Published online Nov 30, 2009. doi: 10.4240/wjgs.v1.i1.68
Revised: June 1, 2008
Accepted: June 8, 2008
Published online: November 30, 2009
We report a case of eosinophilic enteritis involving the proximal small bowel, a relatively rare entity, presenting unusually as enteroliths in a 68-year-old man with complaints of anemia, malena and abdominal pain. The disease if diagnosed in the initial stages responds well to medical treatment but if associated with complications or misdiagnosed, surgical modality is the treatment of choice. In our case, the patient presented with enteroliths and strictures. Resection and anastomosis of the small bowel containing stones was carried out. Histopathology confirmed the diagnosis as eosinophilic enteritis.
- Citation: Shivathirthan N, Maheshwari G, Kamath D, Haldar P. Enterolithiasis complicating eosinophilic enteritis: A case report and review of literature. World J Gastrointest Surg 2009; 1(1): 68-70
- URL: https://www.wjgnet.com/1948-9366/full/v1/i1/68.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v1.i1.68
Eosinophilic enteritis, a relatively rare entity, usually involves gastric antrum or proximal small bowel[1]. Eosinophilic gastroenteritis is defined as a disorder that selectively affects the gastrointestinal tract with eosinophil-rich inflammation in the absence of any known causes for eosinophilia[2]. The disease may be asymptomatic or may present as chronic anemia, recurrent abdominal pain, subacute and acute intestinal obstruction or as a rare presentation as enterolithiasis which has not been described previously.
In our case, the patient presented with enteroliths and strictures. Resection and anastomosis of the small bowel containing stones was performed. Histopathology confirmed the diagnosis as eosinophilic enteritis. .
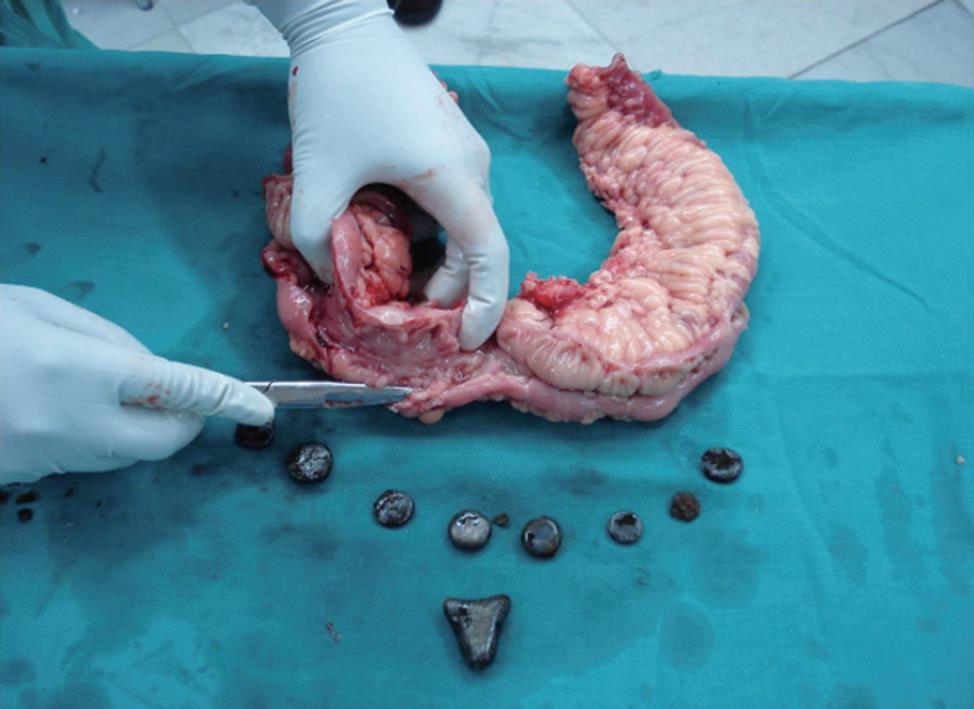
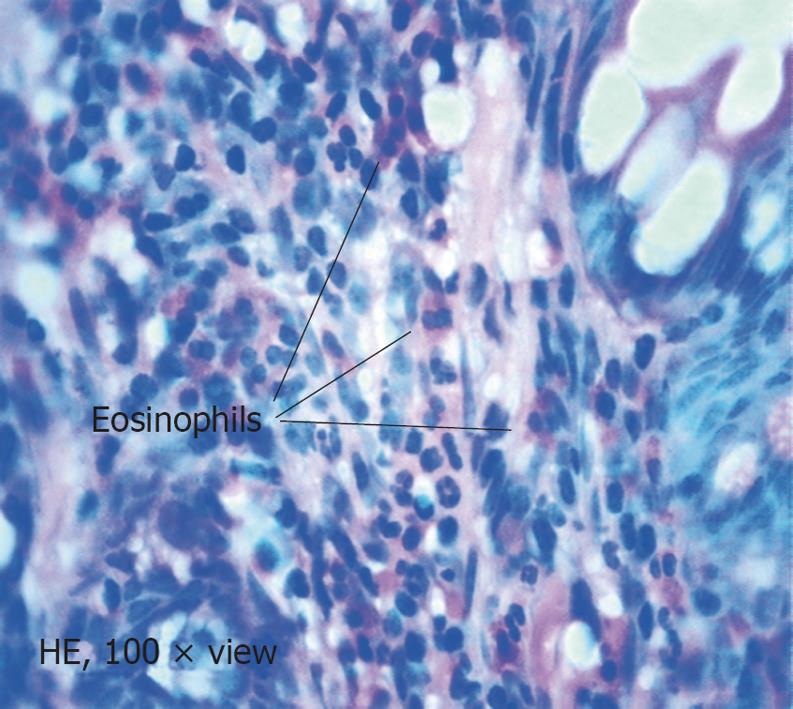
A 68-year-old man was referred to us with complaints of chronic anemia, malena and abdominal pain for 15 years. The patient had been evaluated earlier and had been transfused on multiple occasions. His past medical profile was not suggestive of any associated medical condition and there was no history of use of herbal medications or excessive intake of tea or coffee. Baseline blood investigations, chest X-ray and ECG were normal. Stool for occult blood was positive. Upper gastrointestinal endoscopy and colonoscopy were normal. Ultrasound of the abdomen did not reveal any evidence of cholecystitis or cholelithiasis. The patient underwent a small bowel enteroclysis which revealed multiple strictures in the distal jejunum and proximal ileum with filling defects suggestive of enteroliths. The patient was subjected to exploratory laparotomy through a midline incision. There were multiple strictures at the junction of distal jejunum and proximal ileum with sacculations in between containing more than 10 enteroliths measuring between 4-20 mm (Figure 1). Resection and anastomosis of the small bowel containing stones was then carried out. The resected specimen was sent for histopathological examination. Abdomen was drained and closed in layers. The pathological report of the small bowel containing the enteroliths showed dense transmural infiltration of eosinophils, and eosinophilic enteritis was diagnosed (Figure 2). The biochemical analysis of the stones retrieved from the bowel showed the presence of calcium and oxalate crystals along with concretions of ingested vegetable fibre. Calcium oxalate was reported to be the major component of these stones. The patient had uneventful recovery and was discharged on the 10th postoperative day.
Primary eosinophilic gastrointestinal disorders are defined as disorders that selectively affect the gastrointestinal tract with eosinophil-rich inflammation in the absence of known causes for eosinophilia (e.g. drug reactions, parasitic infections, and malignancy)[2]. These disorders include eosinophilic esophagitis, eosinophilic gastritis, eosinophilic gastroenteritis, eosinophilic enteritis, and eosinophilic colitis and are occurring with increasing frequency[3]. The symptoms depend on the site of infiltration and the layers affected. High blood levels of eosinophils are usually present. Computed tomography plays a fundamental role in the evaluation of this disease[4].
In contrast to the esophagus, the stomach and intestine have readily detectable baseline eosinophils under healthy conditions. Eosinophilic gastritis, enteritis and gastroenteritis are grouped together because they are clinically similar and there is a paucity of information available concerning their pathogenesis. However, it is likely that they are indeed distinct entities in most patients. These diseases are characterized by the selective infiltration of eosinophils in the stomach, small intestine, or both, with variable involvement of the esophagus, large intestine, or both[5,6]. It is now appreciated that many disorders are accompanied by eosinophil infiltration in the stomach, such as parasitic and bacterial infections (including Helicobacter pylori), IBD, hypereosinophilic syndrome (HES), eosinophilic enteritis, periarteritis, allergic vasculitis, scleroderma, drug injury, and drug hypersensitivity[7]. These disorders are classified into primary and secondary subtypes. The primary subtype includes the atopic, nonatopic, and familial variants, whereas the secondary subtype is divided into two groups, one is composed of systemic eosinophilic disorders (HES) and the other is composed of non eosinophilic disorders. Primary eosinophilic enteritis, gastritis and gastroenteritis have also been called idiopathic or allergic gastroenteropathy. The familial form has not been well characterized. Primary eosinophilic gastroenteritis encompasses multiple disease entities subcategorized into three types on the basis of the histologic involvement: mucosal, muscularis and serosal forms[8]. Of note, either layer of the gastrointestinal tract can be involved, so that endoscopic biopsy can be normal in patients with the muscularis subtype, serosal subtype, or both. No standards are available for the diagnosis of eosinophilic gastritis or gastroenteritis, but a few findings support the diagnosis[9]. For example, the presence of increased eosinophils in biopsy specimens from the gastrointestinal tract wall, the infiltration of eosinophils within intestinal crypts and gastric glands, the lack of involvement of other organs, and the exclusion of other causes of eosinophilia (e.g. infections and IBD) are supportive of eosinophilic gastroenteritis. The clinical presentations of eosinophilic enteritis depend on the site of involvement with eosinophilic enterits being asymptomatic or symptomatic. Symptomatic cases may present as chronic anemia, subacute intestinal obstruction due to strictures, acute obstruction due to intussusceptions or chronic abdominal pain[1,2,6].
Enteroliths, the endogenous foreign bodies, were first described by Pfahler and Stamm in 1915. True enteroliths of the small intestine are of three main types: (1) those consisting mainly of bile acids; (2) those consisting mainly of calcium oxalate; and (3) those consisting mainly of phosphate. Bile acid enteroliths are made up mainly of choleic acid.
The maximum size reported in the literature is more than 6 cm, and maximum number is up to 1400 enteroliths proximal to a postoperative stricture in a patient who had surgery for colon carcinoma[10]. Most of the conditions causing enteroliths are due to stasis or hypermotility[10]. Enteroliths in association with eosinophilic enteritis has not been reported so far in the literature to the best of our knowledge. Judging from published reports, cases of stones in the small intestine are rare. In the literature, the composition is described only in general terms. It would no doubt increase our understanding of the subject, and probably of lithiasis in general, if all such stones were reported and analysed as completely as possible.
Peer reviewer: Nikolaus Gassler, Professor, Institute of Pathology, University Hospital RWTH Aachen, Pauwelsstrasse 30, 52074 Aachen, Germany
S- Editor Zhong XY L- Editor Ma JY E- Editor Lin YP
| 1. | Kshirsagar AY, Jagtap SV, Kanojiya RP, Langade YB, Shinde SL, Shekhar N. Eosinophilic enteritis presenting as a rare cause for ileo-ileal intussusception. World J Gastroenterol. 2007;13:6444-6445. |
| 2. | Shin WG, Park CH, Lee YS, Kim KO, Yoo KS, Kim JH, Park CK. Eosinophilic enteritis presenting as intussusception in adult. Korean. J Intern Med. 2007;22:13-17. |
| 3. | Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004;113:11-28; quiz 29. |
| 4. | Ahualli J, Méndez-Uriburu L, Ravera ML, Raimondo MA, Ortiz Mayor M. [Primary eosinophilic enteritis: a case report]. Radiologia. 2007;49:272-274. |
| 5. | Torpier G, Colombel JF, Mathieu-Chandelier C, Capron M, Dessaint JP, Cortot A, Paris JC, Capron A. Eosinophilic gastroenteritis: ultrastructural evidence for a selective release of eosinophil major basic protein. Clin Exp Immunol. 1988;74:404-408. |
| 6. | Katz AJ, Twarog FJ, Zeiger RS, Falchuk ZM. Milk-sensitive and eosinophilic gastroenteropathy: similar clinical features with contrasting mechanisms and clinical course. J Allergy Clin Immunol. 1984;74:72-78. |
| 7. | Ahmad M, Soetikno RM, Ahmed A. The differential diagnosis of eosinophilic esophagitis. J Clin Gastroenterol. 2000;30:242-244. |
| 8. | Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH. Eosinophilic gastroenteritis. Medicine (Baltimore). 1970;49:299-319. |
| 9. | Kelly KJ. Eosinophilic gastroenteritis. J Pediatr Gastroenterol Nutr. 2000;30 Suppl:S28-S35. |
| 10. | Klingler PJ, Seelig MH, Floch NR, Branton SA, Metzger PP. Small-intestinal enteroliths--unusual cause of small-intestinal obstruction: report of three cases. Dis Colon Rectum. 1999;42:676-679. |