Published online Nov 27, 2021. doi: 10.4240/wjgs.v13.i11.1497
Peer-review started: February 8, 2021
First decision: March 30, 2021
Revised: April 1, 2021
Accepted: September 2, 2021
Article in press: September 2, 2021
Published online: November 27, 2021
Processing time: 291 Days and 12.2 Hours
The omentum is an organ that is easily sacrificed during abdominal surgery. The scope of omentectomy and whether a routine omentectomy should be performed are still unknown.
To review the literature in order to determine the physiological functions of the omentum and the roles it plays in pathological events in order to reveal the necessity for removal and preservation of the omentum.
A clinical review of the English language literature based on the MEDLINE (PubMed) database was conducted using the keywords: “abdomen”, “gastrointestinal”, “tumor”, “inflammation”, “omental flap”, “metastasis”, “omentum”, and “omentectomy”. In addition, reports were also identified by systematically reviewing all references in retrieved papers.
The omentum functions as a natural barrier in areas where pathological processes occur in the abdominal cavity. The omentum limits and controls inflammatory and infectious pathologies that occur in the abdomen. It also aids in treatment due to its cellular functions including lymphatic drainage and phagocytosis. It shows similar behavior in tumors, but it cannot cope with increasing tumor burden. The stage of the disease changes due to the tumor mass it tries to control. Therefore, it is considered an indicator of poor prognosis. Due to this feature, the omentum is one of the first organs to be sacrificed during surgical procedures. However, there are many unknowns regarding the role and efficacy of the omentum in cancer.
The omentum is a unique organ that limits and controls inflammatory processes, foreign masses, and lesions that develop in the abdominal cavity. Omental flaps can be used in all anatomical areas, including the thorax, abdomen, pelvis, and extremities. The omentum is an organ that deserves the title of the abdominal policeman. It is generally accepted that the omentum should be removed in cases where there is tumor invasion. However, the positive or negative contribution of omental resection in the treatment of abdominal pathologies should be questioned.
Core Tip: The omentum is a unique organ that monitors and controls inflammatory processes, foreign masses, and lesions that develop in the abdominal cavity. Omental flaps can be used in all anatomical areas, including the thorax, abdomen, pelvis, and extremities. The omentum is an organ that deserves the title of the abdominal policeman. It is generally accepted that the omentum should be removed in cases where there is tumor invasion. However, the positive or negative contribution of omental resection in the treatment of abdominal pathologies should be questioned.
- Citation: Atay A, Dilek ON. Is omentectomy necessary in the treatment of benign or malignant abdominal pathologies? A systematic review. World J Gastrointest Surg 2021; 13(11): 1497-1508
- URL: https://www.wjgnet.com/1948-9366/full/v13/i11/1497.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i11.1497
The omentum is the first organ to be removed in cases scheduled for cytoreductive surgery (CRS). It is an organ that is easily sacrificed during various abdominal surgeries. The omentum is very effective in defending the body against pathogens as well as injuries. It is also considered to be an immunological organ[1,2].
The omentum can reach all parts of the abdomen[1-3]. It has an extensive lymphatic-functioning cellular network of mesenchymal cells, also called milky spots. Milky spots are primitive lymphatic tissue rich in macrophages and lymphocytes clustered around capillaries. These cells function as lymphoid tissue[4]. For example, this mechanism is found in many cases such as plastron appendicitis, diverticulitis, cholecystitis and so on. Milky spots capture antigens, and pathogenic organisms that are released into the peritoneum. Lymphatic ducts then remove them from the environment[2,5,6]. Nevertheless, when the tumor load increases, this system does not function well and becomes insufficient. An increase in tumor volume results in seeding to the omentum. This, in turn, causes tumor growth and nodular forms emerge due to the "polypeptide growth hormone" secreted by macrophages. Attachment and growth of tumor cells is also facilitated by another factor: The "angiogenesis factor" which is secreted from the omentum[2,6]. It not only allows formation of adhesives and neovascularization, but also protects the body and the organ against damage due to radiation. According to Morrison, the omentum is the "abdominal policeman"[1]. It tries to control the process by turning it into a local inflammation site. In cases with progression towards infection, the omentum attempts to control the progress by forming an abscess. This is a mechanism that is seen in diverticulitis, cholecystitis, and plastron appendicitis.
The omentum is a unique organ due to its extraordinary functional properties in the abdomen, but the reasons for its frequent removal rather than preservation by surgeons have been questioned, according to literature data. With this aim, clinical retrospective and prospective studies have been carried out as well as experimental studies. A review of the English language literature based on a MEDLINE (PubMed) database was conducted using the keywords: “Abdomen”, “gastrointestinal”, “tumor”, “inflammation”, “omental flap”, “metastasis”, “omentum”, and “omentectomy”. In addition, reports were also found by systematically reviewing all references in retrieved papers.
Our literature search of MEDLINE found 1305 articles with the keyword "omentectomy". Articles related to the gastrointestinal system were separated with the help of other keywords. It was found that most of the articles were on gynecological (n = 519), stomach (n = 121), colorectal (n = 104), and appendix (n = 52) pathologies and were mostly related to tumors. Articles related to the gastrointestinal system were evaluated. A brief review of its use in the treatment or reconstruction of all other clinical pathologies was also included in this article. Interestingly, 1623 articles were identified with the keyword "omental flap". That is an interesting finding as it shows that the properties of the omentum are being used more.
Experimental studies in rats indicated that the omentum displays angiogenic activity. Myofibroblasts in the wound area multiply due to increased blood supply. This, in return, promotes the healing process[7]. Nevertheless, another study showed just the opposite: In gastric ulcer-generated and omentectomy rats, the healing of ulcers was accelerated[8]. This contradiction indicates the need for further clinical studies on this subject.
Studies show that excess fat in the internal organs causes metabolic syndrome. In an experimental study, overweight rats subjected to omentectomy showed that nonalcoholic fatty liver, and metabolic syndrome were prevented[9]. C-reactive protein and interleukin-6 are believed to mediate the omentum, which results in leptin resistance and induces obesity.
Tumor behavior with or without the omentum has been a topic of several studies. In an experimental study by Lawrance et al[6] in rats, tumors were detected in the colon and omentum of 38% and 43% of rats, respectively, that underwent colon resection and anastomosis, and intraluminal injection of tumor cells. When the same procedure was repeated in the omentectomy group, tumors developed in 14% and 9% of rats in the anastomosis and abdominal cavity, respectively. While 53% and 79% of rats developed tumors in the anastomosis and abdominal cavity (omentum), respectively, in the groups intraperitoneally injected with tumor cells, and these rates were found to be 16% and 29%, respectively, in the omentectomy group. The omentum is believed to have a capturing function to collect and cover tumor cells, especially colon tumors. On the other hand, studies have reported that omentectomy rats developed fewer tumors (26%), as in an experimental colon cancer model performed by Weese et al[10]. Yokoyama et al[11] proposed that removal of the omentum with metastases would cause not only relapse but also tumor spread.
It was determined that dogs who underwent pancreatic resection and whose pancreatic duct were left open, and who underwent omentectomy had reduced survival, but those who did not undergo omentectomy lived much longer[12].
An experimental study on the role of omentectomy in the formation of adhesions suggested that rats subjected to omentectomy had a lower level of plasminogen activator and higher adhesions[13].
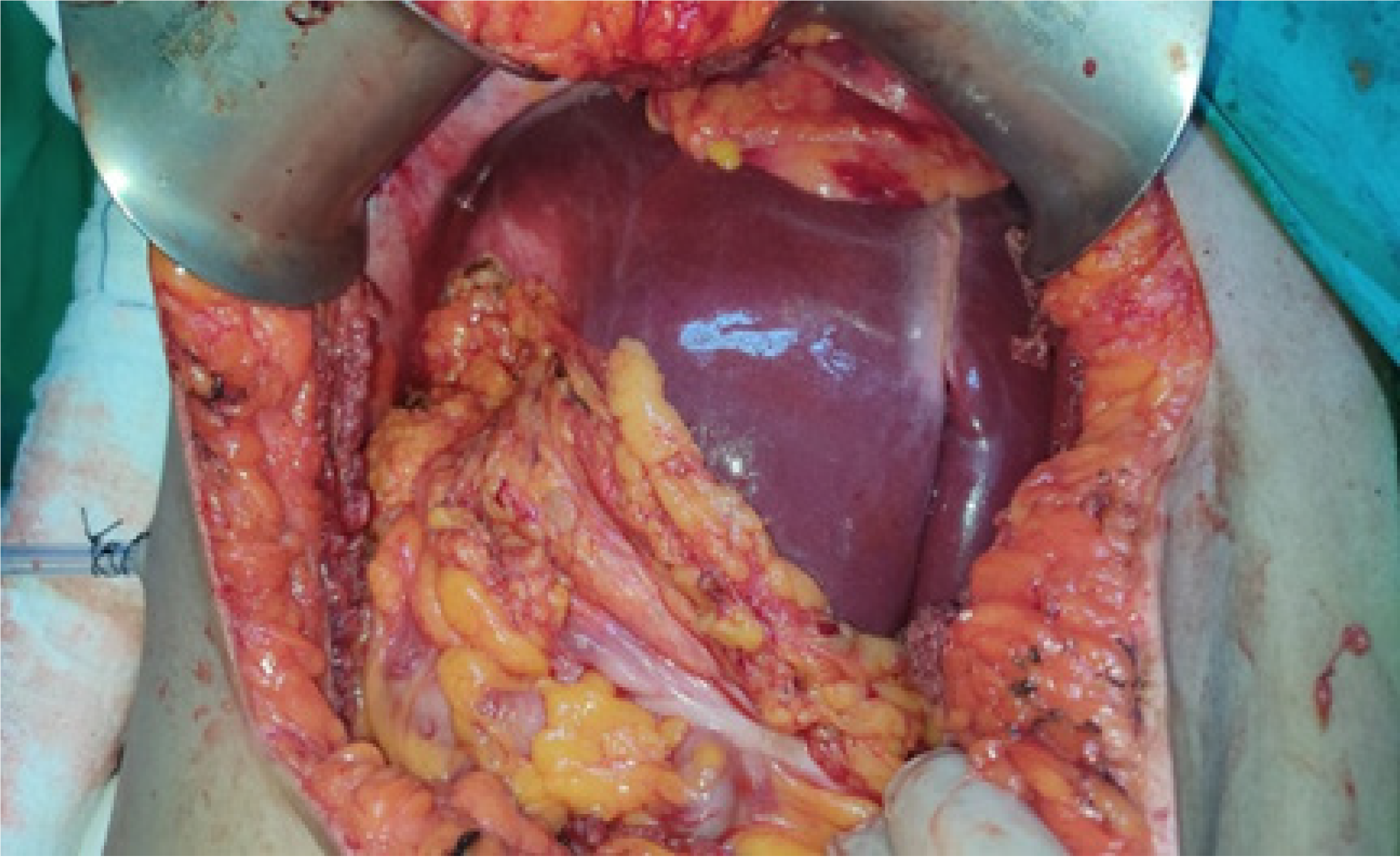
Gastrointestinal tumors: The first areas of attachment of tumors beyond the serosa, especially gastric tumors, are the peritoneal surfaces and the omentum. The omentum captures and surrounds (capturing function) any antigenic lesion in the abdominal cavity[3,6] (Figure 1). There are several studies that disagree on the necessity of omentectomy in gastric tumors. D2/modified D2 dissection is performed as a standard procedure in patients with stomach cancer. Barchi et al[14] in their series of 284 patients who underwent omentectomy, D2 dissection, and gastrectomy due to stomach cancer, found omental metastasis in only five patients (1.8%). They determined that omental metastasis prevalence was higher in patients who had T3-T4 lesions. They recommended avoiding omentectomy in patients with T1--2M0 tumors (diameter < 5.2 cm). They also stated that tumors in the greater omentum lymph nodes were more common in advanced stages of the disease. Hasegawa et al[15] studied 330 patients who had advanced-stage gastric tumors. They did not detect a statistical difference between the groups with omentum-sparing gastrectomy and gastric tumor and those who underwent omentectomy. In their study of 100 patients with gastric tumor, Jongerius et al[16] reported that 5% of the patients had omental metastases, and these were patients with T3 and T4 lymph node involvement. Moreover, they reported that the probability of omental metastasis in patients who were considered operable as a result of preoperative evaluations was very low and that omentectomy was not required during radical gastrectomy. Kim et al[17] reported that there was no significant difference between the groups after 38 mo of follow-up in their gastric tumor series of 37 cases who underwent partial (n = 17) or total omentectomy (n = 20).
Kurokawa et al[18] conducted a multicentric study involving 1204 patients with gastric tumor recruited from 57 hospitals. They divided the patients with gastric resection and D2 dissection into two groups: Omentectomy or bursectomy. They observed no significant difference between the groups concerning their 5-year survival rates. They also concluded and recommended D2 dissection and omentectomy as the routine approach for the surgical treatment of gastric cancer. Bursectomy is not routinely performed as it causes more complications such as fistula and bleeding and does not provide an advantage in terms of survival. For this reason, it is only performed in patients who suffer from posterior gastric wall tumors. On the other hand, there are also studies in the literature suggesting preservation of the omentum in patients with T1-T2 gastric cancer (M0). In advanced cases, however, there is a need for prospective clinical trials; because surgeons tend to perform radical surgery and omentectomy in advanced cases. In tumors with peritoneal involvement, such as pseudomyxoma peritonei, complete CRS can significantly contribute to survival. It can be an aggressive operation that involves organ resection and omentectomy[19].
Colon and rectum: There is a belief among surgeons that the remaining omentum after colectomy will cause adhesions in the small intestine. However, studies refute this. Ambroze et al[20] demonstrated that this belief was incorrect in their large series of colectomy, ileoanal anastomosis, and omentectomy. They observed no significant difference in ileus.
CRS is also performed to eliminate the macroscopic and microscopic spread of colorectal cancers. In a large data analysis performed by Bonnefoy et al[21], they found that 71% of patients in the colorectal cancer series of 337 cases who underwent total omentectomy had macroscopic omental metastasis. They also found that 17% of patients without macroscopic omental metastases had microscopic metastases in the omentum. They recommend routine omentectomy in colorectal cancer cases with peritoneal metastasis. Complete supracolic omentectomy is recommended as part of CRS, especially in mucinous type colorectal cancer[22].
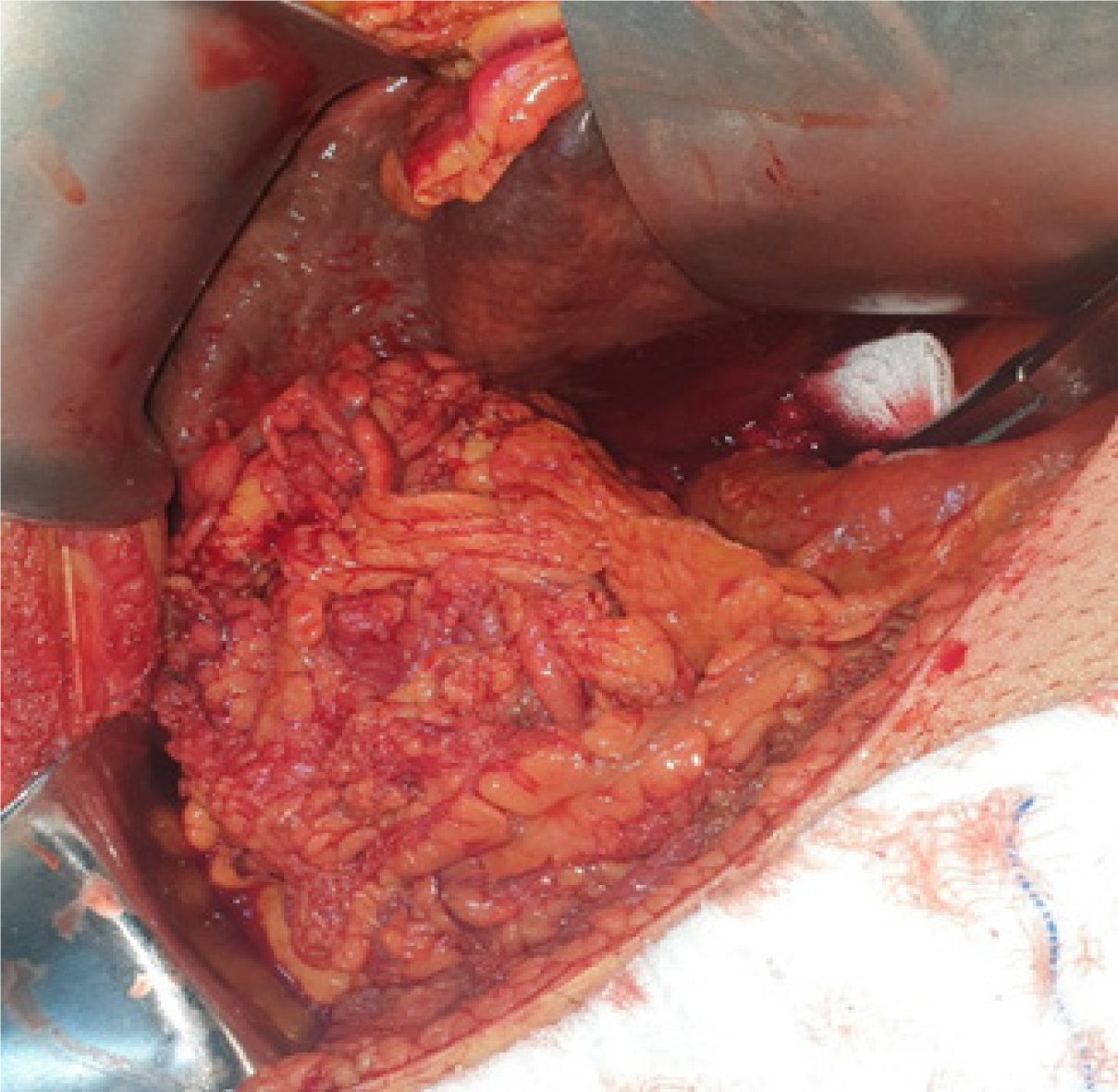
Hepato-pancreato-biliary: The omentum may be involved in many benign and malignant pathologies of the liver. In inflammatory liver lesions, the omentum adheres to the lesion and tries to limit it. In peripheral tumors and after liver surgery, the omentum may adhere to the liver and form new collaterals. The omentum is one of the two organs that most commonly form a collateral circulation with the liver. Because the omentum is free and mobile, it can reach every segment of the liver. It may contribute to the blood supply and venous drainage with collaterals that develop in cirrhotic or tumor patients[23]. Chu et al[24] reported that new collaterals developed in patients with portal hypertension who underwent partial splenectomy and retrosternal omental flap fixation to prevent complications due to esophageal varices and may be effective against hemostasis and hypersplenism. Studies suggest repetitive aggressive surgeries and adding omentectomy to the procedure in patients with ruptured hepatocellular carcinoma[25]. The omentum can also be used to fill cavities (omentoplasty) that occur during the treatment of liver hydatid cysts (Figure 2)[26].
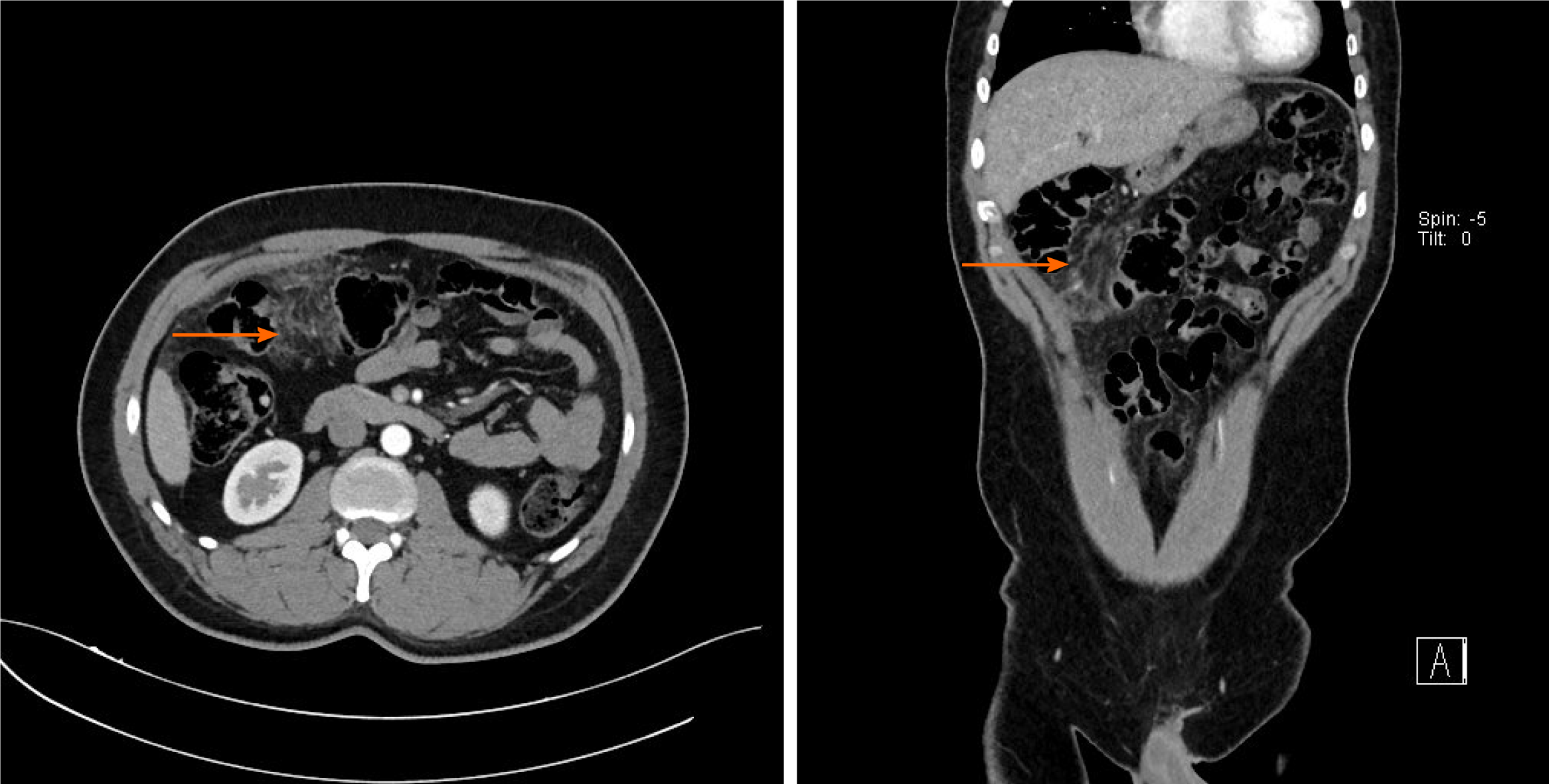
In acute cholecystitis, the omentum surrounding the inflamed gallbladder is commonly seen (Figure 3). As in acute appendicitis, the omentum surrounding the gallbladder during cholecystitis attacks may form permanent adhesions even with regression of inflammation. In the case of progression of the inflammatory process and perforation of the gallbladder, it can contribute to pericholecystic abscess formation, keep the infection local, and prevent the spread of infection. Cases in which bile duct injury developed and the resulting defect was closed with an omentum flap have also been reported in the literature[27].
Omentectomy has no place in the surgery of pancreatic tumors. However, it is often added to the procedure, especially in locally advanced distal pancreatic tumors[28]. Although different results have been found when the anastomosis is wrapped with an omental flap in patients who underwent pancreaticoduodenectomy, a recent meta-analysis reported that an omental wrap might be beneficial in reducing complications[29].
Appendix: Appendectomy is the only treatment option in acute or perforated appendicitis. However, the management of plastron appendicitis bordered and surrounded by the omentum is different. Plastron appendicitis occurs in 6% of appendicitis cases. The omentum is the organ that makes the most significant contribution to plastron formation. In plastron appendicitis, which manifests as a mass in the right lower quadrant, the omentum limits the inflammatory process and tries to keep it under control. A conservative approach is the first option in patients with plastron appendicitis. However, the presence of tumors and inflammatory bowel diseases that can mimic appendicitis should be investigated with colonoscopy and computed tomography (CT) imaging in healed patients[30].
Complete omental resection is performed as a routine procedure in patients who have decided to undergo CRS. In addition to appendectomy, cecectomy, right hemicolectomy, and lymph node dissections are also performed in epithelial tumors of the appendix[31,32]. On the other hand, pseudomyxoma peritonei (PMP) is one of the most lethal complications of appendix tumors. PMP is seen in 9% of low-grade tumors, and it is reported that PMP develops in 67.9% of perforated mucinous neoplasms. CRS and hyperthermic intraperitoneal chemotherapy are also recommended for appendiceal neoplasms[33,34].
Bariatric surgery: Bariatric surgery for obesity is one of the most performed procedures in the last two decades. Gastrointestinal resections and bypass procedures are the most preferred methods. Meta-analyses have reported that adding omentectomy to the procedure during bariatric surgery has no positive contribution other than a minimal reduction in body mass index[35]. Another study indicated that omentectomy included in Roux-en-Y gastric bypass (RYGB) surgery was not successful in reducing insulin resistance. There is literature concerning metabolically positive feedbacks in similar cases in which omentectomy was included in the RYGB. Still there is a need for extensive and prospective studies[36].
Reconstruction tool: The omentum promotes healing in the areas where it is placed and in surrounding organs and facilitates the recovery of function. Omental free flaps can be used in all anatomical areas, including the thorax, abdomen, and pelvis[37]. Fistulas are a well-known entity that can cause very complex problems and have a high risk of morbidity and mortality.
The omentum can be used to seal, shield, wrap, to fill any defects, especially peptic ulcer perforations. Placing and fixing the omental flap in the perforation area (Graham’s repair) in peptic ulcer perforations is a method that has been known since 1937 and is still in use[38,39]. It has been reported that a falciform ligament was used to close the perforation in a patient who underwent total omentectomy for intraabdominal tumors and developed peptic ulcer perforation over time[40]. Several clinical studies have investigated the contribution of the omentum to healing following it being wrapped around the anastomosis. Studies have reported that wrapping intrathoracic esophagogastric anastomoses with the omentum decreases complications such as anastomosis opening and stricture development. In an esophagectomy series of 255 cases by Dai et al[38], fewer complications were reported in the group in which the omentum was wrapped around the anastomosis. In their study of 171 cases of colon resection in which anastomoses were protected by omental wrapping, Agnifili et al[41] observed a positive impact of omental wraps. They concluded that omentectomy should not be performed in colorectal surgery.
Gynecological tumor surgery: Gynecological tumor surgery is one of the most common abdominal operations with omentectomy. Surgeons tend to prefer aggressive resection during laparotomy due to peritonitis carcinomatosis-like appearance. Specifically, omentectomy has a significant role in staging of endometrium- and ovarian-origin tumors[42-44]. In gynecological tumors, omental involvement is observed in 9%-37.5% of cases[45-47]. Involvement of the omentum indicates a poor prognosis. In order to reduce the tumor burden, omentectomy is added to the procedures during CRS. Nevertheless, the contribution of omentectomy to survival is still debated. As omental involvement is minimal in early-stage tumors, omentectomy does not affect survival. Therefore, unless there is macroscopic involvement, omentectomy should be avoided[48]. In the early stages, random omental biopsies can help in reliable staging.
Adhesions: Adhesions are the most common complications after abdominal surgery. The omentum has a tendency to gravitate towards areas of surgery. In their study, Ariake et al[49] focused on 113 patients who underwent surgery due to intestine obstruction caused by adhesions. In the 5-year follow-up, they observed that in 18 patients (20.8%) the ileus recurred. They also found that 54.5% of the patients with omentectomy and 21.3% without omentectomy developed ileus. This indicates that omentectomy may be considered a risk factor for ileus formation.
(1) Capturing function: The omentum also has a capturing function. The omentum tries to limit foreign bodies that remain or emerge in the abdominal cavity after surgery by surrounding them. It wraps the stones that are spilled from the gallbladder during cholecystectomies. It can also turn them into an inflammatory mass[50]. The tracing of stones without clinical symptoms is possible. However, due to rarely spilled stones, abscesses originating from the omentum may become a fistula. In such cases, without omentectomy, drainage may suffice.
(2) Shielding system: A shielding system (omental spacer) using the omentum may help prevent complications such as radiation enteritis, which is a severe pelvic irradiation complication. Yamada et al[51] reported that the created omental spacer was very useful in preventing radiation to the intestines.
(3) Hernia incarceration: The most important prognostic factor of hernia incarceration is hernia content. With penetration of the omentum into the hernia sac, the possibility of strangulation of the intestines decreases (Figure 4). In a study of 2184 pediatric patients, the rate of incarcerated hernia was 1.6%. Intestine (62%) and omentum (12%) were the most common organs in the hernia sac. Partial bowel resection was reported in four cases, and partial omentectomy in only 2 cases[52].
Omental torsion and necrosis: Omental torsion and necrosis are infrequent entities which can mimic many clinical pathologies. Abdominal CT is helpful in the diagnosis. In patients who do not recover following medical treatment (Figure 5), surgery can resolve the problem. Therefore, in cases who undergo exploration, the laparoscopic approach should be the first option. Some surgeons also want to perform an appendectomy while laparoscopically resecting the omental necrosis[53].
The omentum also limits and controls infections. If the infection has caused too much damage to the omentum, omentectomy may be necessary. In the literature, there are cases where laparotomy was performed for abscesses due to melioidosis (Burkholderia pseudomallei). As the mass detected during laparotomy and lesions in the omentum resemble a tumor implant, the tendency to perform omentectomy increases. Omental involvement in patients with abdominal tuberculosis may mimic ovarian tumor[54,55]. In order to prevent unnecessary radical surgical resection, it is more appropriate to perform laparoscopic exploration and biopsy first.
Some clinical studies have shown that omentectomy affects inflammation-related genes. A clinical study by Tamboli et al[56] observed that inflammation in skeletal muscles decreased after RYGB surgery, which was greater in those who also underwent omentectomy. Adding omentectomy to a partial jejunal resection in patients with metabolic syndrome resulted in better-controlled type 2 diabetes mellitus[57].
Peritoneal dialysis catheter (Tenckhoff catheter) dysfunction is a common problem in nephrology clinics (23%-36%). Among its most commonly reported causes are malposition and omental wrap. There are reports indicating that partial omentectomy in some patients with catheter dysfunction contributes to the dialysis catheter being more functional. On the contrary, in another clinical study involving 154 patients with peritoneal dialysis catheters, it was concluded that omentectomy had no contribution to catheter occlusion[58].
The use of omental flaps and lymph nodes in the treatment of lymphedema can significantly contribute to patients' quality of life and wound healing[59].
As in peptic ulcer perforation and selected cases with bile duct trauma, many case reports have undergone reconstruction with an omental flap for the treatment of bronchopleural fistula[60].
The omentum is a unique organ with unlimited mobility and protective physiological properties in the abdomen. However, this does not prevent the omentum from being one of the first organs to be sacrificed in radical abdominal surgery. Omental flaps can be used in all anatomical areas, including the thorax, abdomen, pelvis, and extremities. It is an organ that is first affected by inflammatory and pathological events that occur in the abdominal cavity, limits developing pathological processes, and tries to control them, saving treatment time.
The omentum is called the “abdominal policeman”. It limits and controls inflammatory and infectious pathologies, and thus contributes to patient survival. It shows similar behavior in tumors, but it cannot cope with increasing tumor burden and the stage of the disease changes due to the tumor mass it tries to control, and therefore it is considered an indicator of poor prognosis. Experimental and clinical studies are needed to determine the behavior of the omentum in different pathological conditions. During this process, the effect of omental resection on morbidity, mortality and survival in the treatment of abdominal pathologies should be carefully calculated in each case.
The omentum is an organ that is easily sacrificed during various abdominal surgeries. It is one of the first organs to be removed in cases scheduled for cytoreductive surgery.
As it plays an effective role in defense against pathogens and injuries, the omentum is classified as an immunological organ. It can also reach almost anywhere in the abdomen.
The omentum is a unique organ due to its extraordinary functional properties in the abdomen, but the reasons for its frequent removal rather than preservation by surgeons have been questioned in the light of literature data.
A review of the English language literature based on the MEDLINE (PubMed) database was conducted using the keywords “abdomen”, “gastrointestinal”, “tumor”, “inflammation”, “omental flap”, “metastasis”, “omentum”, and “omentectomy”.
Our literature search found 1305 articles with the keyword “omentectomy”. It was found that most of the articles were on gynecological (n = 519), stomach (n = 121), colorectal (n = 104), and appendix (n = 52) pathologies and were mostly related to tumors. A brief review of its use in the treatment or reconstruction of other clinical pathologies was also included in this article.
The omentum tries to limit and control inflammatory and pathological events that occur in the abdomen. As it limits and controls inflammatory and infectious pathologies, it contributes to the survival of the patient.
The omentum is not an organ that can be easily sacrificed at random. Experimental and prospective clinical studies on the control of tumor spread, control of infection, adhesion formation and the protective role of the omentum in patients undergoing omentectomy are needed.
All the figures in the article were obtained from Professor Osman Nuri Dilek's private archive.
Provenance and peer review: Invited article; Externally peer reviewed.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shetiwy M S-Editor: Wang JJ L-Editor: Webster JR P-Editor: Li JH
| 1. | Platell C, Cooper D, Papadimitriou JM, Hall JC. The omentum. World J Gastroenterol. 2000;6:169-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 72] [Reference Citation Analysis (0)] |
| 2. | Meza-Perez S, Randall TD. Immunological Functions of the Omentum. Trends Immunol. 2017;38:526-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 239] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 3. | Liebermann-Meffert D. The greater omentum. Anatomy, embryology, and surgical applications. Surg Clin North Am. 2000;80:275-293, xii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 159] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Ma T, Liu T. [Immunological characteristics of peritoneal cavity and intra-abdominal infection]. Zhonghua Wei Chang Wai Ke Za Zhi. 2018;21:1347-1350. [PubMed] |
| 5. | Koppe MJ, Nagtegaal ID, de Wilt JH, Ceelen WP. Recent insights into the pathophysiology of omental metastases. J Surg Oncol. 2014;110:670-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Lawrance RJ, Loizidou M, Cooper AJ, Alexander P, Taylor I. Importance of the omentum in the development of intra-abdominal metastases. Br J Surg. 1991;78:117-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Konturek SJ, Brzozowski T, Majka I, Pawlik W, Stachura J. Omentum and basic fibroblast growth factor in healing of chronic gastric ulcerations in rats. Dig Dis Sci. 1994;39:1064-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Ulven AJ, Romslo I, Varhaug JE, Svanes K. Reduced mucosal blood flow and acid secretion related to accelerated healing of gastric ulcer in rats after omentectomy including partial gastric devascularization. Eur Surg Res. 1979;11:154-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | García-Ruiz I, Solís-Muñoz P, Fernández-Moreira D, Grau M, Muñoz-Yagüe MT, Solís-Herruzo JA. Omentectomy Prevents Metabolic Syndrome By Reducing Appetite and Body Weight In A Diet-Induced Obesity Rat Model. Sci Rep. 2018;8:1540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Weese JL, Ottery FD, Emoto SE. Does omentectomy prevent malignant small bowel obstruction? Clin Exp Metastasis. 1988;6:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Yokoyama Y, Hirakawa H, Wang H, Mizunuma H. Is omentectomy mandatory in the operation for ovarian cancer? Eur J Obstet Gynecol Reprod Biol. 2012;164:89-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Traverso LW, MacFarlane SK. Pancreatic juice in the peritoneal cavity: antibiotics or omental preservation prevent mortality. J Surg Res. 1987;43:220-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Cerci C, Eroglu E, Sutcu R, Celikbas B, Kilbas A. Effects of omentectomy on the peritoneal fibrinolytic system. Surg Today. 2008;38:711-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Barchi LC, Ramos MFKP, Dias AR, Yagi OK, Ribeiro-Júnior U, Zilberstein B, Cecconello I. TOTAL OMENTECTOMY IN GASTRIC CANCER SURGERY: IS IT ALWAYS NECESSARY? Arq Bras Cir Dig. 2019;32:e1425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Hasegawa S, Kunisaki C, Ono H, Oshima T, Fujii S, Taguri M, Morita S, Sato T, Yamada R, Yukawa N, Rino Y, Masuda M. Omentum-preserving gastrectomy for advanced gastric cancer: a propensity-matched retrospective cohort study. Gastric Cancer. 2013;16:383-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Jongerius EJ, Boerma D, Seldenrijk KA, Meijer SL, Scheepers JJ, Smedts F, Lagarde SM, Balague Ponz O, van Berge Henegouwen MI, van Sandick JW, Gisbertz SS. Role of omentectomy as part of radical surgery for gastric cancer. Br J Surg. 2016;103:1497-1503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 17. | Kim MC, Kim KH, Jung GJ, Rattner DW. Comparative study of complete and partial omentectomy in radical subtotal gastrectomy for early gastric cancer. Yonsei Med J. 2011;52:961-966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Kurokawa Y, Doki Y, Mizusawa J, Terashima M, Katai H, Yoshikawa T, Kimura Y, Takiguchi S, Nishida Y, Fukushima N, Iwasaki Y, Kaji M, Hirao M, Katayama H, Sasako M. Bursectomy versus omentectomy alone for resectable gastric cancer (JCOG1001): a phase 3, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol. 2018;3:460-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 103] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 19. | Cazauran JB, Lasseur A, Pasquer A, Rousset P, Guedj J, Passot G, Glehen O. Total Mesenteric Peritonectomy for Peritoneal Metastases (with video). Ann Surg Oncol. 2017;24:3988-3989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Ambroze WL Jr, Wolff BG, Kelly KA, Beart RW Jr, Dozois RR, Ilstrup DM. Let sleeping dogs lie: role of the omentum in the ileal pouch-anal anastomosis procedure. Dis Colon Rectum. 1991;34:563-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Bonnefoy I, Mohamed F, Bonnot PE, Benzerdjeb N, Isaac S, Cotte E, Glehen O, Passot G. Risk of Omental Metastases in Patients Undergoing Cytoreductive Surgery for Colorectal Peritoneal Metastases. Dis Colon Rectum. 2020;63:1251-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Milito P, Battaglia L, Cosimelli M, Antista M, Guaglio M, Deraco M, Baratti D. Management and complete resection of peritoneal and bone metastases from mucinous rectal carcinoma. Tumori. 2020;300891620977695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Cheng LF, Ma KF, Fan WC, Yung AW, Li TM, Wong CS. Hepatocellular carcinoma with extrahepatic collateral arterial supply. J Med Imaging Radiat Oncol. 2010;54:26-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Chu H, Han W, Wang L, Xu Y, Jian F, Zhang W, Wang T, Zhao J. Long-term efficacy of subtotal splenectomy due to portal hypertension in cirrhotic patients. BMC Surg. 2015;15:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 25. | Ryu JK, Lee SB, Kim KH, Yoh KT. Surgical treatment in a patient with multiple implanted intraperitoneal metastases after resection of ruptured large hepatocellular carcinoma. Hepatogastroenterology. 2004;51:239-242. [PubMed] |
| 26. | Gomez I Gavara C, López-Andújar R, Belda Ibáñez T, Ramia Ángel JM, Moya Herraiz Á, Orbis Castellanos F, Pareja Ibars E, San Juan Rodríguez F. Review of the treatment of liver hydatid cysts. World J Gastroenterol. 2015;21:124-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 91] [Cited by in RCA: 111] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 27. | Ng JJ, Kow AWC. Pedicled omental patch as a bridging procedure for iatrogenic bile duct injury. World J Gastroenterol. 2017;23:6741-6746. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Goh BK, Tan YM, Cheow PC, Chung AY, Chow PK, Wong WK, Ooi LL. Solid pseudopapillary neoplasms of the pancreas: an updated experience. J Surg Oncol. 2007;95:640-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 29. | Andreasi V, Partelli S, Crippa S, Balzano G, Tamburrino D, Muffatti F, Belfiori G, Cirocchi R, Falconi M. A systematic review and meta-analysis on the role of omental or falciform ligament wrapping during pancreaticoduodenectomy. HPB (Oxford). 2020;22:1227-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 30. | Panahi P, Ibrahim R, Veeralakshmanan P, Ackah J, Coleman M. Appendiceal phlegmon in adults: Do we know how to manage it yet? Ann Med Surg (Lond). 2020;59:274-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Nasseri YY, Zhu R, Sutanto C, Wai C, Cohen JS, Ellenhorn J, Artinyan A. Role of right hemicolectomy in patients with low-grade appendiceal mucinous adenocarcinoma. Am J Surg. 2019;218:1239-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 32. | Young S, Sueda SK, Hotta M, Sung ML, OʼConnor VV, Leung AM. Surgical management of appendiceal mucinous neoplasm: Is appendectomy sufficient? J Surg Oncol. 2020;122:1173-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 33. | Narasimhan V, Pham T, Warrier S, Craig Lynch A, Michael M, Tie J, Ramsay R, Heriot A. Outcomes from cytoreduction and hyperthermic intraperitoneal chemotherapy for appendiceal epithelial neoplasms. ANZ J Surg. 2019;89:1035-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Bell PD, Huber AR, Drage MG, Barron SL, Findeis-Hosey JJ, Gonzalez RS. Clinicopathologic Features of Low-grade Appendiceal Mucinous Neoplasm: A Single-institution Experience of 117 Cases. Am J Surg Pathol. 2020;44:1549-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Andersson DP, Thorell A, Löfgren P, Wirén M, Toft E, Qvisth V, Riserus U, Berglund L, Näslund E, Bringman S, Thörne A, Arner P, Hoffstedt J. Omentectomy in addition to gastric bypass surgery and influence on insulin sensitivity: a randomized double blind controlled trial. Clin Nutr. 2014;33:991-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 36. | Dillard TH, Purnell JQ, Smith MD, Raum W, Hong D, Laut J, Patterson EJ. Omentectomy added to Roux-en-Y gastric bypass surgery: a randomized, controlled trial. Surg Obes Relat Dis. 2013;9:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 37. | Mazzaferro D, Song P, Massand S, Mirmanesh M, Jaiswal R, Pu LLQ. The Omental Free Flap-A Review of Usage and Physiology. J Reconstr Microsurg. 2018;34:151-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 38. | Dai JG, Zhang ZY, Min JX, Huang XB, Wang JS. Wrapping of the omental pedicle flap around esophagogastric anastomosis after esophagectomy for esophageal cancer. Surgery. 2011;149:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 39. | Graham RR. The treatment of acute perforation of duodenal ulcer. Am J Surg. 1946;72:802-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 40. | Boshnaq M, Thakrar A, Martini I, Doughan S. Utilisation of the falciform ligament pedicle flap as an alternative approach for the repair of a perforated gastric ulcer. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 41. | Agnifili A, Schietroma M, Carloni A, Mattucci S, Caterino G, Carlei F. [Omentoplasty is effective in lowering the complications of ano-rectal resections]. Minerva Chir. 2004;59:363-368. [PubMed] |
| 42. | Qin B, Xu W, Li Y. Are omentectomy and lymphadenectomy necessary in patients with apparently early-stage malignant ovarian germ cell tumors? Int J Gynecol Cancer. 2019;29:398-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 43. | Xu W, Li Y. Is Omentectomy Mandatory Among Early Stage (I, II) Malignant Ovarian Germ Cell Tumor Patients? Int J Gynecol Cancer. 2017;27:1373-1378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 44. | Arie AB, McNally L, Kapp DS, Teng NN. The omentum and omentectomy in epithelial ovarian cancer: a reappraisal: part II--The role of omentectomy in the staging and treatment of apparent early stage epithelial ovarian cancer. Gynecol Oncol. 2013;131:784-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 45. | Ulker V, Tunca A, Numanoglu C, Akbayir O, Akyol A, Erim A, Ongut C. Should omentectomy be a part of surgical staging in patients with endometrioid adenocarcinoma of the uterine corpus? Gynecol Obstet Invest. 2014;77:58-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 46. | Ross MS, Elishaev E, Berger JL, Kelley JL, Taylor SE. Prognostic Significance of omental Disease and the Role of Omental Sampling in Patients With Uterine Carcinosarcoma. Int J Gynecol Cancer. 2018;28:254-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 47. | Luz R, MacDonald N, Mould T. Omental Biopsy for Surgical Staging of Uterine Serous Carcinoma. Int J Gynecol Cancer. 2016;26:1448-1454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 48. | Ozdal B, Unlu BS, Yalcin HR, Tapisiz OL, Energin H, Besli M, Gungor T. Role of omentectomy and appendectomy in surgical staging of endometrioid endometrial cancer. Eur J Gynaecol Oncol. 2013;34:322-324. [PubMed] |
| 49. | Ariake K, Yokoyama S, Doi T, Takemura S, Kajiwara T, Kuroda F. Effect of omentum removal on the risk for postoperative adhesive small bowel obstruction recurrence: a case-control study. Int J Surg. 2015;13:27-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 50. | Urade T, Sawa H, Murata K, Mii Y, Iwatani Y, Futai R, Abe S, Sanuki T, Morinaga Y, Kuroda D. Omental abscess due to a spilled gallstone after laparoscopic cholecystectomy. Clin J Gastroenterol. 2018;11:433-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 51. | Yamada M, Sato H, Ieko Y, Miyasaka Y, Kanai T, Yano N, Ono T, Akamatsu H, Harada M, Ichikawa M, Teranishi Y, Kikuchi Y, Nemoto K. In silico comparison of the dosimetric impacts of a greater omentum spacer for abdominal and pelvic tumors in carbon-ion, proton and photon radiotherapy. Radiat Oncol. 2019;14:207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 52. | Houben CH, Chan KW, Mou JW, Tam YH, Lee KH. Irreducible inguinal hernia in children: how serious is it? J Pediatr Surg. 2015;50:1174-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 53. | Kataoka J, Nitta T, Ota M, Takashima Y, Yokota Y, Fujii K, Higashino T, Ishibashi T. Laparoscopic omentectomy in primary torsion of the greater omentum: report of a case. Surg Case Rep. 2019;5:76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 54. | Sugi Subramaniam RV, Karthikeyan VS, Sistla SC, Ali SM, Sistla S, Vijayaraghavan N, Ram D. Intra-abdominal melioidosis masquerading as a tubercular abdomen: report of a rare case and literature review. Surg Infect (Larchmt). 2013;14:319-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 55. | Akhan SE, Dogan Y, Akhan S, Iyibozkurt AC, Topuz S, Yalcin O. Pelvic actinomycosis mimicking ovarian malignancy: three cases. Eur J Gynaecol Oncol. 2008;29:294-297. [PubMed] |
| 56. | Tamboli RA, Hajri T, Jiang A, Marks-Shulman PA, Williams DB, Clements RH, Melvin W, Bowen BP, Shyr Y, Abumrad NN, Flynn CR. Reduction in inflammatory gene expression in skeletal muscle from Roux-en-Y gastric bypass patients randomized to omentectomy. PLoS One. 2011;6:e28577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 57. | Milleo FQ, Campos AC, Santoro S, Lacombe A, Santo MA, Vicari MR, Nogaroto V, Artoni RF. Metabolic effects of an entero-omentectomy in mildly obese type 2 diabetes mellitus patients after three years. Clinics (Sao Paulo). 2011;66:1227-1233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 58. | Radtke J, Schild R, Reismann M, Ridwelski RR, Kempf C, Nashan B, Rothe K, Koch M. Obstruction of peritoneal dialysis catheter is associated with catheter type and independent of omentectomy: A comparative data analysis from a transplant surgical and a pediatric surgical department. J Pediatr Surg. 2018;53:640-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 59. | Di Taranto G, Chen SH, Elia R, Bolletta A, Amorosi V, Sitpahul N, Chan JC, Ribuffo D, Chen HC. Free gastroepiploic lymph nodes and omentum flap for treatment of lower limb ulcers in severe lymphedema: Killing two birds with one stone. J Surg Oncol. 2020;121:168-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 60. | Uchibori A, Okada S, Takeda-Miyata N, Tsunezuka H, Kato D, Inoue M. Omental Flap for Bronchopleural Fistula After Pneumonectomy and Aorta Replacement. Ann Thorac Surg. 2020;109:e349-e351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |