Copyright
©The Author(s) 2020.
World J Diabetes. Jul 15, 2020; 11(7): 293-308
Published online Jul 15, 2020. doi: 10.4239/wjd.v11.i7.293
Published online Jul 15, 2020. doi: 10.4239/wjd.v11.i7.293
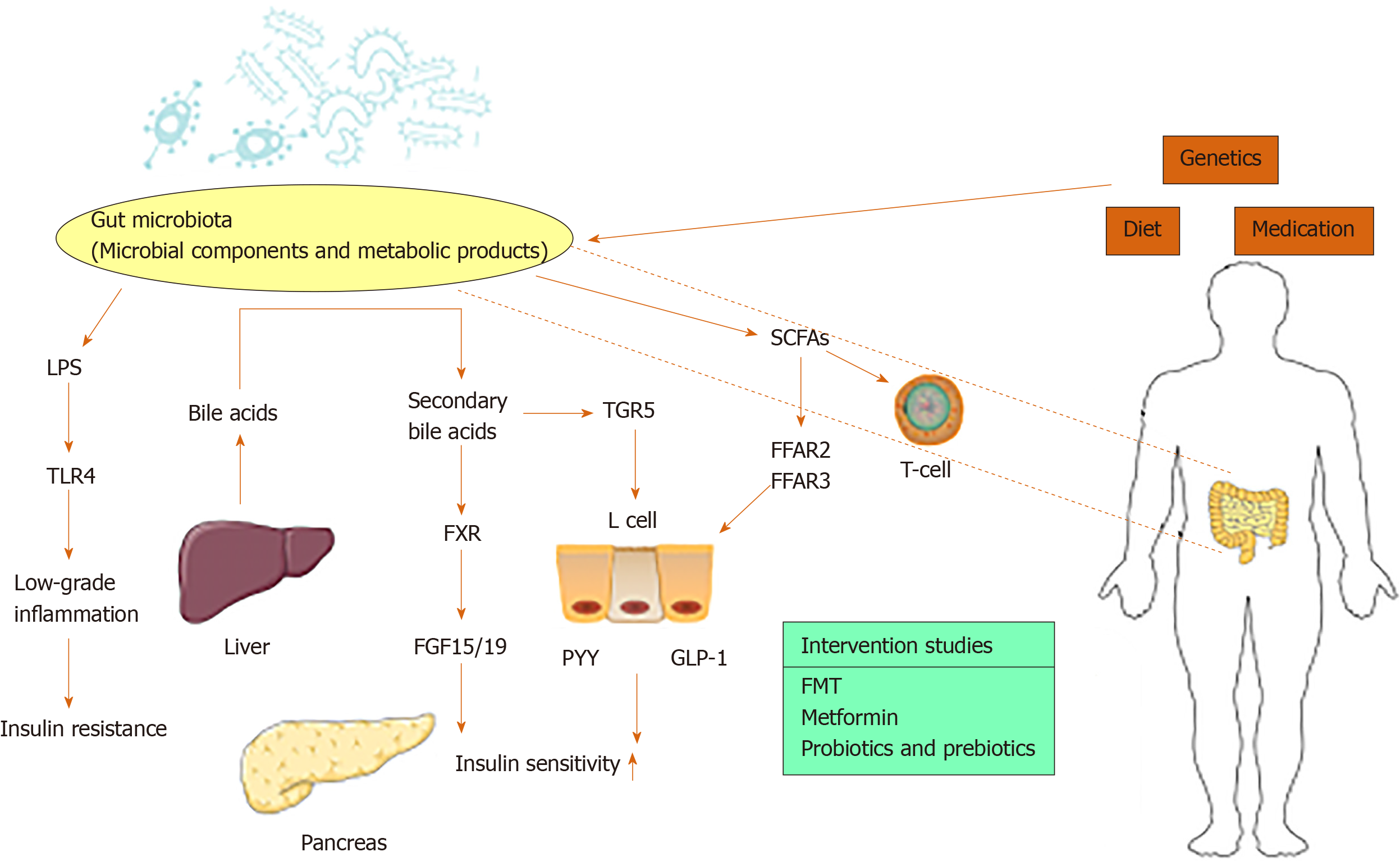
Figure 1 The main mechanism of gut microbiota affecting insulin resistance and diabetes.
Gut microbes are influenced by diet, genetics and medication, and common types of interventions in humans include fecal microbiota transplantation, metformin and probiotics. Lipopolysaccharide (LPS), short-chain fatty acids (SCFAs) and bile acids are major regulators of diabetes. LPS binds to the Toll-like receptor 4 to induce low-grade inflammation and insulin resistance. Bile acids are synthesized by the liver and transformed into secondary bile acids through the metabolism of gut microbiota. Secondary bile acids activate Farnesoid X receptor to induce increased secretion of fibroblast growth factor 15/19. Secondary bile acids activate Takeda G protein-coupled receptor to stimulate intestinal L cells to secrete glucagon-like peptide-1 (GLP-1). SCFAs activate L cells to promote the release of GLP-1 and peptide YY to increase insulin sensitivity. SCFAs also have a regulatory effect on T cells. LPS: Lipopolysaccharide; TLR4: Toll-like receptor 4; FXR: Farnesoid X receptor; FGF15/19: Fibroblast growth factor 15/19; TGR5: Takeda G protein-coupled receptor 5; PYY: Peptide YY; GLP-1: Glucagon-like peptide-1; SCFAs: Short-chain fatty acids; FFAR 2: Free fatty acid receptor 2; FFAR 3: Free fatty acid receptor 3; FMT: Fecal microbiota transplantation.
- Citation: Li WZ, Stirling K, Yang JJ, Zhang L. Gut microbiota and diabetes: From correlation to causality and mechanism. World J Diabetes 2020; 11(7): 293-308
- URL: https://www.wjgnet.com/1948-9358/full/v11/i7/293.htm
- DOI: https://dx.doi.org/10.4239/wjd.v11.i7.293