Published online Feb 27, 2020. doi: 10.4240/wjgs.v12.i2.77
Peer-review started: October 1, 2019
First decision: October 23, 2019
Revised: November 18, 2019
Accepted: December 5, 2019
Article in press: December 5, 2019
Published online: February 27, 2020
Processing time: 106 Days and 20.2 Hours
Upper gastrointestinal fishbone microperforations are rare and not commonly reported in medical literature. Despite the increasing use of computer tomography (CT) imaging and the employment of the Alvardo criteria, misdiagnosis of acute appendicitis can still occur. We report the rare case of an elderly Chinese gentleman who had a fish-bone induced microperforation of the duodenum that closely mimicked the symptoms of acute appendicitis.
This 79-year-old man presented with migratory lower abdominal pain that localized at his periumbilical region and right lower quadrant. He had associated pyrexia, general malaise and was noted to have an elevated white cell count. CT investigations initially revealed a distended appendix which was resected laparoscopically but showed no obvious signs of gross inflammation. The patient then deteriorated clinically and had increased oxygen requirements immediately after the surgery. This prompted further investigations. A further review of his CT scan revealed a fine fishbone microperforation in the distal duodenum associated with retroperitoneal abscess formation and seepage extending into the right lower quadrant. He was then started on broad spectrum intravenous antibiotics and subsequently underwent a laparotomy 12 h later to manage the obscure aetiology and to drain the abscess. The post-operative course was uneventful and he was discharged 11 d later including a 2-d stay in the intensive care unit.
This case offers an insight into a potential mimic of acute appendicitis and the diagnostic difficulties experienced in such presentations.
Core tip: This case provides clinicians with a unique insight on how a patient with a fishbone induced upper gastrointestinal microperforation can mimic the lower gastrointestinal symptoms commonly seen in acute appendicitis. It highlights the difficulty that the team faced with the diagnosis and management of such pathology and provides clinicians with an alternative differential diagnosis that can be considered in this specific patient group. Additionally, it serves to remind clinicians about the importance of accurate radiological imaging and the potential of observer error (particularly that of the satisfaction-of-search error) that can occur when managing patients with seemingly straightforward presentations.
- Citation: Lim D, Ho CM. Appendicitis-mimicking presentation in fishbone induced microperforation of the distal duodenum: A case report. World J Gastrointest Surg 2020; 12(2): 77-84
- URL: https://www.wjgnet.com/1948-9366/full/v12/i2/77.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v12.i2.77
Microperforations are defined as small perforations that result in the presence of localized air bubbles outside the bowel wall without the presence of any pneumoperitoneum and are usually associated with diverticular disease[1]. We report this rare but unique case of an elderly 79-year-old Chinese gentleman who presented with the clinical symptoms of appendicitis but was eventually diagnosed with a fishbone induced microperforation of the distal duodenum.
Fishbones are one of the most common forms of ingested foreign bodies. While most ingested fishbones are asymptomatic, some can lodge themselves within the gastrointestinal (GI) tract and cause a microperforation[2]. Depending on its location, they can cause local inflammation and haematoma formation[3,4]. This case is particularly relevant due to the possible epidemiological link between the Chinese population and the increased prevalence of ingested fishbones, as suggested by Arulanandam et al[5] who attributed this to an increase in consumption of unfilleted fish and the common practice of deboning fish using their mouths.
Acute appendicitis is common and classically presents with migrating lower abdominal and right iliac fossa pain with the accompanying symptoms of pyrexia and general malaise. The current diagnostic approach incorporates a combination of clinical suspicion, haematological findings, the exclusion of other differentials, ultrasound and radiological investigations to diagnose acute appendicitis[6]. Increasing use of computer tomography (CT) imaging and employment of the Alvardo criteria in clinical practice has further increased the diagnostic accuracy of clinicians, achieving a positive diagnosis rate of 80%-95%[7]. However, misdiagnosis, such as fishbone-induced injury can still occur, as seen by the following case.
This case report is primarily written to highlight a unique case of a patient who presented with a fishbone-induced microperforation of the upper GI tract that accurately mimicked the symptoms of acute appendicitis, the diagnostic difficulty that the team experienced and the management pathway that was undertaken in the treatment of this patient. No proposed scientific question was formulated through the abovementioned case.
This 79-year-old Chinese male presented with a one-day history of lower abdominal pain and pyrexia.
The pain initially presented at the peri-umbilical region and later migrated to his right lower quadrant. He reported no associated dysuria, nausea, vomiting, hematemesis or melena and has a known past medical history of hypertension, type 2 diabetes mellitus and hyperlipidaemia. He was recently admitted for bronchoscopy and biopsy of a left bronchial mass a week prior to this episode. This was later found to be a bronchial carcinoid tumour.
On examination, he had generalized lower abdominal tenderness with maximal tenderness around the periumbilical and right lower quadrant. His abdomen was otherwise soft with mild guarding, active bowel sounds and no rigidity. His vitals were slightly deranged, with a tachycardia (heart rate 110 beats/min), tachypnea (respiratory rate 22 times/min), mild hypertension (132/78 mmHg) and pyrexia (38.4 °C) Otherwise, his oxygen saturations remained normal (96%) on room air and he had no acute confusion or neurological deficit.
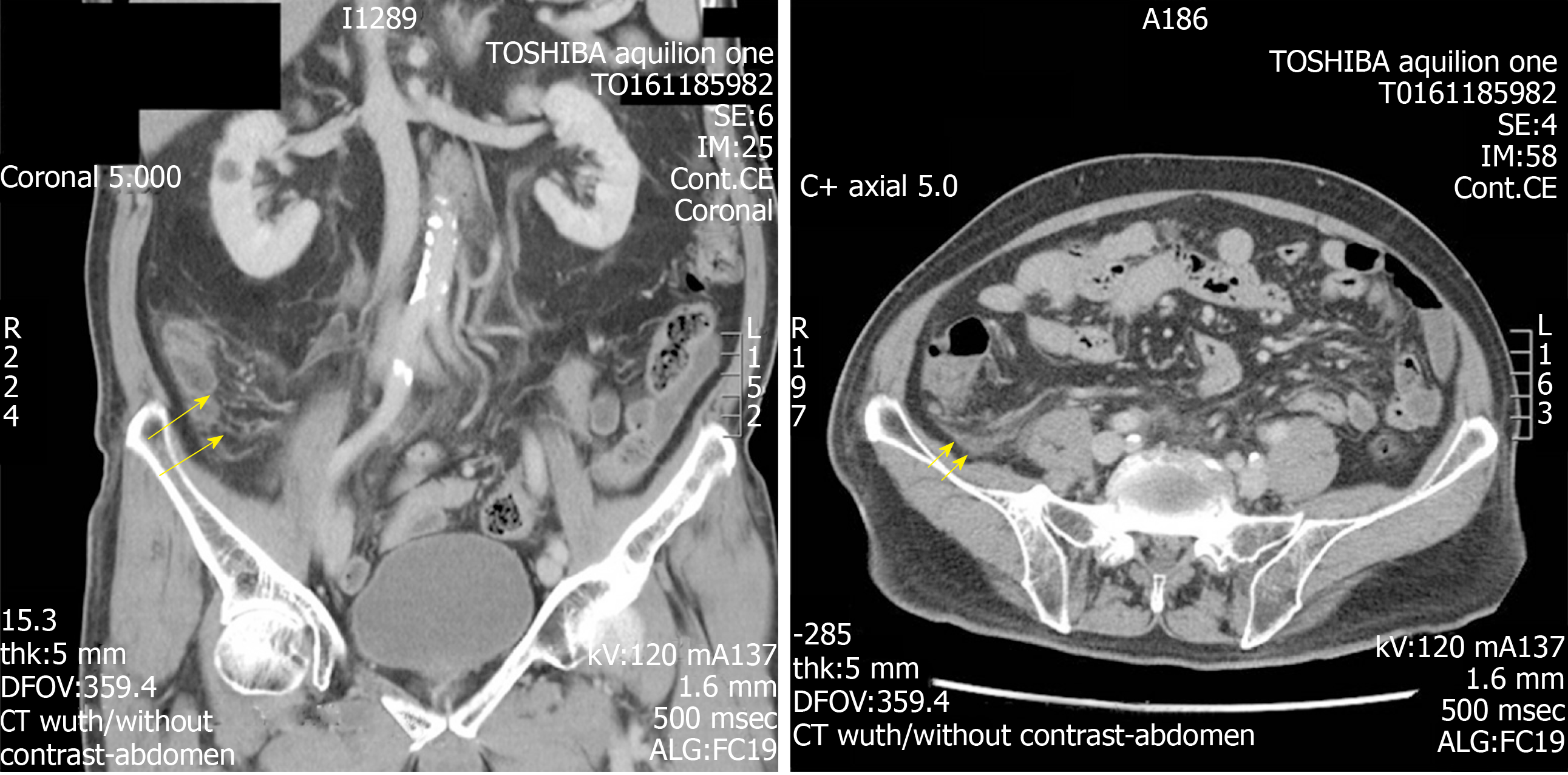
He had a raised white cell count of 16.98 × 103/mm3 with raised neutrophils. C-reactive protein (0.98 mg/L) and other parameters were within the normal range. CT of the abdomen and pelvis with contrast excluded any renal calculi and revealed the presence of a dilated tubular structure with mild fat stranding with increased enhancement (Figure 1). This structure and the associated inflammatory changes were presumed to be an inflamed appendix. As the symptoms and radiological evidence fit, a preliminary diagnosis of acute appendicitis was made.
The patient underwent a laparoscopic appendectomy the following day. An intact and mildly erythematous appendix was resected and some clear ascitic fluid was drained from within the peritoneum.
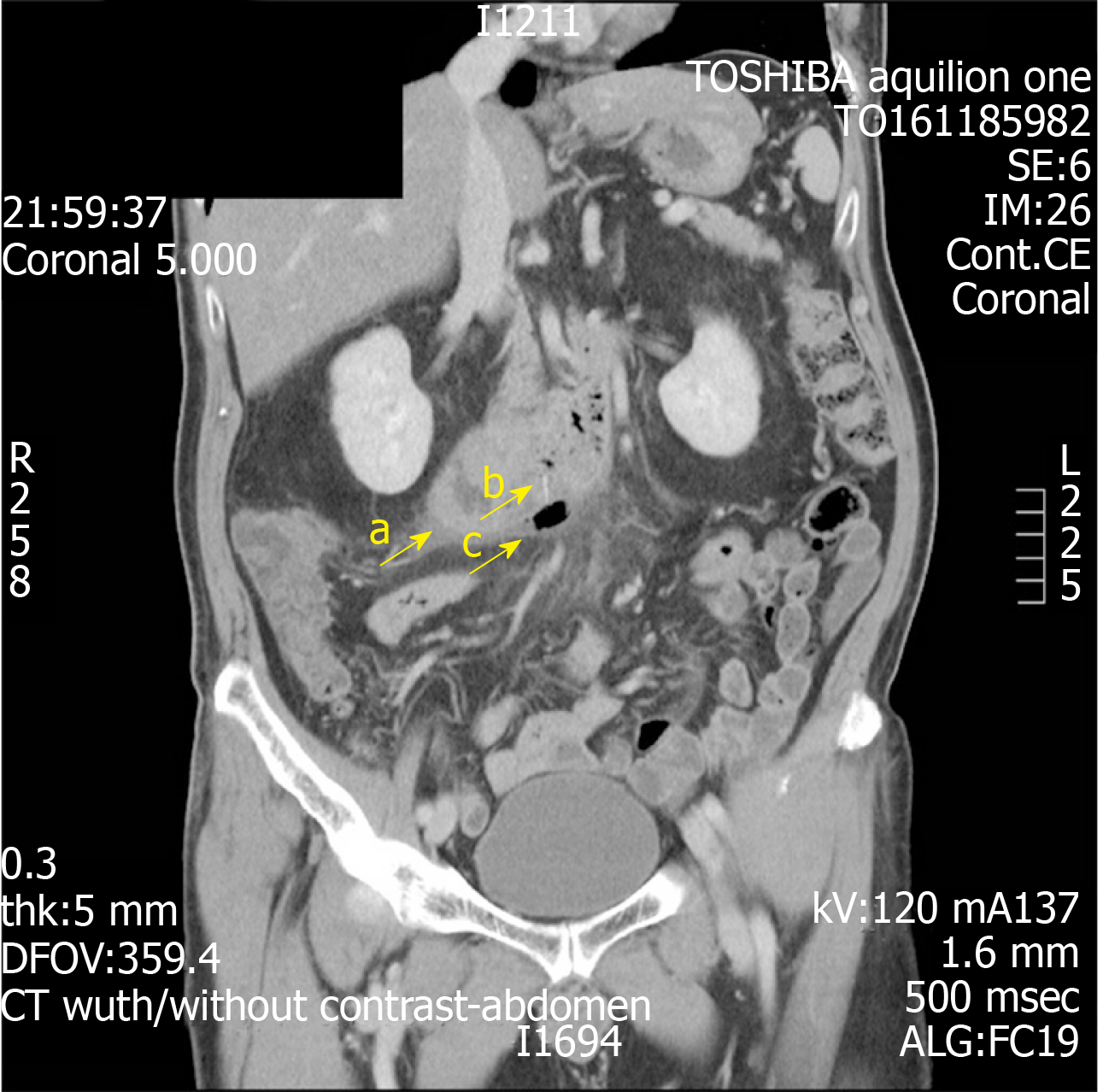
During the immediate postoperative phase, the patient suffered an acute deterioration and had increasing oxygen requirements. There were also concomitant acute changes of consolidation seen on his chest radiograph. These prompted concerns of possible unresolved sepsis. A further review of his CT scans revealed an additional finding of a fine fishbone of 1.4 cm in length. This had caused a microperforation at the inferior border of the 3rd segment of the duodenum, resulting in the formation of an abscess and associated fat stranding along the right pararenal fascia (Figures 2 and 3).
Further review of his CT scan suggested that the preliminary diagnosis was inaccurate, and that the patient most likely had a fishbone induced microperforation of his duodenum that resulted in the formation of a small retroperitoneal abscess.
Based on his deteriorating clinical condition at that time, a decision to undergo an exploratory laparotomy was made. In the interim, the patient was started on broad-spectrum intravenous antibiotics (Meropenam). The laparotomy was performed 12 h after the appendectomy. The localized retroperitoneal abscess was drained and 10 mL of pus was aspirated. However, despite thorough examination of the duodenum, both the exact site of perforation and the fishbone were unable to be identified and retrieved. Manual pressure was then applied at the presumed site of the microperforation based on the CT scan to reintroduce the bone back into the intestinal lumen. The area was subsequently washed out and a retroperitoneal drain was inserted.
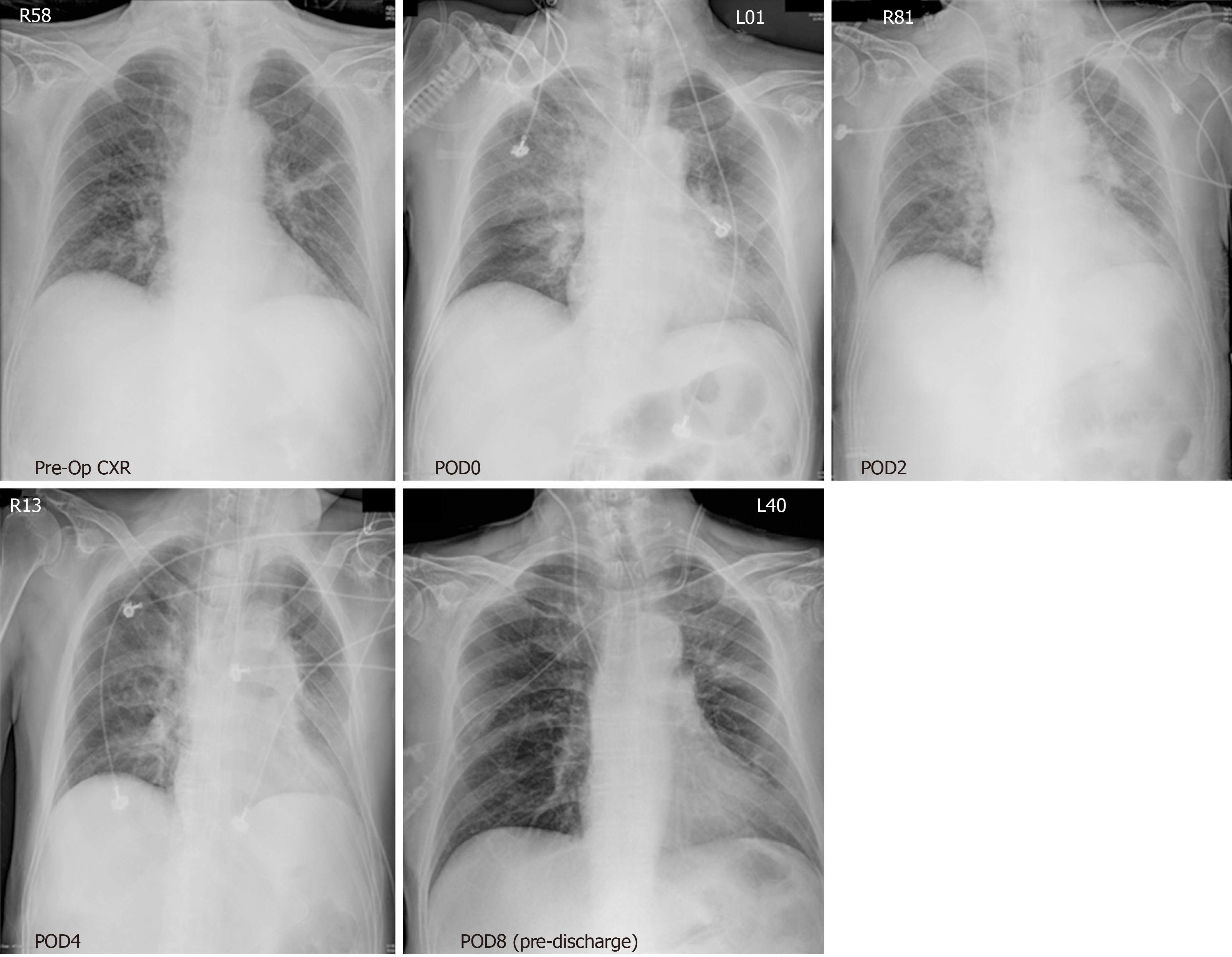
Post-operatively, the patient was transferred to the intensive care unit for 2 d. A feeding jejunostomy was inserted for enteral feeding and to prevent the recurrence of a retro-peritonitis. He did not require any inotropic support and required decreasing amounts of ventilatory support to manage his oxygen requirements. His oxygen saturations improved, and the changes noted in his chest radiograph rapidly resolved (Figure 4). His pain was well controlled with analgesia and he was stepped down to the wards where he recovered well. His antibiotics was then converted to an oral form (levofloxacin) and his retroperitoneal drain was removed. Regular oral feeding was re-introduced and the patient remained well with further complications. He was subsequently discharged after a total of 11 d in hospital. On follow-up, the patient remained well and did not develop any long-term complications related to his ingested fishbone. He then had his jejunostomy tube removed and required no further follow-up from the team.
Subsequent pathological examination of the resected appendix showed minimal infiltration of neutrophils. This effectively excluded acute appendicitis as the main diagnosis for this episode. His cultures from the abscess isolated intestinal coliforms and confirmed that the infection was from a GI source. Detailed cross-examination of the entire case revealed that his initial oxygen desaturation were secondary to pulmonary haemorrhage that occurred from traumatic suctioning during anaesthesia and was the cause of his acute changes on his chest radiographs. This was incidental and was not related to his intrabdominal sepsis.
Fishbone microperforation of the distal GI tract is rare but is increasingly reported across various centres in the last 10 years[8-10]. However, due to its ambiguous presentation, the diagnosis can often be missed, leading to increased complications[11]. This scenario may be further complicated by the possible subacute presentation of fish-bone induced microperforation and the individual patient’s lack of awareness of fishbone ingestion[9]. Specifically, this patient’s ingestion of the fish bone was attributed to his consumption of fish soup a week ago as a traditional remedy following his recent biopsy for his bronchial carcinoid tumour and he had not noticed the ingestion of any fishbone.
Typically, fish bones lodge themselves within the aerodigestive tract, and occasionally at the distal GI tract, near the terminal ileum and caecum[12-14]. Only a few cases of duodenal, jejunal and proximal ileal microperforations were reported and these usually resulted in damage to local structures like the pancreas and the development of peritonitis[9,15].
What defines this case was the way this patient presented. He presented with the classical symptoms of pyrexia, raised inflammatory markers and migratory epigastric to right lower quadrant abdominal pains that is commonly associated with acute appendicitis. Furthermore, the positive radiological findings of a distended appendiceal structure seemed to agree with the clinical presentation and further supported the initial diagnosis of acute appendicitis. In addition, due to the lack of patient awareness of fishbone ingestion and the small number of similar cases reported, the fish bone was not noticed during the initial interpretation of the scan. Therefore, the final diagnosis of a duodenal microperforation with a retroperitoneal abscess raised unexpected great attention.
While the exact pathophysiology remains unclear, we believed that the initial microperforation caused the presentation of periumbilical pain. Due to the retroperitoneal nature of the distal duodenum, it is postulated that intestinal content must have seeped within the retroperitoneal space into the right pararenal fascia, forming the retroperitoneal abscess. This resulted in the development of localized “retro-peritonitis” which corresponded to his right lower quadrant pain. This disease process is the likely reason behind the migratory nature of his pain. Furthermore, we believe that the retroperitoneal nature of the site of microperforation and subsequent abscess formation accounted for the inability to visualize any intra-peritoneal pathology during the initial laparoscopy.
The management of such microperforation can take either a medical or surgical approach. Medical treatment is usually done via the endoscopic retrieval of the fish bone, alongside intravenous antibiotic administration and can be considered in patients who present without major complications[10,16]. This was not suitable in this patient due to his deteriorating clinical condition at the time and concerns regarding progressing sepsis. As a result, a surgical approach was considered. This usually includes a midline laparotomy with identification and closure of the area of perforation via primary repair, the removal of the fishbone and the aspiration of any abscess or fluids within the abdominal or retroperitoneal space, with post-operative antibiotics and monitoring[10].
In this case, the inability to identify and remove the fishbone during the laparotomy did not appear to have an impact on the recovery of the patient and he improved clinically. It is therefore hypothesized that the fishbone dislodged itself form the initial area of microperforation and had passed through the entirety of the patient’s GI tract without any further incident[2]. This is further supported by the uneventful post-operative course and the lack of any further complications pertaining to the retained fishbone. As a result, further investigation and management such as endoscopy w not necessary unless any complications or indications arose.
The importance of accurate imaging and interpretation was also highlighted by this case. Radiographs, although often performed early, are not helpful due to the possibility of radiolucency of fish bones. As a result, CT investigations are increasingly used, and this helps reduce the gap between these common abdominal symptoms and the diagnostic uncertainty. We believe that this case highlights a form of observer error, specifically that of the satisfaction-of-search error, given the similarity of the patient’s symptoms to acute appendicitis and the ambiguous appearance of the appendix in the scan[17]. In such errors, As reported by Bathla et al[3], the use of CT scans as diagnostic investigations are reliably sensitive in finding the lodged fish bone, with missed diagnoses often attributed to a lack of observer awareness. This was seen in this case and was similarly highlighted in other studies[3,18]. Fish bones were usually identified as either linear or curvilinear calcifications within the GI tract with associated inflammatory changes like fat stranding and/or a pneumoperitoneum[19]. Such changes of fat stranding were noted along the area of inflammation in this patient’s CT scan. Thus, the effective use and meticulous interpretation of CT imaging, along with detailed history tracing and correlation, can play a large role in narrowing the diagnostic dilemma when dealing with these conditions.
This case report showcases the large diagnostic difficulty faced by clinicians when managing patients with upper GI microperforations, particularly those with symptoms that can mimic common conditions such as acute appendicitis. It displays the diagnostic and management process behind a patient with a fishbone-induced upper GI perforation can present with the classical symptoms of acute appendicitis and provides an additional differential diagnosis that can be considered. In addition, this case provides clinicians with a good example of the satisfaction-of-search error that can occur when interpreting straightforward presentations and emphasizes the importance of accurate radiological reporting and its roles in patient management and minimising patient morbidity. Concurrently, this case report also highlights the effectiveness of using CT imaging to identify fishbone embedment in patients with such symptoms and previous history of fishbone ingestion.
Thanks to all our colleagues in the General Surgery and Radiology departments at National Taiwan University Hospital for their support and collaboration in the challenging diagnosis and management of this patient.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Taiwan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Azevedo R, Sikiric P, Tchilikidi KY S-Editor: Yan JP L-Editor: A E-Editor: Ma YJ
| 1. | Pemberton JH. Acute colonic diverticulitis: Medical management. [cited 11 November 2019]. Available from: https://www.uptodate.com/contents/acute-colonic-diverticulitis-medical-management. |
| 2. | Ambe P, Weber SA, Schauer M, Knoefel WT. Swallowed foreign bodies in adults. Dtsch Arztebl Int. 2012;109:869-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 129] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 3. | Bathla G, Teo LL, Dhanda S. Pictorial essay: Complications of a swallowed fish bone. Indian J Radiol Imaging. 2011;21:63-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Venkatesh SH, Venkatanarasimha Karaddi NK. CT findings of accidental fish bone ingestion and its complications. Diagn Interv Radiol. 2016;22:156-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Arulanandam S, Das De S, Kanagalingam J. A prospective study of epidemiological risk factors for ingestion of fish bones in Singapore. Singapore Med J. 2015;56:329-32; quiz 333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Baird DLH, Simillis C, Kontovounisios C, Rasheed S, Tekkis PP. Acute appendicitis. BMJ. 2017;357:j1703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 7. | Petroianu A. Diagnosis of acute appendicitis. Int J Surg. 2012;10:115-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 77] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 8. | Magadum SB, Mench K, Anaje A, Mulla V. Appendicular perforation caused by fish bone: A rare case report. Med J DY Patil Univ. 2014;7:764-765. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Symeonidis D, Koukoulis G, Baloyiannis I, Rizos A, Mamaloudis I, Tepetes K. Ingested fish bone: an unusual mechanism of duodenal perforation and pancreatic trauma. Case Rep Gastrointest Med. 2012;2012:308510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Arango LA, León Sierra LP, Martínez Gutiérrez DC, Jurado Grisales M. Incidental foreign body in the gastrointestinal tract: Report of three cases and literature review. Rev Col Gastroenterol. 2011;26:316-327. |
| 11. | Triadafilopoulos G. Ingested foreign bodies and food impactions in adults. 2011. [cited 4 April 2019]. Available from: https://www.uptodate.com/contents/ingested-foreign-bodies-and-food-impactions-in-adults. |
| 12. | Kim HU. Oroesophageal Fish Bone Foreign Body. Clin Endosc. 2016;49:318-326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg. 1990;211:459-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 167] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | Chiu HH, Li JH, Chen JS. Penetration of esophageal wall by a fish bone. J Intern Med Taiwan. 2006;17:298-301. |
| 15. | Choi Y, Kim G, Shim C, Kim D, Kim D. Peritonitis with small bowel perforation caused by a fish bone in a healthy patient. World J Gastroenterol. 2014;20:1626-1629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Dedania B, Khanapara D, Panwala A, Dharan M. A Case of Mysterious Impacted Duodenal Foreign Body Presenting with Halitosis. Case Rep Gastroenterol. 2016;10:800-807. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Pinto A, Brunese L. Spectrum of diagnostic errors in radiology. World J Radiol. 2010;2:377-383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 144] [Cited by in RCA: 122] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 18. | Akazawa Y, Watanabe S, Nobukiyo S, Iwatake H, Seki Y, Umehara T, Tsutsumi K, Koizuka I. The management of possible fishbone ingestion. Auris Nasus Larynx. 2004;31:413-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Beecher SM, O'Leary DP, McLaughlin R. Diagnostic dilemmas due to fish bone ingestion: Case report & literature review. Int J Surg Case Rep. 2015;13:112-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |