 (120.17-167.72) | 75.66 (52.57-135.88) |
There was no significant difference in circumferential incision length and the resected area between the ESD-C-E and ESD-C-NE groups. Regarding the speed of the procedure, both incision and dissection speeds of the ESD-C-E group were significantly faster than those of the ESD-C-NE group.
Results of the univariate and multivariate analyses for evaluating the factors associated with the difficulty of ESD are shown in Table 3. In the univariate analysis, the assistant skill of non-experts and a resected area of ≥ 500 mm2 were the significant factors associated with the difficulty of ESD. Likewise, in the multivariate analysis, the assistant skill of non-experts (odds ratio [OR]: 16.5) and a resected area of ≥ 500 mm2 (OR: 15.3) remained independent factors associated with the difficulty of ESD.
| No. of patients | No. of events | Univariate | Multivariatea | |||||
| OR | 95%CI | P value | OR | 95%CI | P value | |||
| Location | 0.52 | 0.49 | ||||||
| Middle third | 20 | 9 | 1.64 | 0.37-7.25 | 2.09 | 0.17-12.3 | ||
| Lower third | 12 | 4 | 1 | Reference | 1 | Reference | ||
| Position | 0.60 | 0.73 | ||||||
| Non-GC | 13 | 6 | 1.47 | 0.35-6.17 | 0.68 | 0.08-5.73 | ||
| GC | 19 | 7 | 1 | Reference | 1 | Reference | ||
| Assistant skill | 0.016a | 0.021a | ||||||
| Non-expert | 16 | 10 | 7.22 | 1.44-36.20 | 16.5 | 1.52-178.00 | ||
| Expert | 16 | 3 | 1 | Reference | 1 | Reference | ||
| Resected area | 0.025a | 0.023a | ||||||
| ≥ 500 mm2 | 12 | 8 | 6.00 | 1.25-28.8 | 15.3 | 1.46-159.00 | ||
| < 500 mm2 | 20 | 5 | 1 | Ref. | 1 | |||
No studies have evaluated how assistant skill level affects the treatment outcomes of ESD-C in clinical practice due to ethical issues of assuring the safety of the ESD procedure. In this study, using an ex vivo porcine model, we evaluated the effects of the assistant skill level on the ESD-C procedure. We showed for the first time that ESD-C with expert assistants achieved a significantly shorter procedure time than that with non-expert assistants. The difficulty of ESD was significantly associated with the assistant skill level and the size of the resected area. The importance of the assistant’s skill level in ESD-C could be dependent on the unique feature of the CC, which is significantly different from the conventional endo-knives, including the needle-type and insulated-tip knives. The assistants for ESD procedures with conventional endo-knives only have to move the tip in or out during the ESD procedures, with no specific technical skills required[6,7]. In contrast, the assistants for ESD-C with a scissor-type knife require certain technical skills acquired by experience. They need to adjust the incision line or dissection line by rotating the endo-knife in an appropriate position, as well as close and open the knife to grasp and release the tissues[13]. As a result, the total procedure time of ESD-C-E was significantly shorter than that of ESD-C-NE in this study. We revealed that the assistant skill level is a key factor to influencing the procedure time. In fact, the assistance of a non-expert had the highest OR for the difficulty of ESD.
Consistent with the procedure time, there were significant differences in the incision time and speed between the ESD-C-E and ESD-C-NE groups. Although the dissection speed of ESD-C-E was significantly faster than that of ESD-C-NE, there was no significant difference in the dissection times between the two groups. This discrepancy could be explained by the following: The possible difference in the dissection time could be masked by some differences in the size of the resected area and tumor position between the two groups. In fact, the procedure time was associated not only with the assistant skill but also the size of the resected area shown by multivariate analysis. In addition, the dissection times might also be masked by application of the traction method, which played a role in the reduction of the dissection time in both groups[19,20].
One important finding is that a high completion rate was achieved in both groups in this study. Only one ESD-C procedure was incomplete in the ESD-C-NE group. The achievement of a high completion rate in ESD-C might be due to superiority of the CC over the conventional endo-knives in terms of safety, usability, and feasibility according to recent reports[12,15,16,21,22]. It has been indicated that the completion rate of ESD-C performed by a trainee is higher than that of ESD using conventional endo-knives[12]. Consistent with the result in our study, no perforation occurred during the ESD-C procedures in both groups. The usage of the CC might also contribute to preventing perforations. Since the CC allows us to grasp and release the target tissue at any time, the risk of unintentional perforation during ESD-C could be much lower than that when using conventional endo-knives. We should also mention that the traction method applied in all ESD-C procedures also plays a role in the reduction of the perforation risk. Indeed, traction-assisted ESD reduces perforation risk[20]. Taken together, ESD-C using the traction method is a very useful tool to achieve safe ESD with very few risks of intraprocedural perforation.
This study had several limitations. First, this study limited target lesions to 30 mm in size in the middle or lower thirds of the stomach because the mucosal layers in the upper third of the porcine stomach are too thick to perform the ESD-C procedure. Second, this was an ex vivo study using a porcine animal model without any blood flow. The ESD procedure-related complications, including intra/postoperative bleeding other than intraoperative perforation, could not be evaluated. Hemostasis in ESD-C can depend on the assistant skill level because the bleeding point must be properly grasped by the CC. We assume that the importance of the assistant skill in ESD-C found in this study would be more significant in clinical practice when performed on humans. Further studies in living animals or humans are required to assess such complications in the future. Third, all operators were non-experts with experience performing < 20 ESD cases. Therefore, it is unclear whether similar outcomes can be obtained in cases where all operators are replaced with experts. A validation study will be required to clarify this point. Forth, the manipulation by the assistant in ESD-C was different from that in ESD with other-types of knives such as needle-type and insulated-tip knives. It is unclear whether the results of this study could be applied to ESD with other-types of knives. Further studies using other-types of knives are required in the future.
In conclusion, we demonstrated the importance of the assistant skill level in ESD-C in an ex vivo porcine model. ESD-C with expert assistance could contribute to shorter procedure times. Assistance by experts has the additional benefit of providing supervision to trainees simultaneously. Furthermore, we believe that a quicker ESD procedure will be possible if an expert assistant is in charge, even in cases with experts in ESD.
A clutch cutter is used as a scissor-type endoscopic knife in endoscopic submucosal dissection (ESD) of gastrointestinal tract tumors. Assistant staff support operators to manipulate the endoscopic devices during the ESD procedure. ESD with the clutch cutter (ESD-C) required technical skills for assistant staff to rotate the device and grasp the target tissue.
It is unclear whether the skills of the assistant staff affect the technical outcomes of ESD-C.
The aim of this study was to investigate how the skills of the assistant staff may affect the technical outcomes of ESD-C.
A total of 32 ESD-Cs on mock lesions in an ex vivo porcine stomach model were performed by trainees: 16 ESD-Cs were assisted by an expert and the other 16 ESD-Cs were assisted by a non-expert. Technical outcomes were compared between the two groups.
ESD-Cs were assisted by an expert achieved significantly shorter procedure time, with high curability and low perforation rate compared to ESD-Cs were assisted by a non-expert. Assistant skill was significantly associated with the difficulty of ESD on multivariate analysis.
Assistant skill is an important factor when trainees perform ESD-C procedures.
This was an ex vivo porcine model study with small sample size. Validation study in human with large sample size is desired in the future.
The authors thank all members in the Kitakyushu ESD Hands-on Seminar and Tokyo ESD Hands-on Seminar for assisting with data collection. The authors thank Hiroko Fujisawa for creating illustrations. The authors thank Junji Kishimoto (Center for Clinical and Translational Research at Kyushu University Hospital) for reviewing the statistical methods of this study.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dai YC, Yu PF S-Editor: Zhang L L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Ono H, Yao K, Fujishiro M, Oda I, Nimura S, Yahagi N, Iishi H, Oka M, Ajioka Y, Ichinose M, Matsui T. Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer. Dig Endosc. 2016;28:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 406] [Article Influence: 45.1] [Reference Citation Analysis (0)] |
| 2. | Kitagawa Y, Uno T, Oyama T, Kato K, Kato H, Kawakubo H, Kawamura O, Kusano M, Kuwano H, Takeuchi H, Toh Y, Doki Y, Naomoto Y, Nemoto K, Booka E, Matsubara H, Miyazaki T, Muto M, Yanagisawa A, Yoshida M. Esophageal cancer practice guidelines 2017 edited by the Japan Esophageal Society: part 1. Esophagus. 2019;16:1-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 377] [Cited by in RCA: 390] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 3. | Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, Hisabe T, Yao T, Watanabe M, Yoshida M, Kudo SE, Tsuruta O, Sugihara KI, Watanabe T, Saitoh Y, Igarashi M, Toyonaga T, Ajioka Y, Ichinose M, Matsui T, Sugita A, Sugano K, Fujimoto K, Tajiri H. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015;27:417-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 435] [Article Influence: 43.5] [Reference Citation Analysis (0)] |
| 4. | Esaki M, Suzuki S, Ikehara H, Kusano C, Gotoda T. Endoscopic diagnosis and treatment of superficial non-ampullary duodenal tumors. World J Gastrointest Endosc. 2018;10:156-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Bhatt A, Abe S, Kumaravel A, Vargo J, Saito Y. Indications and Techniques for Endoscopic Submucosal Dissection. Am J Gastroenterol. 2015;110:784-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 6. | Ohkuwa M, Hosokawa K, Boku N, Ohtu A, Tajiri H, Yoshida S. New endoscopic treatment for intramucosal gastric tumors using an insulated-tip diathermic knife. Endoscopy. 2001;33:221-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 309] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 7. | Toyonaga T, Man-I M, Fujita T, Nishino E, Ono W, Morita Y, Sanuki T, Masuda A, Yoshida M, Kutsumi H, Inokuchi H, Azuma T. The performance of a novel ball-tipped Flush knife for endoscopic submucosal dissection: a case-control study. Aliment Pharmacol Ther. 2010;32:908-915. [PubMed] |
| 8. | Akahoshi K, Akahane H, Murata A, Akiba H, Oya M. Endoscopic submucosal dissection using a novel grasping type scissors forceps. Endoscopy. 2007;39:1103-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Akahoshi K, Okamoto R, Akahane H, Motomura Y, Kubokawa M, Osoegawa T, Nakama N, Chaen T, Oya M, Nakamura K. Endoscopic submucosal dissection of early colorectal tumors using a grasping-type scissors forceps: a preliminary clinical study. Endoscopy. 2010;42:419-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Akahoshi K, Honda K, Akahane H, Akiba H, Matsui N, Motomura Y, Kubokawa M, Endo S, Higuchi N, Oya M. Endoscopic submucosal dissection by using a grasping-type scissors forceps: a preliminary clinical study (with video). Gastrointest Endosc. 2008;67:1128-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Hayashi Y, Miura Y, Yamamoto H. Pocket-creation method for the safe, reliable, and efficient endoscopic submucosal dissection of colorectal lateral spreading tumors. Dig Endosc. 2015;27:534-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Dohi O, Yoshida N, Terasaki K, Azuma Y, Ishida T, Kitae H, Matsumura S, Ogita K, Takayama S, Mizuno N, Nakano T, Hirose R, Inoue K, Kamada K, Uchiyama K, Ishikawa T, Takagi T, Kishimoto M, Konishi H, Naito Y, Itoh Y. Efficacy of Clutch Cutter for Standardizing Endoscopic Submucosal Dissection for Early Gastric Cancer: A Propensity Score-Matched Analysis. Digestion. 2019;100:201-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Akahoshi K, Akahane H, Motomura Y, Kubokawa M, Itaba S, Komori K, Nakama N, Oya M, Nakamura K. A new approach: endoscopic submucosal dissection using the Clutch Cutter® for early stage digestive tract tumors. Digestion. 2012;85:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Otsuka Y, Akahoshi K, Yasunaga K, Kubokawa M, Gibo J, Osada S, Tokumaru K, Miyamoto K, Sato T, Shiratsuchi Y, Oya M, Koga H, Ihara E, Nakamura K. Clinical outcomes of Clutch Cutter endoscopic submucosal dissection for older patients with early gastric cancer. World J Gastrointest Oncol. 2017;9:416-422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (2)] |
| 15. | Hayashi Y, Esaki M, Suzuki S, Ihara E, Yokoyama A, Sakisaka S, Hosokawa T, Tanaka Y, Mizutani T, Tsuruta S, Iwao A, Yamakawa S, Irie A, Minoda Y, Hata Y, Ogino H, Akiho H, Ogawa Y. Clutch Cutter knife efficacy in endoscopic submucosal dissection for early gastric neoplasms. World J Gastrointest Oncol. 2018;10:487-495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Esaki M, Hayashi Y, Ikehara H, Ihara E, Horii T, Tamura Y, Ichijima R, Yamakawa S, Irie A, Shibuya H, Suzuki S, Kusano C, Minoda Y, Akiho H, Ogawa Y, Gotoda T. The effect of scissor-type vs non-scissor-type knives on the technical outcomes in endoscopic submucosal dissection for superficial esophageal cancer: a multi-center retrospective study. Dis Esophagus. 2020;33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Yamamoto S, Uedo N, Ishihara R, Kajimoto N, Ogiyama H, Fukushima Y, Yamamoto S, Takeuchi Y, Higashino K, Iishi H, Tatsuta M. Endoscopic submucosal dissection for early gastric cancer performed by supervised residents: assessment of feasibility and learning curve. Endoscopy. 2009;41:923-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 134] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 18. | Yoshida M, Kakushima N, Mori K, Igarashi K, Kawata N, Tanaka M, Takizawa K, Ito S, Imai K, Hotta K, Ishiwatari H, Matsubayashi H, Ono H. Learning curve and clinical outcome of gastric endoscopic submucosal dissection performed by trainee operators. Surg Endosc. 2017;31:3614-3622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Suzuki S, Gotoda T, Kobayashi Y, Kono S, Iwatsuka K, Yagi-Kuwata N, Kusano C, Fukuzawa M, Moriyasu F. Usefulness of a traction method using dental floss and a hemoclip for gastric endoscopic submucosal dissection: a propensity score matching analysis (with videos). Gastrointest Endosc. 2016;83:337-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 94] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 20. | Yoshida M, Takizawa K, Suzuki S, Koike Y, Nonaka S, Yamasaki Y, Minagawa T, Sato C, Takeuchi C, Watanabe K, Kanzaki H, Morimoto H, Yano T, Sudo K, Mori K, Gotoda T, Ono H; CONNECT-G Study Group. Conventional vs traction-assisted endoscopic submucosal dissection for gastric neoplasms: a multicenter, randomized controlled trial (with video). Gastrointest Endosc. 2018;87:1231-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 116] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 21. | Akahoshi K, Motomura Y, Kubokawa M, Gibo J, Kinoshita N, Osada S, Tokumaru K, Hosokawa T, Tomoeda N, Otsuka Y, Matsuo M, Oya M, Koga H, Nakamura K. Endoscopic Submucosal Dissection for Early Gastric Cancer using the Clutch Cutter: a large single-center experience. Endosc Int Open. 2015;3:E432-E438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Akahoshi K, Akahane H. A new breakthrough: ESD using a newly developed grasping type scissor forceps for early gastrointestinal tract neoplasms. World J Gastrointest Endosc. 2010;2:90-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |