Published online Sep 15, 2014. doi: 10.4251/wjgo.v6.i9.377
Revised: May 11, 2014
Accepted: July 18, 2014
Published online: September 15, 2014
Processing time: 207 Days and 9.2 Hours
Synchronous occurrence of adenocarcinoma and mucosa associated lymphoid tissue (MALT) lymphoma of colon is rare, and its presence with coexisting tuberculosis is still rarer. To our knowledge, this may be the first case report. In the present report, we describe a 43-year-old female who presented with a history of abdominal pain, fever, loss of weight and loss of appetite. Colonoscopy showed a large ulceroproliferative mass arising from the caecum, biopsy of which showed it to be adenocarcinoma of the colon. A right hemicolectomy was performed and microscopic study of the colon revealed tuberculosis and synchronous adenocarcinoma with lymphoma. Eight of sixteen lymph nodes showed tuberculosis and three of sixteenpericoloniclymphnodes showed metastatic deposits. Immunostains further confirmed the tumour to be adenocarcinoma with MALT lymphoma. We would like to highlight the diagnostic challenges arising from the multi-faceted presentations of these three conditions.
Core tip: We report a first case report of synchronous adenocarcinoma,mucosa associated lymphoid tissue (MALT) lymphoma and tuberculosis in the same segment of colon in 43-year-old immunocompetent female patient. There are around 4 case reports of sychronous adenocarcinoma and MALT lymphoma to date in the literature.What we describe isthe first such case in the literature.
- Citation: Velu ARK, Srinivasamurthy BC, Nagarajan K, Sinduja I. Colonic adenocarcinoma, mucosa associated lymphoid tissue lymphoma and tuberculosis in a segment of colon: A case report. World J Gastrointest Oncol 2014; 6(9): 377-380
- URL: https://www.wjgnet.com/1948-5204/full/v6/i9/377.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v6.i9.377
Mucosa-associated lymphoid tissue (MALT) tumors are a distinct subtype of non-Hodgkin’s lymphoma associated with predisposing infectious or autoimmune processes, resulting in chronic lymphoid proliferation. Though the stomach is the most common site, MALT tumor has been reported in non-gastric sites like salivary gland, lung, ocular adnexa and skin[1]. The colon is a rare location for MALT lymphoma[2]. Synchronous colonic adenocarcinoma and malignant lymphoma in the same patient is rare with an estimated incidence of around 0.0002%[3]. Only a few cases have been reported in literature.Adenocarcinoma and tuberculosis occurring at the same site is exceedingly rare. Chronic inflammatory mucosal damage initiating a sequence of metaplasia and dysplasia could result in neoplastic changes[4]. We describe a case report never reported in literature before, sychronous adenocarcinoma and lymphoma with tuberculosis of the colon which poses a diagnostic and therapeutic challengeespecially when the patient can present with equivocal symptoms.
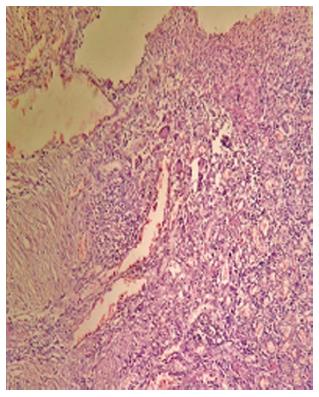
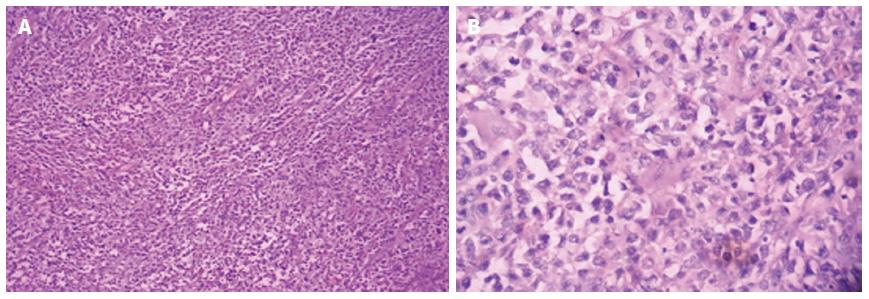
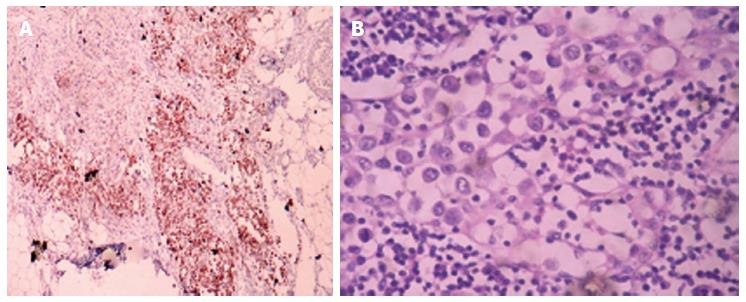
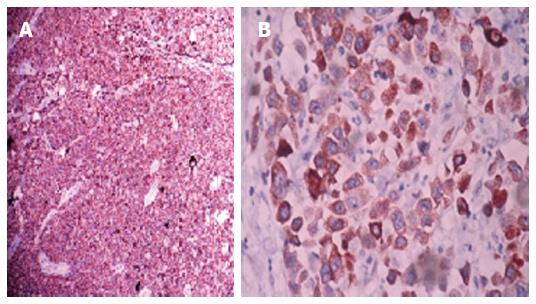
A 43-year-old female was referred with a history of abdominal pain, fever, loss of weight and loss of appetite for 6 mo. Hematological investigations showed normocytic normochromic anemia with a raised erythrocyte sedimentation rate. Chest roentgenogram was normal. Human immunodeficiency virus antibodies were negative. Colonoscopy revealed an ulcero-proliferative mass arising from the caecum. Ultrasonography revealed a thickened caecal wall with mesenteric lymphadenopathy. A biopsy diagnosed it as adenocarcinoma. A right hemicolectomy was performed. The gross pathological examination of the lesion showed a 4 cm × 3.5 cm × 3 cm ulcero-proliferative tumour present on the mucosal surface. The entire mucosal surface appeared normal without any abnormality or polypoidal lesion. Sixteen pericolic lymph nodes varying in size from 0.5 to 3 cm were isolated from pericolic fat. Sections from ulcero-proliferative growthrevealed extensive mucosal necrosis with ill defined granuloma, langhans giant cells (Figure 1) and moderately differentiatedadenocarcinomathat extended through the muscularis propria into the subserosal adipose tissue (Figure 2A). Dense lymphocyticinfiltration was seen in the submucosa. These lymphoid cells were small to medium sized cells with mildly irregular nuclear contours anda moderate pale cytoplasm (Figure 2B). Thus, microscopic study revealed tuberculosis with tumour and the tumour type to be synchronous adenocarcinoma with lymphoma. The adenocarcinoma component was moderately differentiated while the lymphoma component was of low grade MALT lymphoma.The surgical cut margins were free of tumor. Eight of sixteen lymph nodes showed features of tuberculosis with acid fast bacilli in two of the lymph nodes and three of sixteen pericoloniclymphnodes showed metastatic deposits (Figure 3B). A tissue section from mucosa did not reveal acid fast bacilli.Immunohistochemical analysis was performed on representative sections from the colon and lymph node to characterize the lymphoid cells and to confirm adenocarcinoma.CD 20 (Dako preparation) was diffusely positive (Figure 4A) and CD5 was negative in neoplastic lymphocytes. Cytokeratin and epithelial membrane antigen (Figure 3A and Figure 4B) was positive in sections from colon, pericolonictumor and metastatic deposits in lymphnodes.
After surgery, the patient was put on anti-tubercular treatment. No other adjuvant therapy was started as the patient was not willing; the patient is alive and well after 6 mo post-operatively.
Our case, to the best of our knowledge, is the first ever reported case of synchronous adenocarcinoma and lymphoma with tuberculosis. An association of TB and malignancy has been noted by several authors in different organs[4]. Some authors have proposed that the association of carcinoma and tuberculosis is coincidental[5]. In our case both occurred at the same segment of colon and it is justified to think that the inflammatory condition has facilitated malignancy and the impaired immune mechanism has further facilitated the development of second malignancy. In 1987, Tanaka et al[6] analysed 26 TB and adenocarcinoma cases reported in Japan and supported the possibility of cancer originating from a tuberculous lesion. Chronic inflammatory mucosal damage initiating a sequence of metaplasia and dysplasia may result in neoplastic change. On the other hand an impaired host immune response due to malignancy would have reactivated the dormant tubercular lesion. However, it is still a matter of debate and further research is required to determine if a tuberculous infection, being similar to other chronic infections and inflammatory conditions, may facilitate carcinogenesis or the malignancy which reactivates the infection[7]. Devi et al[8] and Argyropoulos et al[9] first reported a case of synchronous adenocarcinoma and MALT lymphoma in athesame segment of colon followed by a series of three cases by Argyropoulos in 2012. Occurrence of secondary MALT-type lymphoma in a patient with prior colon adenocarcinoma after colectomy has been reported in the literature[10]. It is extremely difficult to diagnose synchronous tumours in the same segment.In our case, a dense lymphocytic infiltratenoted in the vicinity of adenocarcinomaalerted us to thoroughly sample the specimen and to assess the immunophenotype by immunohistochemistry which was of great help in confirming the diagnosis.
A 43-year-old female referred with history of abdominal pain, fever, loss of weight and loss of appetite for 6 mo.
Colonoscopy revealed ulcero-proliferative mass arising from the caecum.
Tuberculosis, adenocarcinoma of the colon.
Normocytic normochromic anaemia, raised erythrocyte sedimentation rate, human immunodeficiency virus antibodies negative.
Ultrasonography revealed thickened caecal wall and Mesenteric lymphadenopathy.
Synchronous adenocarcinoma, mucosa associated lymphoid tissue lymphoma and tuberculosis of a segment of colon.
Right hemicolectomy.
On immunohistochemical stain, CD20, cytokeratin and exponential moving average were positive.
Impaired host immune response due to malignancy can reactivate the dormant tubercular lesion. It is extremely difficult to diagnose synchronous tumours in the same segment. In this case, a dense lymphocytic infiltrate noted in the vicinity of adenocarcinomaalerted the authors to thoroughly sample the specimen and to assess the immunophenotype by immunohistochemistry which was of great help in confirming the diagnosis.
This paper is the first report of synchronous adenocarcinoma and lymphoma with tuberculosis. This is an interesting case report.
P- Reviewer: Aurello P, De Silva AP, Garcia-Elorriaga G, Kowada A S- Editor: Song XX L- Editor: O’Neill M E- Editor: Wu HL
| 1. | Zucca E, Conconi A, Pedrinis E, Cortelazzo S, Motta T, Gospodarowicz MK, Patterson BJ, Ferreri AJ, Ponzoni M, Devizzi L. Nongastric marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. Blood. 2003;101:2489-2495. [PubMed] |
| 2. | Doolabh N, Anthony T, Simmang C, Bieligk S, Lee E, Huber P, Hughes R, Turnage R. Primary colonic lymphoma. J Surg Oncol. 2000;74:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Barron BA, Localio SA. A statistical note on the association of colorectal cancer and lymphoma. Am J Epidemiol. 1976;104:517-522. [PubMed] |
| 4. | Chakravartty S, Chattopadhyay G, Ray D, Choudhury CR, Mandal S. Concomitant tuberculosis and carcinoma colon: coincidence or causal nexus? Saudi J Gastroenterol. 2010;16:292-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Jain BK, Chandra SS, Narasimhan R, Ananthakrishnan N, Mehta RB. Coexisting tuberculosis and carcinoma of the colon. Aust N Z J Surg. 1991;61:828-831. [PubMed] |
| 6. | Tanaka K, Kondo S, Hattori F, Yamashita Y, Matsuda M, Itoh K, Okada Y, Kojima K, Nakagami K, Suzuki H. A case of colonic carcinoma associated with intestinal tuberculosis, and an analysis of 26 cases reported in Japan. Gan No Rinsho. 1987;33:1117-1123. [PubMed] |
| 7. | Falagas ME, Kouranos VD, Athanassa Z, Kopterides P. Tuberculosis and malignancy. QJM. 2010;103:461-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Devi P, Pattanayak L, Samantaray S. Synchronous adenocarcinoma and mucosa-associated lymphoid tissue lymphoma of the colon. Saudi J Gastroenterol. 2011;17:69-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Argyropoulos T, Foukas P, Kefala M, Xylardistos P, Papageorgiou S, Machairas N, Boltetsou E, Machairas A, Panayiotides IG. Simultaneous occurrence of colonic adenocarcinoma and MALT lymphoma: A series of three cases. World J Gastrointest Oncol. 2012;4:89-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Shaheen S, Guddati AK. Secondary mucosa-associated lymphoid tissue (MALT) lymphoma of the colon. Med Oncol. 2013;30:502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |