Copyright
©The Author(s) 2015.
World J Diabetes. Dec 10, 2015; 6(17): 1323-1336
Published online Dec 10, 2015. doi: 10.4239/wjd.v6.i17.1323
Published online Dec 10, 2015. doi: 10.4239/wjd.v6.i17.1323
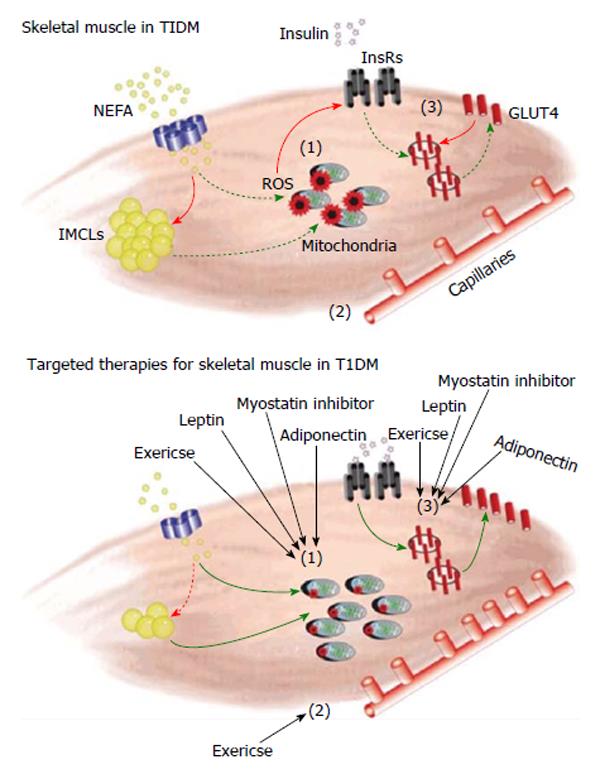
Figure 1 Schematic figure representing skeletal muscle dysfunction in type 1 diabetes mellitus and possible therapeutic approaches targeting skeletal muscle.
(1) In T1DM, due to dyslipidemia and/or the reduced ability for muscle to uptake carbohydrates, an increased amount of non-esterified fatty acids (NEFA) are shuttled into the skeletal muscle. The majority of this excess fat is deposited in the form of intramyocellular lipid droplets (IMCLs) as there is a reduced ability to efficiently oxidize lipids due to impairments to oxidative capacity. An increased amount of metabolic stress and reactive oxygen species (ROS) production within the mitochondria is observed in T1DM and appears to be a causative factor; (2) T1DM also induces dysfunction with regard to the vasculature network. There is a thickening of the basement membrane and downregulation of angiogenesis resulting in a decreased capillary-to-fiber ratio. Impairments to microvasculature have also been linked with generation of macrovascular complications (e.g., atherosclerosis), a serious long-term diabetic complication; and (3) Insulin resistance results in disruptions to the insulin signalling pathway. Improper insulin signalling prevents excess glucose in the blood from being taken up by the muscle via decreased translocation of the GLUT4 glucose transporter. Our proposed treatments of exercise, myostatin inhibition, leptin and adiponectin target the specific pathways mentioned above in skeletal muscle. We hypothesize that if diabetic myopathy is attenuated it will allow muscle to contribute a greater amount towards reducing hyperglycemia. Since muscle is an important large metabolic organ, if skeletal muscle health was improved there would be resultant decreases in oxidative stress, improvements to glycemic control and a reduction in the need for exogenous insulin. T1DM: Type 1 diabetes mellitus; GLUT4: Glucose transporter type 4.
- Citation: Coleman SK, Rebalka IA, D’Souza DM, Hawke TJ. Skeletal muscle as a therapeutic target for delaying type 1 diabetic complications. World J Diabetes 2015; 6(17): 1323-1336
- URL: https://www.wjgnet.com/1948-9358/full/v6/i17/1323.htm
- DOI: https://dx.doi.org/10.4239/wjd.v6.i17.1323