Published online Mar 15, 2013. doi: 10.4251/wjgo.v5.i3.68
Revised: January 17, 2013
Accepted: January 23, 2013
Published online: March 15, 2013
Processing time: 127 Days and 8.8 Hours
Retroperitoneal fibrosis secondary to malignant disease is a rare condition associated with a dismal prognosis. We herein present the first ever reported case of retroperitoneal fibrosis related to esophageal adenocarcinoma in a 63-year-old patient who developed bilateral ureteral obstruction due to extensive retroperitoneal fibrosis 18 mo after having completed neoadjuvant chemoradation followed by surgery for a pT3N0 adenocarcinoma of the distal esophagus. We also report the case of a previously healthy woman who presented with bilateral ureteral obstruction and diffuse narrowing of the common biliary duct and was found to have extensive retroperitoneal fibrosis as a consequence of metastatic gastric adenocarcinoma. Both patients had poor performance status and were unsuitable for palliative chemotherapy. This paper shows that urinary and biliary obstructive symptoms might represent retroperitoneal fibrosis as a consequence of gastroesophageal malignancy.
- Citation: Peixoto RD, Al-Barrak J, Lim H, Renouf D. Gastroesophageal cancer and retroperitoneal fibrosis: Two case reports and review of the literature. World J Gastrointest Oncol 2013; 5(3): 68-70
- URL: https://www.wjgnet.com/1948-5204/full/v5/i3/68.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v5.i3.68
Retroperitoneal fibrosis is a rare clinical condition characterized by the presence of pathologic collagen plaque around the abdominal aorta and iliac vessels, as well as the inferior vena cava and the ureters. Approximately 70% of retroperitoneal fibrosis is idiopathic in nature, while the remaining 30% are believed to be related to certain drugs (ergot-derivatives, methysergide, bromocriptine, beta-blockers, methyldopa, analgesics, hydralazine), malignancy (carcinoid, lymphoma, sarcoma, carcinomas of the colon, prostate, breast, stomach), infections (tuberculosis, histoplasmosis, actinomycosis), radiotherapy (testicular seminoma, colon carcinoma, pancreatic carcinoma), surgery (lymphadenectomy, colectomy, hysterectomy, aortic aneurysmectomy), trauma, amyloidosis[1,2]. From our knowledge, there are only nine reported cases of retroperitoneal fibrosis associated with gastric cancer[3-11], while there is no report associated with esophageal cancer.
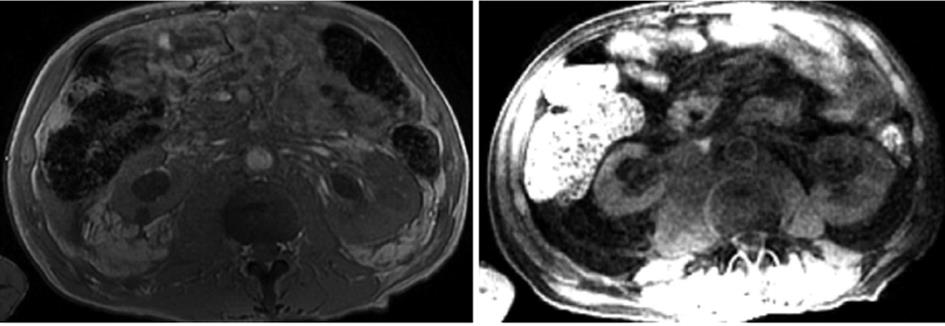
A 63 year-old man with a past history of pT3N0 adenocarcinoma of the distal esophagus treated with neoadjuvant chemoradiation (5 wk of chemoradiation at dose 50.4 Gy with cisplatin 25 mg/m2 days 1-3 and 5-fluorouracil 1000 mg/m2 daily × 4, weeks 1 and 5) followed two-hole esophagectomy with gastric reconstruction presented 18 mo after the completion of treatment with acute kidney injury caused by bilateral ureteral obstruction. Bilateral nephrostomy tubes were placed. Magnetic resonance imaging of the abdomen revealed an ill-defined retroperitoneal infiltrate extending from the level of the renal vessels towards the presacral space distally demonstrating retroperitoneal fibrosis (Figure 1). The patient underwent a biopsy of the retroperitoneum which showed poorly differentiated adenocarcinoma consistent with metastasis from the previous esophageal cancer.
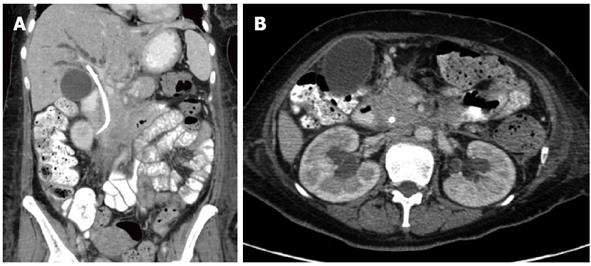
A previously healthy 54-year-old woman who presented to the emergency department with a 4-wk history of flank pain, persistent nausea with vomiting, anorexia and progressive oliguria as well as intermittent hematuria. The patient was found to have bilateral hydronephrosis due to ureteral obstruction with consequent renal insufficiency and underwent bilateral nephrostomy. Shortly after admission, she also became jaundiced. Subsequent work-up revealed diffuse narrowing of the common biliary duct and a biliary stent was inserted. A liver biopsy was consistent with cholestasis and immunoglobulin G4 level was normal. Computed tomography (CT) scan of the abdomen showed extensive retroperitoneal soft tissue mass, extending all the way up to the liver hilum as well as diffusely narrowed caliber of the inferior vena cava and portal vein (Figure 2). These findings were consistent with retroperitoneal fibrosis. During an attempt to an endoscopic-ultrasound guided fine-needle aspiration of the retroperitoneum mass, she was found to have thickening of the gastric wall. Gastric biopsy revealed invasive adenocarcinoma in a scenario of linitis plastica while the ascetic fluid revealed malignant cells.
Symptoms caused by this fibrotic process are usually secondary to compression and constriction of local anatomic structures. The most frequent presenting symptom is pain in the lower back, flank or abdomen, which tends to increase over time[12]. Other common symptoms include weight loss, anorexia, testicular pain, edema, and gross hematuria[2]. In late stages, patients may develop progressive ureteral obstruction with renal insufficiency due to encasement of both ureters by the retroperitoneal mass. More rarely, involvement of the biliary tree by the fibrotic tissue may cause obstructive jaundice[13], as was the case of our second patient.
In most cases of retroperitoneal fibrosis secondary to malignant disease, abnormal collagen plaque in the retroperitoneum results from an exuberant desmoplastic response to retroperitoneal metastases[2]. It is believed to be an immune-mediated process, in which macrophages release cytokines that stimulate fibroblast proliferation with subsequent fibrosis. However, its etiology and pathobiology remain obscure. This mechanism is different in carconoid tumors, which may lead to retroperitoneal fibrosis without the presence of metastasis probably through a serotonin-mediated mechanism[14]. Another possible explanation for carcinoid-induced retroperitoneal fibrosis is the release of profibrogenic growth factors such as platelet-derived growth factor, insulin-like growth factors, epidermal growth factor, and the family of transforming growth factors α and β[15].
The diagnosis of retroperitoneal fibrosis is primarily made by imaging studies. Contrast-enhanced CT scan is the method of choice as it visualizes the extent of fibrosis and may assess the presence of metastatic tumor. Moreover, CT scan may also enable CT-guided biopsy[16]. Positron emission tomography (PET)-CT has recently been reported as a useful imaging modality in idiopathic retroperitoneal fibrosis, not only for diagnosis but also for treatment response evaluation[17]. Because retroperitoneal fibrosis is a metabolically active tissue, it will show increased radiotracer uptake, irrespective of a malignant or idiopathic cause. However, PET-CT scan may reveal an occult primary tumor as well as metastatic disease. Biopsy of the retroperitoneum is highly recommended if there is suspicion for an underling malignancy.
Usually retroperitoneal fibrosis secondary to malignant disease is associated with a dismal prognosis. The nonspecific symptoms often make the diagnosis very difficult and during late stages patients may have organ dysfunction and poor performance status, being unsuitable for palliative chemotherapy. Both of our patients were not able to undergo chemotherapy. Unfortunately, there is no evidence in the literature that chemotherapy would help reducing malignancy-related retroperitoneal fibrosis. The decision to offer chemotherapy must be done from case to case, taking into consideration performance status and organ dysfunction. Although corticosteroids are the most used drugs for idiopathic retroperitoneal fibrosis, there is no evidence of effectiveness when retroperitoneal fibrosis is secondary to malignancy. The only exception is retroperitoneal fibrosis related to carcinoid tumors, which can achieve great response to corticosteroids[14].
Despite the lack of effective systemic options for the management of retroperitoneal fibrosis associated with malignancy, these patients might draw benefit from palliative surgical approaches in order to relieve obstructive complications. Moreover, pain management is of great importance.
In summary, retroperitoneal fibrosis secondary to malignant disease is a rare condition associated with a dismal prognosis. Organ dysfunction and poor performance status usually preclude the use of systemic chemotherapy.
P- Reviewer Aprile G S- Editor Gou SX L- Editor A E- Editor Lu YJ
| 1. | van Bommel EF, Jansen I, Hendriksz TR, Aarnoudse AL. Idiopathic retroperitoneal fibrosis: prospective evaluation of incidence and clinicoradiologic presentation. Medicine (Baltimore). 2009;88:193-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 160] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 2. | Vaglio A, Salvarani C, Buzio C. Retroperitoneal fibrosis. Lancet. 2006;367:241-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 496] [Cited by in RCA: 469] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 3. | Yokoyama R, Tazaki R, Morita H, Nishitani H, Ariumi S, Osuga S, Sohmiya K, Kono T, Narumi Y, Tsuji M. Retroperitoneal fibrosis in a patient with gastric cancer manifested by lower extremity edema and hydrocele. Intern Med. 2012;51:2157-2160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Karbasi A, Karbasi-Afshar R, Ahmadi J, Saburi A. Retroperitoneal fibrosis as a result of signet ring cell gastric cancer: a case-based review. J Gastrointest Cancer. 2013;44:94-97. [PubMed] |
| 5. | Usher SM, Brendler H, Ciavarra VA. Retroperitoneal fibrosis secondary to metastatic neoplasm. Urology. 1977;9:191-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Thomas MH, Chisholm GD. Retroperitoneal fibrosis associated with malignant disease. Br J Cancer. 1973;28:453-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Dohmen K, Mizukami Y, Tanaka K, Nakamura H, Arase K, Yokogawa Y, Asayama R, Kato A, Kato M, Nakagaki M. Retroperitoneal fibrosis associated with scirrhous gastric cancer. Gastroenterol Jpn. 1993;28:699-705. [PubMed] |
| 8. | Yashiro M, Chung YS, Nishimura S, Inoue T, Sowa M. Fibrosis in the peritoneum induced by scirrhous gastric cancer cells may act as “soil” for peritoneal dissemination. Cancer. 1996;77:1668-1675. [PubMed] |
| 9. | Landaluce Olavarria A, Estraviz Mateos B, Gamarra Quintanilla M, Goicoechea Artola JM, Sarabia García S. [Gastric neoplasm and retroperitoneal fibrosis. A marker of poor prognosis?]. Cir Esp. 2007;81:109-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Amrouche L, Gornet JM, Lascoux C, George C, Florea L, Farge D, Séréni D, Bourgarit A. [From retroperitoneal fibrosis to gastric linitis]. Rev Med Interne. 2009;30:443-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Pérez OI, Lizarralde ZL, de Pierola BF, García AL, Crespo CI. [Retroperitoneal fibrosis secondary to gastric neoplasia]. Actas Urol Esp. 2008;32:345-347. [PubMed] |
| 12. | van Bommel EF. Retroperitoneal fibrosis. Neth J Med. 2002;60:231-242. [PubMed] |
| 13. | Renner IG, Ponto GC, Savage WT, Boswell WD. Idiopathic retroperitoneal fibrosis producing common bile duct and pancreatic duct obstruction. Gastroenterology. 1980;79:348-351. [PubMed] |
| 14. | Chander S, Ergun EL, Chugani HT, Chugani DC, Juhasz C, Shields AF, Weaver DW. High 2-deoxy-2-[18F]fluoro-D-glucose accumulation in a case of retroperitoneal fibrosis following resection of carcinoid tumor. Mol Imaging Biol. 2002;4:363-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Modlin IM, Shapiro MD, Kidd M. Carcinoid tumors and fibrosis: an association with no explanation. Am J Gastroenterol. 2004;99:2466-2478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 81] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 16. | Amis ES. Retroperitoneal fibrosis. AJR Am J Roentgenol. 1991;157:321-329. [PubMed] |
| 17. | Treglia G, Mattoli MV, Bertagna F, Giubbini R, Giordano A. Emerging role of Fluorine-18-fluorodeoxyglucose positron emission tomography in patients with retroperitoneal fibrosis: a systematic review. Rheumatol Int. 2013;33:549-555. [PubMed] |