Published online May 27, 2019. doi: 10.4240/wjgs.v11.i5.271
Peer-review started: April 4, 2019
First decision: May 8, 2019
Revised: May 18, 2019
Accepted: May 23, 2019
Article in press: May 23, 2019
Published online: May 27, 2019
Processing time: 53 Days and 10.1 Hours
Anastomotic leak (AL) after low anterior resection (LAR) can be a highly morbid complication. The incidence of AL ranges from 5% to 20% depending on patient characteristics and the distance of the anastomosis from the anal verge. Low anastomoses and leaks pose technical challenges for endoscopic treatment. The aim of this report was to describe the use of a commercially available laparoscopic energy device through a transanal minimally invasive surgery (TAMIS) port for the management of a symptomatic leak not requiring relaparotomy (grade B) after a LAR with diverting loop ileostomy.
A TAMIS GelPOINT Path port was inserted into the anus to access the distal rectum. Pneumorectum was achieved with AirSeal insufflation and a 30 degree laparoscope was introduced through a trocar. A LigaSureTM Retractable L-Hook device was then used to perform a septotomy of the chronic sinus tract identified posterior to the coloproctostomy. The procedure was then repeated twice in three weeks intervals with ultimate resolution of the chronic leak cavity. Several months after serial TAMIS septotomies, barium enema demonstrated a patent anastomosis with no evidence of persistent leak or stricture. The patient subsequently underwent ileostomy reversal and has had no significant post-operative issues.
TAMIS septotomy with the LigaSureTM Retractable L-Hook is a feasible and effective, minimally invasive salvage technique for the treatment of grade B ALs. Larger studies are needed to assess the generalizability and long-term results of this technique.
Core tip: Anastomotic leaks (ALs) after low anterior resection for the treatment of rectal cancer are highly morbid complications and often pose a technical challenge for its treatment. We report a case of a transanal minimally invasive septotomy of a chronic sinus secondary to an AL, with the use of the Ligasure retractable L-Hook device. This safe and effective technique may help avoid re-operations which are associated with higher mortality and higher permanent stoma rates.
- Citation: Olavarria OA, Kress RL, Shah SK, Agarwal AK. Novel technique for anastomotic salvage using transanal minimally invasive surgery: A case report. World J Gastrointest Surg 2019; 11(5): 271-278
- URL: https://www.wjgnet.com/1948-9366/full/v11/i5/271.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v11.i5.271
Colorectal cancer remains the third most common cause of cancer related deaths in the United States among men and women. The American Cancer Society estimates there to be over 43000 new patients diagnosed with rectal cancer yearly[1]. Mortality associated with this pathology is proportionally related to the staging of the disease prior to surgical treatment.
Over the past decades, significant advancements have been made in the manage-ment of rectal cancer in efforts to improve locoregional control. Among these, universal adoption of neoadjuvant therapy has been as important as the improvements in surgical techniques to control local spread of cancer and recurrence rates. After the introduction of restorative anterior resection by Dixon in 1948, boosted by the advent of surgical staplers and total mesorectal excision (TME) during proctectomy, there was an increase in the proportion of low anterior resection (LAR) over abdominoperineal resection (APR) for the treatment of rectal cancer[2-6]. However, the improved oncologic and functional outcomes resulted in higher leak rates associated with colorectal and coloanal anastomoses[7,8].
LAR for colorectal cancer has a reported morbidity of 20% with anastomotic leak (AL) being among the most dreaded complications. Multivariate analysis and logistic regression models evaluating risk factors for AL after LAR demonstrate that the lower the anterior resection, the more likely an AL will occur[9,10]. Reported rates of AL range between 5% to 20%[11-14]. This variation is in part attributed to the lack of a universally accepted nomenclature and classification of ALs. In 2010, the International Study Group of Rectal Cancer proposed a definition and severity grading system for AL after anterior resection of the rectum[15]. The proposed grading system constituted three groups based on the severity of the AL: Grade A represents an AL identified on imaging not requiring therapeutic interventions. Grade B is a leak requiring interventions such as administration of antibiotics, transanal lavage and/or radiologic assisted placement of a pelvic drain, but not re-laparotomy. And lastly, grade C is a leak requiring re-laparotomy.
Within the options for management of grade B ALs, endoscopic interventions are often used to diagnose and treat the underlying pathology. The ability to treat the AL with minimally invasive techniques is paramount as re-operation is associated with higher mortality rates and higher rates of a permanent stoma[14,16,17].
The purpose of this study was to describe the utility of a commercially available laparoscopic energy device, LigaSureTM Retractable L-Hook (Medtronic, Minneapolis, MN), through transanal minimally invasive surgery (TAMIS) as a novel technique for the management of a grade B AL after LAR.
A 69-year-old hispanic male initially presented with abdominal pain, weight loss, and hematochezia.
Patient was seen in gastroenterology clinic after 6-month having experienced lower abdominal pain, malaise, unintentional weight loss and loose bowel movement with occasional blood in the stool. Patient denied any similar symptoms prior to that time.
Past medical history was positive for benign essential hypertension.
Personal and family history were negative for colorectal cancer, inflammatory bowel disease or other gastrointestinal diseases.
On physical examination, abdomen was soft, non-tender, with no palpable masses. Digital rectal examination revealed a palpable circumferential mass at approximately 7 cm from anal verge.
Routine blood tests including complete blood count, comprehensive metabolic panel and urinalysis were all within normal limits, except hypochromic microcytic anemia with a hemoglobin of 7.4 g/dL and carcinoembryonic antigen was elevated to 4.1 ng/dL (normal range 0.0-3.0 ng/dL)
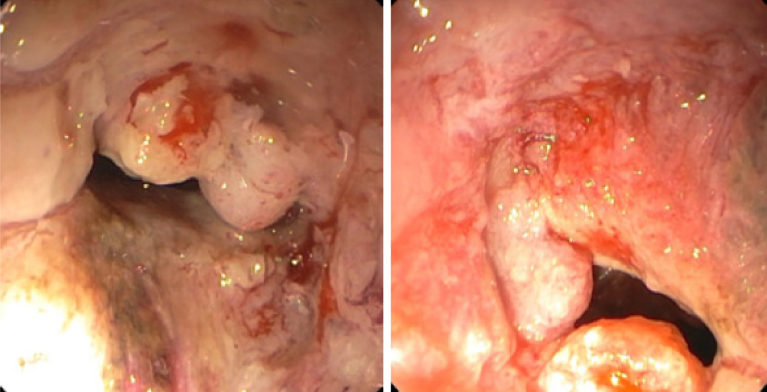
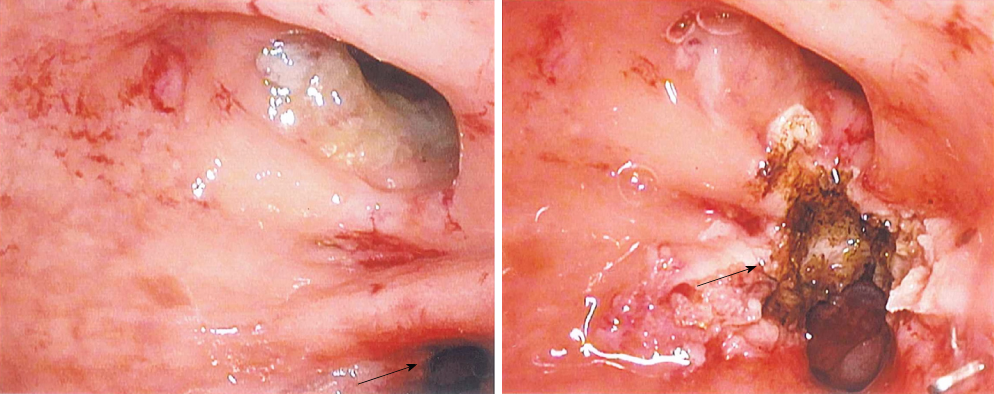
Patient underwent a diagnostic colonoscopy which revealed a near-obstructing, circumferential, ulcerated rectal mass at 7 cm from anal verge (Figure 1). Magnetic resonance imaging of the pelvis was consistent with extramural invasion of the tumor into the muscularis propria with mesorectal nodal involvement.
Biopsy performed during colonoscopy revealed an invasive, moderately diffe-rentiated adenocarcinoma of the rectum (T3N1).
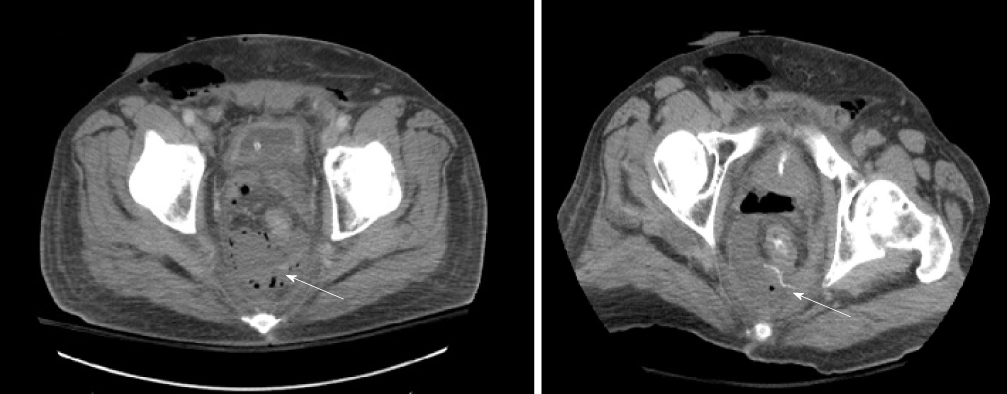
The patient underwent neoadjuvant chemotherapy with 5-Fluorouracil in combi-nation with radiation therapy. Ten weeks after completion of neoadjuvant therapy, he was taken to the operating room for a robotic assisted laparoscopic LAR with TME, stapled coloproctostomy and diverting loop ileostomy. Post-operative course was complicated by a grade B AL with presacral abscess (Figure 2) requiring intravenous antibiotic therapy and percutaneous drainage by interventional radiology. The drain was kept in place for 2 wk and was ultimately removed when output was minimal. The patient recovered uneventfully and plans were made for subsequent ileostomy takedown.
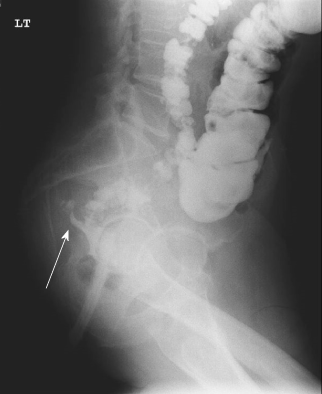
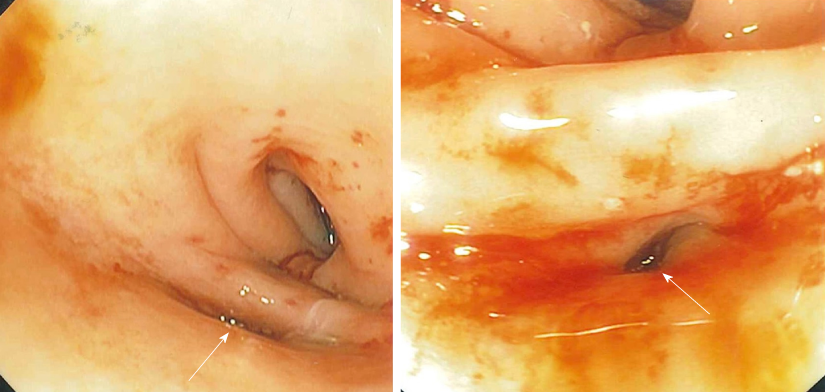
Pre-operative workup for ileostomy takedown including a barium contrast enema (Figure 3) revealed a posterior sinus tract which was confirmed on flexible sigmoidoscopy (Figure 4). In order to prevent future sinus tract drainage and abscess formation, the decision was made to surgically intervene prior to ileostomy reversal. Endoscopic management was not considered given that the staple line and sinus tract location (posterolateral) were 4 cm from the anal verge. Visualization was suboptimal without pneumorectum. Therefore, the decision was made to proceed with a TAMIS approach.
Patient was brought to the operating room, placed under general anesthesia and transitioned into high lithotomy position. A GelPOINT Path® TAMIS port (Applied Medical, Rancho Santa Margarita, CA, United States) was inserted into the anus and secured to the skin with 2-0 silk sutures. Three trocars were placed through the TAMIS port. Pneumorectum was achieved with AirSeal® (Conmed, Utica, NY) insufflation and a 30 degree laparoscope was introduced through the trocar. The chronic sinus tract was identified just posterior to the coloproctostomy at 4 cm from the anal verge. The LigaSureTM Retractable L-Hook device was used to perform partial septotomies to create a wide opening of the mucosal bridge present between the sinus tract and the lumen (Figure 5). The cavity was then bluntly cleared of granulation and fibrotic tissue. The procedure was sequentially repeated twice, under general anesthesia, in three weeks intervals until the sinus tract was completely opened.
After three total septotomy treatments over the course of 9 wk, the sinus tract completely resolved. Post intervention barium contrast enema revealed resolution of the sinus tract and leak (Figure 6). The patient ultimately underwent ileostomy takedown without complications and was doing well at the 6 mo post-operative visit, having 2-3 bowel movements per day with no continence issues.
With the advent of emerging techniques for the treatment of rectal cancer in past decades, significant advances have been made in improving oncologic and functional outcomes[6]. LAR has been coined as the standard of care in selected cases which were previously treated with APR, often preventing the need for a permanent stoma. Unfortunately, this led to the emergence of new challenges inherent to the LAR technique including ALs which can be difficult complications to manage.
Minimally invasive septotomies have been endorsed for the treatment of chronic sinus tracts not only after colorectal interventions but also after foregut procedures including sleeve gastrectomies and roux-en-y gastric bypass for weight loss complicated with staple line leaks[18-21]. During this intervention the septum separating an abscess cavity and the true lumen is divided resulting in a larger communication of both lumens (true lumen and abscess lumen). By these means, internal drainage is favored through a path of low resistance with redirection of the leak flow from the abscess cavity towards the true lumen, resulting in contraction and scarring of the chronic leak/abscess cavity.
Minimally invasive management of AL after low and ultralow anterior resections has the benefit of minimizing the risk of temporary and permanent stomas[13]. Specifically, endoscopic therapies such as fibrin glue application, endoscopic stenting, endoluminal vacuum drainage and clipping have all been described as options to manage varying grades of ALs[22,23]. However, these techniques tend to be less effective for chronic leaks and are limited by several factors including the distance from the anal verge, size of the defect, or ability to traverse the anastomosis.
In cases where endoscopic means are incapable of managing the leak, TAMIS via rectal insufflation can be effective[24,25]. This provides an alternate route to access to the distal rectum with use of conventional laparoscopic instruments[26].
In this report, we describe a minimally invasive technique using a commercially available transanal port and energy device to induce insufflation within the rectum and complete sequential septotomies of a chronic draining sinus tract of the rectum after a LAR. When compared to other energy sources such as bovie and harmonic scalpel, the LigaSure L-Hook offers advantages such as less thermal spread, additional reach and better control due to the retractable technology, and ability to get into tight spaces. Although the concept of endoscopic enlargement and eventual obliteration of a sinus tract after a colorectal leak has been reported in the literature, to our knowledge, this is the first report of the use of the LigaSureTM Retractable L-Hook device during this technique[24,27,28].
No consensus exists for the management of ALs and the determination must be individualized for each patient. Minimally invasive techniques are safe and effective at managing symptomatic, small, contained leaks. However, few studies have compared effectiveness among different modalities and even fewer studies have looked at long term results after these are performed.
The treatment of grade B ALs after LAR for rectal cancer can be challenging. TAMIS septotomy with the LigaSureTM Retractable L-Hook device is a feasible and effective technique for the treatment of select grade B ALs. Larger studies with longer follow up are needed to assess the generalizability and long-term results of this technique.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Balta AZ S-Editor: Ji FF L-Editor: A E-Editor: Wang J
| 1. | American Cancer Society. Key Statistics for Colorectal Cancer, 2018. Available from: URL: https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html. |
| 2. | Stewart DB, Dietz DW. Total mesorectal excision: what are we doing? Clin Colon Rectal Surg. 2007;20:190-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Heald RJ. A new approach to rectal cancer. Br J Hosp Med. 1979;22:277-281. [PubMed] |
| 4. | Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery--the clue to pelvic recurrence? Br J Surg. 1982;69:613-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1985] [Cited by in RCA: 1937] [Article Influence: 45.0] [Reference Citation Analysis (1)] |
| 5. | Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986;1:1479-1482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1867] [Cited by in RCA: 1914] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 6. | Lirici MM, Hüscher CG. Techniques and technology evolution of rectal cancer surgery: a history of more than a hundred years. Minim Invasive Ther Allied Technol. 2016;25:226-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (2)] |
| 7. | Kapiteijn E, Putter H, van de Velde CJ; Cooperative investigators of the Dutch ColoRectal Cancer Group. Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg. 2002;89:1142-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 362] [Cited by in RCA: 377] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 8. | Carlsen E, Schlichting E, Guldvog I, Johnson E, Heald RJ. Effect of the introduction of total mesorectal excision for the treatment of rectal cancer. Br J Surg. 1998;85:526-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 219] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 9. | Yeh CY, Changchien CR, Wang JY, Chen JS, Chen HH, Chiang JM, Tang R. Pelvic drainage and other risk factors for leakage after elective anterior resection in rectal cancer patients: a prospective study of 978 patients. Ann Surg. 2005;241:9-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 234] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 10. | Eriksen MT, Wibe A, Norstein J, Haffner J, Wiig JN; Norwegian Rectal Cancer Group. Anastomotic leakage following routine mesorectal excision for rectal cancer in a national cohort of patients. Colorectal Dis. 2005;7:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 254] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 11. | Eckmann C, Kujath P, Schiedeck TH, Shekarriz H, Bruch HP. Anastomotic leakage following low anterior resection: results of a standardized diagnostic and therapeutic approach. Int J Colorectal Dis. 2004;19:128-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 114] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 12. | Nesbakken A, Nygaard K, Lunde OC, Blücher J, Gjertsen Ø, Dullerud R. Anastomotic leak following mesorectal excision for rectal cancer: true incidence and diagnostic challenges. Colorectal Dis. 2005;7:576-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Chopra SS, Mrak K, Hünerbein M. The effect of endoscopic treatment on healing of anastomotic leaks after anterior resection of rectal cancer. Surgery. 2009;145:182-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Maggiori L, Bretagnol F, Lefèvre JH, Ferron M, Vicaut E, Panis Y. Conservative management is associated with a decreased risk of definitive stoma after anastomotic leakage complicating sphincter-saving resection for rectal cancer. Colorectal Dis. 2011;13:632-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Büchler MW. Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery. 2010;147:339-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 732] [Cited by in RCA: 1033] [Article Influence: 68.9] [Reference Citation Analysis (4)] |
| 16. | Sabbagh C, Maggiori L, Panis Y. Management of failed low colorectal and coloanal anastomosis. J Visc Surg. 2013;150:181-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Smith JD, Butte JM, Weiser MR, D'Angelica MI, Paty PB, Temple LK, Guillem JG, Jarnagin WR, Nash GM. Anastomotic leak following low anterior resection in stage IV rectal cancer is associated with poor survival. Ann Surg Oncol. 2013;20:2641-2646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Mahadev S, Kumbhari V, Campos JM, Galvao Neto M, Khashab MA, Chavez YH, Bessler M, Gonda TA. Endoscopic septotomy: an effective approach for internal drainage of sleeve gastrectomy-associated collections. Endoscopy. 2017;49:504-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 19. | Guerron AD, Ortega CB, Portenier D. Endoscopic Abscess Septotomy for Management of Sleeve Gastrectomy Leak. Obes Surg. 2017;27:2672-2674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Haito-Chavez Y, Kumbhari V, Ngamruengphong S, De Moura DT, El Zein M, Vieira M, Aguila G, Khashab MA. Septotomy: an adjunct endoscopic treatment for post-sleeve gastrectomy fistulas. Gastrointest Endosc. 2016;83:456-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Angrisani L, Hasani A, Santonicola A, Vitiello A, Iovino P, Galasso G. Endoscopic Septotomy for the Treatment of Sleeve Gastrectomy Fistula: Timing and Indications. Obes Surg. 2018;28:846-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Blumetti J, Abcarian H. Management of low colorectal anastomotic leak: Preserving the anastomosis. World J Gastrointest Surg. 2015;7:378-383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 70] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (4)] |
| 23. | Verlaan T, Bartels SA, van Berge Henegouwen MI, Tanis PJ, Fockens P, Bemelman WA. Early, minimally invasive closure of anastomotic leaks: a new concept. Colorectal Dis. 2011;13 Suppl 7:18-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Whitlow CB, Opelka FG, Gathright JB, Beck DE. Treatment of colorectal and ileoanal anastomotic sinuses. Dis Colon Rectum. 1997;40:760-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 56] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | van Vledder MG, Doornebosch PG, de Graaf EJ. Transanal endoscopic surgery for complications of prior rectal surgery. Surg Endosc. 2016;30:5356-5363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Dapri G, Guta D, Grozdev K, Antolino L, Bachir N, Jottard K, Cadière GB. Colorectal anastomotic leakage corrected by transanal laparoscopy. Colorectal Dis. 2016;18:O210-O213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Sneider E, Maykel J. Management of anastomotic leak after low anterior resection with transanal endoscopic microsurgical (TEM) debridement and repair. J Surg Case Rep. 2012;2012:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Brunner W, Rossetti A, Vines LC, Kalak N, Bischofberger SA. Anastomotic leakage after laparoscopic single-port sigmoid resection: combined transanal and transabdominal minimal invasive management. Surg Endosc. 2015;29:3803-3805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |