Published online Aug 15, 2013. doi: 10.4251/wjgo.v5.i8.177
Revised: August 12, 2013
Accepted: August 13, 2013
Published online: August 15, 2013
Processing time: 103 Days and 4.6 Hours
Neuroendocrine tumors are rare neoplasms that infrequently metastasize to the orbit. Given that patients with these tumors may have prolonged survival despite dissemination, maintaining quality of life by providing early diagnosis and effective treatment to preserve vision and comfort is a fundamental issue. We report the case of a 79-year old woman who presented with well-differentiated metastatic neuroendocrine tumor to the liver with no carcinoid syndrome and was started on intramuscular long-acting octreotide with disease stabilization. Two years later she developed right-sided diplopia associated with mild eye discomfort, proptosis and reddening. An magnetic resonance imaging showed a 2.1 cm mass in the right orbit and further biopsy confirmed a neuroendocrine tumor metastasis. The patient was treated with a four-week course of stereotactic radiotherapy to the right orbital metastasis (4000 cGy in 20 fractions) with minor conjunctivitis as the only side effect. Eighteen months later, she remains well with no visual loss.
Core tip: Neuroendocrine tumors are rare neoplasms that only uncommonly metastasize to the orbit. Given these tumors are associated with prolonged survival despite dissemination, maintaining quality of life by providing early diagnosis and effective treatment to preserve vision and comfort is a fundamental issue. We report the case of a patient who 2 years after the diagnosis of metastaic neuroendocrine tumor to the liver presented with right-sided diplopia. She was found to have metastatic neuroendocrine tumor to the right orbit and was successfully treated with radiotherapy. Eighteen months later, she remains well and with no visual loss.
- Citation: Peixoto RD, Lim HJ, Cheung WY. Neuroendocrine tumor metastatic to the orbit treated with radiotherapy. World J Gastrointest Oncol 2013; 5(8): 177-180
- URL: https://www.wjgnet.com/1948-5204/full/v5/i8/177.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v5.i8.177
Carcinoid tumors are low grade neoplasms usually arising from neuroendocrine cells of the bronchial and gastrointestinal tracts[1,2]. Although carcinoid tumors metastasize in 50%-75% of patients with the most common sites being lymph nodes, liver, and bones[1-3], metastases to the eyes and orbits have only rarely been reported[3-6] and are believed to occur through hematogeneous spread via carotid and ophthalmic artery. Improved patient survival, vigilant surveillance and advances in diagnostic tests have led to increased detection of orbital metastases. We report the case of a patient who 2 years after the diagnosis of metastatic neuroendocrine tumor to the liver presented with right-sided diplopia. She was found to have metastatic neuroendocrine tumor to the right orbit and was successfully treated with radiotherapy.
JVD is a 79-year-old Black woman who presented with small bowel obstruction. A computerized tomography (CT) scan showed a mesenteric mass with possible central necrosis as well as multiple low attenuating hepatic lesions. This prompted an ultrasound-guided fine needle aspiration of the liver nodule which confirmed a well-differentiated neuroendocrine tumor (< 2 mitoses per 10 hpf, Ki-67 index 8%, and strongly positive for synaptophysin and chromogranin). Additional investigations demonstrated an elevated 24-h urine 5-Hydroxyindoleacetic acid (133 μmol/d) but normal chromogranin A (27 U/L). An octreotide scan revealed increased uptake within the mesentery as well as the liver. The patient was placed on intramuscular long-acting octreotide 20 mg every 4 wk. A subsequent CT scan showed mild interval progression, prompting an increase in dose of octreotide to 40 mg every 4 wk. Follow-up CT scans showed stable disease. The patient did not report any carcinoid symptoms.
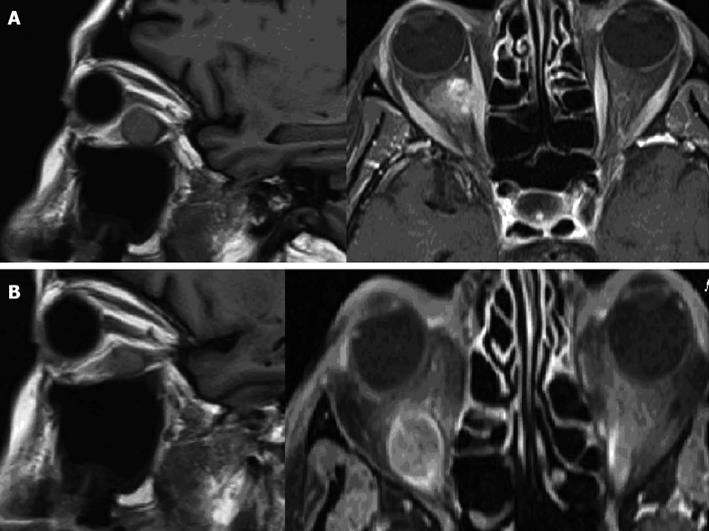
Approximately 2 years after her initial diagnosis, the patient developed right-sided diplopia associated with mild discomfort. On examination, right-sided proptosis and reddening were noted. She underwent a magnetic resonance imaging (MRI) of the head, which showed a homogeneously enhancing well-circumscribed 2.1 cm × 1.4 cm × 1.9 cm mass in the inferomedial right orbit, located between the orbital floor and inferior rectus muscle (Figure 1A). The radiographic findings were highly supportive for metastatic orbital spread from her original carcinoid tumor and a further orbital aspiration biopsy confirmed the diagnosis of low-grade neuroendocrine tumor. She underwent a four-week course of stereotactic radiotherapy to the right orbital metastasis (4000 cGy in 20 fractions) with minor conjunctivitis as the only complication.
At that time she was found to have progression of the disease in the liver as well as a new focus of metastases in the left ventricular myocardial wall. Soon after the completion of palliative radiation therapy to the right orbital metastasis, she was started on palliative Capecitabine and Temozolamide. Three months later a new MRI showed reduction in the size of the orbital lesion to 1.5 cm × 1.5 cm × 1.2 cm and there was improvement of the diplopia (Figure 1B). Eighteen months after receiving radiation therapy the patient remains stable with only mild diplopia and without any vision deterioration.
Carcinoid tumors are mostly low grade neoplasms arising from neuroendocrine cells of the bronchial and gastrointestinal tracts and rarely from other tissues[1,2]. Although originally thought to be of low malignant potential, clinically evident carcinoid tumors metastasize in 50%-75% of patients with the most common sites being surrounding lymph nodes, the liver, and bone[1-3]. Carcinoid tumor metastases to the eye and orbit have been reported only rarely[3-6] and typically occur through hematogeneous spread via carotid and ophthalmic artery. However, improved patient survival, vigilant surveillance and advances in diagnostic tests have led to increased detection of orbital metastases.
Classically, the diagnosis of ocular metastases is mainly suspected on the basis of a prior history of neuroendocrine tumor, evidence of other systemic metastases, and/or clinical symptoms of carcinoid syndrome[3,4]. Diplopia (48%), pain (42%), and visual loss (30%) are the commonest symptoms at presentation, whereas proptosis (63%), strabismus (62%), and visual loss (41%) are the most frequent signs[7]. MRI is considered the diagnostic image of choice in evaluating suspected orbital metastases.
Data regarding survival after the diagnosis of ocular metastatic carcinoid tumor are scarce. In a series of 13 cases, the overall survival was 72% at 5 years and 38% at 10 years[8]. Given that patients with carcinoid tumors may have prolonged survival despite dissemination, maintaining quality of life by providing early diagnosis and effective treatment to preserve vision and comfort is a fundamental issue[9]. Although primary orbital tumors require total surgical excision, metastases to the uvea and the orbit are frequently associated with widespread disease, in which case other therapeutic modalities appear to be more appropriate[2]. In the largest series consisting of 13 patients with carcinoid orbital metastaes, 4 underwent exenteration, 5 had radiotherapy after tumor debulking, 2 had radiotherapy alone, and 2 had local radiotherapy with receptor-targeted chemotherapy[8].
The generally accepted treatment of orbital metastatic disease is with irradiation and/or chemotherapy[10], although serial observation may be appropriate in asymptomatic slow-growing tumors without vision deterioration. External beam irradiation may be an effective and noninvasive tool in selected cases[11,12], especially for single and symptomatic lesions. Side effects may include skin erythema, conjunctivitis, corneal ulceration, cataract formation, retinopathy and neuropathy[13,14]. Data regarding tumor response and symptom relief of ocular metastatic carcinoid tumor after palliative radiotherapy is non-existent.
Another potential treatment option for metastatic carcinoid tumors to the orbit is radiopharmaceuticals. Its main advantage is the treatment of disseminated lesions in a variety of sites, and the dose may be repeated as required. Regression of choroidal metastases after chemotherapy has also been described[15]. One case of successfully treated choroidal metastases from a bronchial carcinoid with xenon arc photocoagulation and proton beam irradiation has also been reported[16]. In addition, the combination of chemotherapy with external beam radiotherapy may be associated with symptomatic improvement and stabilization of the lesions with minimal adverse effects[5].
In conclusion, metastatic neuroendocrine tumors to the orbit are rare, but usually associated with important symptoms that compromise patients’ well-being. Because neuroendocrine tumors tend to have an indolent course with prolonged survival, early treatment of orbit metastases may help maintain quality of life.
P- Reviewer Roy PK S- Editor Wen LL L- Editor A E- Editor Lu YJ
| 2. | Modlin IM, Sandor A. An analysis of 8305 cases of carcinoid tumors. Cancer. 1997;79:813-829. [PubMed] |
| 3. | Harbour JW, De Potter P, Shields CL, Shields JA. Uveal metastasis from carcinoid tumor. Clinical observations in nine cases. Ophthalmology. 1994;101:1084-1090. [PubMed] |
| 4. | Riddle PJ, Font RL, Zimmerman LE. Carcinoid tumors of the eye and orbit: a clinicopathologic study of 15 cases, with histochemical and electron microscopic observations. Hum Pathol. 1982;13:459-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 40] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Isidori AM, Kaltsas G, Frajese V, Kola B, Whitelocke RA, Plowman PN, Britton KE, Monson JP, Grossman AB, Besser GM. Ocular metastases secondary to carcinoid tumors: the utility of imaging with [(123)I]meta-iodobenzylguanidine and [(111)In]DTPA pentetreotide. J Clin Endocrinol Metab. 2002;87:1627-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Zimmerman LE, Stangl R, Riddle PJ. Primary carcinoid tumor of the orbit. A clinicopathologic study with histochemical and electron microscopic observations. Arch Ophthalmol. 1983;101:1395-1398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Valenzuela AA, Archibald CW, Fleming B, Ong L, O’Donnell B, Crompton J J, Selva D, McNab AA, Sullivan TJ. Orbital metastasis: clinical features, management and outcome. Orbit. 2009;28:153-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 8. | Mehta JS, Abou-Rayyah Y, Rose GE. Orbital carcinoid metastases. Ophthalmology. 2006;113:466-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Caplin ME, Buscombe JR, Hilson AJ, Jones AL, Watkinson AF, Burroughs AK. Carcinoid tumour. Lancet. 1998;352:799-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 243] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 10. | Shields CL, Shields JA, Eagle RC, Peyster RG, Conner BE, Green HA. Orbital metastasis from a carcinoid tumor. Computed tomography, magnetic resonance imaging, and electron microscopic findings. Arch Ophthalmol. 1987;105:968-971. [PubMed] |
| 11. | Bardenstein DS, Char DH, Jones C, Crawford JB, Miller TR, Riekhof FT. Metastatic ciliary body carcinoid tumor. Arch Ophthalmol. 1990;108:1590-1594. [PubMed] |
| 12. | Rush JA, Waller RR, Campbell RJ. Orbital carcinoid tumor metastatic from the colon. Am J Ophthalmol. 1980;89:636-640. [PubMed] |
| 13. | Ahmad SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr Opin Ophthalmol. 2007;18:405-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 175] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 14. | Rosset A, Zografos L, Coucke P, Monney M, Mirimanoff RO. Radiotherapy of choroidal metastases. Radiother Oncol. 1998;46:263-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Fan JT, Ortiz RG, Buettner H. Regression of choroidal metastases from a bronchial carcinoid tumor after chemotherapy with cisplatin and etoposide. Am J Ophthalmol. 1994;117:111-113. [PubMed] |
| 16. | Gragoudas ES, Carroll JM. Multiple choroidal metastasis from bronchial carcinoid treated with photocoagulation and proton beam irradiation. Am J Ophthalmol. 1979;87:299-304. [PubMed] |