Published online Dec 15, 2013. doi: 10.4251/wjgo.v5.i12.235
Revised: November 12, 2013
Accepted: November 18, 2013
Published online: December 15, 2013
Processing time: 91 Days and 0.7 Hours
Pancreatic cancer is an aggressive malignancy potentially curable with surgical intervention. Following pancreaticoduodenectomy for suspected pancreatic head malignancy, patients have a high risk for both immediate and delayed problems due to surgical complications and recurrent disease. We report here a patient with pancreatic cancer treated with pancreaticoduodenectomy who developed recurrent disease resulting in obstruction of the afferent limb. The patient developed biliary obstruction and cholangitis at presentation. Her biliary tree failed to dilate which precluded safe percutaneous biliary decompression. During surgical exploration, she was found to have a dilated afferent limb at the level of the transverse mesocolon. The patient underwent decompression of the afferent limb as well as the biliary tree using a venting gastrojejunostomy to the blind loop. This represents a novel surgical approach for management of this complicated and difficult problem.
Core tip: Complications from recurrent pancreatic cancer can result in afferent loop obstruction. This leads to stasis of the biliary, intestinal and pancreatic secretions. We present here a unique approach to manage afferent loop obstruction caused by recurrent peritoneal metastases from pancreatic cancer. The patient underwent decompression of the afferent limb as well as the biliary tree using a venting gastrojejunostomy to the blind loop. This represents a novel surgical approach for management of this complicated and difficult problem.
- Citation: Bakes D, Cain C, King M, Dong XD(. Management of afferent loop obstruction from recurrent metastatic pancreatic cancer using a venting gastrojejunostomy. World J Gastrointest Oncol 2013; 5(12): 235-239
- URL: https://www.wjgnet.com/1948-5204/full/v5/i12/235.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v5.i12.235
Pancreatic cancer is the fourth leading cause of cancer in the United States[1]. Pancreaticoduodenectomy (Whipple procedure) remains a mainstay of treatment for resectable pancreatic head malignancy. Unfortunately, the incidence of recurrent disease remains high with frequent peritoneal metastases[1-3]. Complications from recurrent disease range from bowel obstruction, pancreatitis, sepsis, and cholangitis due to biliary obstruction[2-4]. A unique type of obstruction occurs at the retrocolic jejunal limb of the afferent loop which can lead to stasis of the biliary, intestinal and pancreatic secretions[3-6]. We present here a case of afferent loop obstruction caused by recurrent peritoneal metastases from pancreatic cancer.
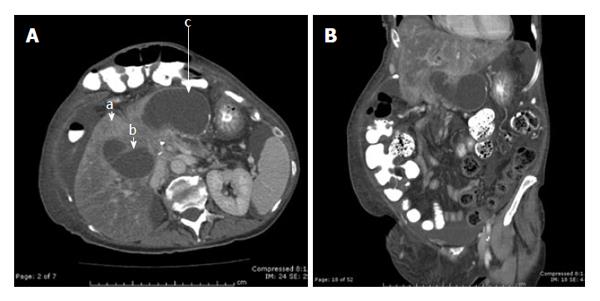
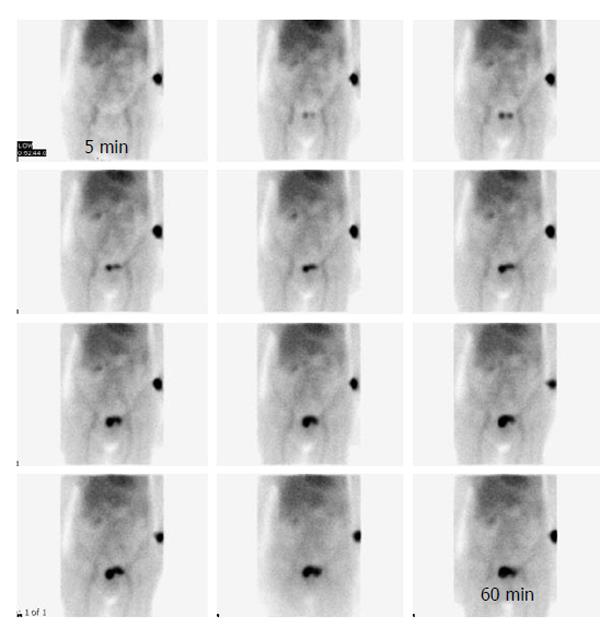
The patient was a 70-year-old Caucasian female who first presented with painless jaundice leading to the diagnosis of pancreatic cancer. The patient underwent a pancreaticoduodenectomy at an outside institution for management of her condition followed by adjuvant chemotherapy and radiation. The patient required another operation a year later due to an episode of small bowel obstruction, complicated with postoperative development of a small enterocutaneous fistula along with a large ventral hernia. She then presented to our hospital 2 years from her pancreaticoduodenectomy procedure with new onset abdominal pain along with jaundice. The patient had evidence of cholangitis with fevers, chills, leukocytosis of 21700/mm3 and a bilirubin level of 16.0 mg/dL. Preoperative imaging, including a computed tomographic scan, showed severely dilated afferent limb in the right upper quadrant (Figure 1). A cholescintigraphy (DISIDA) scan showed poor visualization of the liver even 2.5 h after isotope injection suggesting intrinsic liver dysfunction (Figure 2). Her case was complicated by the lack of significant biliary dilatation precluding the use of interventional radiology techniques to percutaneously manage her cholangitis. Therefore, the patient underwent surgical exploration for management of her afferent loop obstruction. Intraoperative findings showed the obstruction to be secondary to a tight stricture at the jejunal limb as it traversed the mesentery of the colon. Biopsy of the area confirmed peritoneal recurrence from pancreatic cancer. The presence of the small enterocutaneous fistula at the level of mid-jejunum precluded the use of another small bowel loop for Roux-en-Y reconstruction. Because of the proximity of the stomach to the dilated afferent limb, we employed a primary anastomosis between the dilated afferent limb and the lesser curvature of the stomach as a venting gastrojejunostomy. The patient also had primary repair of her incisional hernia without the use of a mesh. She recovered uneventfully from surgery and was discharged from the hospital to rehabilitation center following 10 d. Her bilirubin level slowly improved and tapered off to a level of 4.1 mg/dL about 35 d postoperatively. The patient eventually succumbed to her metastatic pancreatic cancer 4 mo later.
Complications from advanced pancreatic cancer remain common. After pancreaticoduodenectomy for resectable pancreatic cancer, patients present with substantial morbidity following chemotherapy and radiation along with the effects of recurrent pancreatic cancer[1,2]. Jacobs et al[3] noted that even long term survivors of pancreatic cancer develop multiple complications including infection, diabetes, depression, bowel obstruction and other malignancies[4]. Although not well described until more recently, the incidence of afferent loop syndrome developing in a cohort of patients after pancreaticoduodenectomy may be as high as 13%, as described by Pannala et al[5] from Virginia Mason Medical Center. The occurrence of this uncommon condition has been well described in the literature following gastrectomy with Billroth II reconstruction, with an incidence of 0.5%-2%[6].
Clinical and radiographic presentations associated with this condition have been separated into acute and chronic afferent loop obstruction[6-11]. Acute and chronic afferent loop syndromes differ by the timing of presentation with the acute afferent loop syndrome more often in the postoperative period and the chronic type presenting years later[6-11]. The first case of afferent loop syndrome was described by McNealy et al[12] in 1942 as a cause of early postoperative duodenal stump leak. Roux et al[12] eventually coined the terms afferent loop syndrome in 1950.
Pancreaticoduodenectomy employs a roux limb of jejunum for reconstruction of the pancreatic and biliary drainage. Since the reconstruction following a pancreaticoduodenectomy employs an afferent limb for drainage of the bile, pancreatic and proximal intestinal secretions, it is functionally similar and also frequently termed afferent loop obstruction in the literature when obstructed[11]. However, the etiology, clinical presentation, and management options can vary from those following gastric surgeries.
The presentation of a roux limb obstruction is associated with high rates of morbidity and mortality[7,8]. Patients are frequently malnourished due to long standing history of underlying malignancy. The most common presenting symptom following pancreaticoduodenectomy is cholangitis at 50% followed by nausea and abdominal pain[5]. The presentation is different from those following gastric surgeries, which is exemplified by bilious vomiting for chronic afferent loop obstruction. Complicating the presentation is that patients with pancreatic cancer frequently have a poor long term prognosis which frequently leads to a minimalist approach for management of these patients.
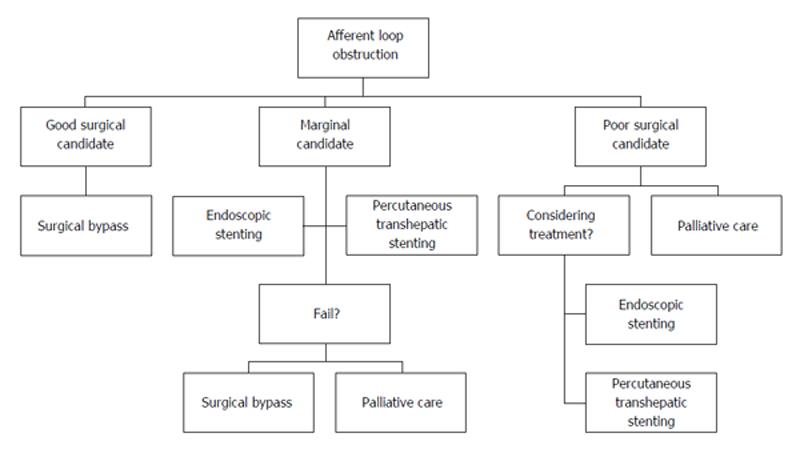
Prior to the introduction of endoscopic and percutaneous techniques, initial management options for afferent loop obstruction were first centered on surgical approaches. However, surgical approaches are limited due to the location of the Roux limb, which is through the mesentery of the colon. Resection of the obstructed afferent loop is a poor choice because of the necessity for reconstruction of both the pancreatic and biliary anastomoses. In addition, an in situ jejuno-jejunal bypass at the obstructed site is not feasible because of the vascular anatomy. Therefore, the most common approaches described in the literature involved the use of another jejunal Roux limb to decompress the dilated afferent loop[7,8,13]. Recently, advances in endoscopic and percutaneous techniques have been described in the literature to offer options for management of these patients[14-19]. More commonly, biliary decompression by interventional radiology manages to treat the acute cholangitis seen in these patients[15-17]. In addition, successful endoscopic stenting with dual stents of the stenotic segment avoids external drains and its associated long term problems[17,19]. Even transgastric drainage endoscopically has been reported recently[18]. Unfortunately, long term survival is usually unaffected regardless of the approach employed for salvage of this situation. As shown in Figure 3, we provided an algorithm for the management of these patients based on their medical co-morbidities.
The case presented here is a long term complication following pancreaticoduodenectomy, frequently seen for recurrent disease[5]. In the case described here, our patient presented several unique challenges precluding the use of conservative and traditional surgical approaches. Our patient lacked biliary dilatation on the CT imaging which precluded the use of interventional radiology as a means for biliary decompression. Furthermore, the presence of enterocutaneous fistula, albeit small, made another Roux limb not feasible during surgery due to the lost of additional length of small bowel following resection and reconstruction. Our approach for performing a venting gastrojejunostomy was an idea developing following preoperative imaging review and surgical planning. The dilated jejunal Roux limb was in close proximity of the stomach making the anastomosis rather straight forward. Our goal of extending the life of our patient was also accomplished without significant postoperative morbidity. The patient lived approximately 4 mo postoperatively, which is consistent with the historically described outcome for this disease.
In summary, recurrent pancreatic cancer is associated with a poor prognosis. Afferent loop syndrome is a known complication from recurrent pancreatic cancer, with the classic radiographic presentations of a dilated small bowel loop and clinical evidence of cholangitis due to failure of biliary excretion. Early recognition of this serious condition, due to the ascending cholangitis, can lead to prompt management. Management options are evolving with improved endoscopic techniques and percutaneous options. However, surgery remains a viable option in appropriate candidates to establish a lasting decompression of the dilated Roux limb.
Afferent loop syndrome is a known complication from recurrent pancreatic cancer, with the classic radiographic presentations of a dilated small bowel loop and clinical evidence of cholangitis due to failure of biliary excretion.
A unique type of biliary obstruction following pancreaticoduodenectomy occurs at the retrocolic jejunal limb of the afferent loop, leading to stasis of the biliary, intestinal and pancreatic secretions.
Complications from recurrent pancreatic cancer range from bowel obstruction, pancreatitis, sepsis, and cholangitis due to biliary obstruction.
Patients typically have evidence of cholangitis with fevers, chills, leukocytosis and hyperbilirubinemia.
Radiographic imaging using a computed tomographic scan typically shows a severely dilated afferent limb in the right upper quadrant.
Management of afferent loop syndrome has traditional relied on surgical approaches using another jejunal Roux limb. However, recent advances in endoscopic and percutaneous techniques have been described in the literature to offer other options for management of these patients.
Early recognition of afferent loop syndrome can lead to prompt management using endoscopic, percutaneous, or surgical techniques to decompress the dilated Roux limb.
The manuscript is well-written, concise and easy to comprehend. Venting Gastrojejunostomy for recurrent pancreatic cancer has not been described before.
P- Reviewer: Giannopoulos GA S- Editor: Zhai HH L- Editor: A E- Editor: Liu XM
| 1. | Hariharan D, Saied A, Kocher HM. Analysis of mortality rates for pancreatic cancer across the world. HPB (Oxford). 2008;10:58-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 249] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 2. | Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA, Hickey H, Beger H, Fernandez-Cruz L, Dervenis C, Lacaine F. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004;350:1200-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1945] [Cited by in RCA: 1909] [Article Influence: 90.9] [Reference Citation Analysis (0)] |
| 3. | Jacobs NL, Que FG, Miller RC, Vege SS, Farnell MB, Jatoi A. Cumulative morbidity and late mortality in long-term survivors of exocrine pancreas cancer. J Gastrointest Cancer. 2009;40:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Reid-Lombardo KM, Ramos-De la Medina A, Thomsen K, Harmsen WS, Farnell MB. Long-term anastomotic complications after pancreaticoduodenectomy for benign diseases. J Gastrointest Surg. 2007;11:1704-1711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 112] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 5. | Pannala R, Brandabur JJ, Gan SI, Gluck M, Irani S, Patterson DJ, Ross AS, Dorer R, Traverso LW, Picozzi VJ. Afferent limb syndrome and delayed GI problems after pancreaticoduodenectomy for pancreatic cancer: single-center, 14-year experience. Gastrointest Endosc. 2011;74:295-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Mitty WF, Grossi C, Nealon TF. Chronic afferent loop syndrome. Ann Surg. 1970;172:996-1001. [PubMed] |
| 7. | Aimoto T, Uchida E, Nakamura Y, Katsuno A, Chou K, Tajiri T, Naito Z. Malignant afferent loop obstruction following pancreaticoduodenectomy: report of two cases. J Nippon Med Sch. 2006;73:226-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Spiliotis J, Karnabatidis D, Vaxevanidou A, Datsis AC, Rogdakis A, Zacharis G, Siamblis D. Acute cholangitis due to afferent loop syndrome after a Whipple procedure: a case report. Cases J. 2009;2:6339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Lalla M, Arregui M. Afferent loop syndrome after Whipple procedure. Scientific Session of the Society of American Gastrointestinal and Endoscopic Surgeons. 2009 Apr; Phoenix, Arizona, USA. Berlin: Springer 2009; 403. |
| 10. | Locke GR, Alexander GL, Sarr MG. Obstructive jaundice: an unusual presentation of afferent loop obstruction. Am J Gastroenterol. 1994;89:942-944. [PubMed] |
| 11. | Warrier RK, Steinheber FU. Afferent loop obstruction presenting as obstructive jaundice. Dig Dis Sci. 1979;24:74-76. [PubMed] |
| 12. | Roux G, Pedoussaut R, Marchal G. [Afferent loop syndrome of gastrectomized subjects]. Lyon Chir. 1950;45:773-780. [PubMed] |
| 13. | Bushkin FL, Woodward ER, O’Leary JP. Experience with the jejunal loop interposition in the treatment of postgastrectomy disorders. Am Surg. 1977;43:101-107. [PubMed] |
| 14. | Moriura S, Takayama Y, Nagata J, Akutagawa A, Hirano A, Ishiguro S, Matsumoto T, Sato T. Percutaneous bowel drainage for jaundice due to afferent loop obstruction following pancreatoduodenectomy: report of a case. Surg Today. 1999;29:1098-1101. [PubMed] |
| 15. | Hosokawa I, Kato A, Shimizu H, Furukawa K, Miyazaki M. Percutaneous transhepatic metallic stent insertion for malignant afferent loop obstruction following pancreaticoduodenectomy: a case report. J Med Case Rep. 2012;6:198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Gwon DI. Percutaneous transhepatic placement of covered, self-expandable nitinol stent for the relief of afferent loop syndrome: report of two cases. J Vasc Interv Radiol. 2007;18:157-163. [PubMed] |
| 17. | Caldicott DG, Ziprin P, Morgan R. Transhepatic insertion of a metallic stent for the relief of malignant afferent loop obstruction. Cardiovasc Intervent Radiol. 2000;23:138-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Matsumoto K, Kato H, Tomoda T, Sakakihara I, Yamamoto N, Noma Y, Sonoyama T, Tsutsumi K, Okada H, Yamamoto K. A case of acute afferent loop syndrome treated by transgastric drainage with EUS. Gastrointest Endosc. 2013;77:132-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Han K, Song HY, Kim JH, Park JH, Nam DH, Ryu MH, Yook JH. Afferent loop syndrome: treatment by means of the placement of dual stents. AJR Am J Roentgenol. 2012;199:W761-W766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |