Published online Aug 15, 2025. doi: 10.4251/wjgo.v17.i8.108016
Revised: May 28, 2025
Accepted: July 2, 2025
Published online: August 15, 2025
Processing time: 120 Days and 21 Hours
Serum carcinoembryonic antigen (CEA) levels and magnetic resonance imaging (MRI) findings are widely used for the diagnosis and treatment of rectal cancer; however, research investigating their correlation remains limited.
To investigate the correlation between baseline MRI features and serum CEA levels in patients diagnosed with primary rectal cancer.
Eighty patients (age: 42-78 years) diagnosed with primary rectal cancer were enrolled. Baseline MRI examinations were performed to evaluate tumor size, T stage, circumferential resection margin status, extramural vascular invasion (EMVI), and lymph node metastasis. Serum CEA levels were concurrently measured. Statistical methods were used to analyze correlations.
Tumor size, T stage, EMVI, and lymph node metastasis were significantly correlated with serum CEA levels (P < 0.05). Multivariate analysis identified T stage and lymph node metastasis as independent factors influencing serum CEA levels.
This study confirmed the correlation between baseline MRI features and serum CEA levels in patients with primary rectal cancer, highlighting their potential utility for precise diagnosis, staging, and prognostic evaluation.
Core Tip: The correlation between magnetic resonance imaging (MRI) features and serum carcinoembryonic antigen (CEA) levels for diagnosing and treating rectal cancer currently remains under investigation. Accordingly, the present study explored this association in 80 patients diagnosed with primary rectal cancer at the authors’ hospital between July 2022 and August 2024. Patients were grouped according to clinical characteristics and treatment plans, and analysis confirmed a strong correlation between baseline MRI features and serum CEA levels.
- Citation: Wang P, Zhao WN, Han J, Wang KX, Yang XF, Huang YJ. Correlation between baseline magnetic resonance imaging features and serum carcinoembryonic antigen levels in patients with primary rectal cancer. World J Gastrointest Oncol 2025; 17(8): 108016
- URL: https://www.wjgnet.com/1948-5204/full/v17/i8/108016.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i8.108016
Colorectal cancer, particularly rectal cancer, is among the most common malignancies of the digestive tract and poses a significant threat to human health[1]. In recent years, the incidence of rectal cancer has been increasing annually due to lifestyle changes and aging populations[2,3]. According to global cancer statistics, rectal cancer ranks among the leading malignancies in terms of both incidence and mortality worldwide, with a substantial number of new cases and deaths reported each year[4,5]. In China, rectal cancer remains a critical public health issue that imposes a heavy burden on patients, families, and society.
There are multiple challenges to the diagnosis and treatment of rectal cancer. Early stage rectal cancer often presents with nonspecific symptoms, leading to delayed diagnosis and a high proportion of patients diagnosed at advanced stages of disease, thereby missing optimal treatment opportunities[6,7]. Surgery remains the primary treatment modality; however, for cases involving locally advanced or metastatic disease, monotherapy using surgery yields suboptimal outcomes, necessitating multimodal approaches, such as chemoradiotherapy[8]. Although essential, these treatments are associated with physical and psychological distress, variable efficacies, and high recurrence rates. Consequently, identifying effective diagnostic and prognostic biomarkers to improve early detection and therapeutic outcomes has become a focal point in oncology research[9,10].
Serum carcinoembryonic antigen (CEA), a widely used tumor biomarker, plays a pivotal role in colorectal cancer management. CEA is an acidic glycoprotein with embryonic antigenic properties and is minimally expressed in healthy adults, but is markedly elevated in individuals diagnosed with colorectal cancer due to tumor cell proliferation and secretion. Studies suggest that CEA not only aids in auxiliary diagnosis but is also correlated with disease staging, therapeutic response evaluation, prognosis prediction, and recurrence monitoring[11-13]. For example, serum CEA levels are closely associated with tumor size, depth of invasion, and lymph node metastasis, with higher levels typically observed in the advanced stages of disease. Postoperative decline(s) in CEA levels may indicate therapeutic efficacy, whereas persistent or recurrent elevation often signals tumor relapse or metastasis. Nevertheless, CEA lacks specificity for rectal cancer because its levels are influenced by confounding factors such as smoking, alcohol consumption, and inflammation, thus limiting its clinical utility[14-16].
Magnetic resonance imaging (MRI), a non-invasive imaging modality, has emerged as a cornerstone in the diagnosis and staging of rectal cancer. Due to its superior soft-tissue resolution, MRI enables precise visualization of the rectal wall layers, tumor morphology, size, depth of invasion, and involvement of adjacent structures, thereby guiding accurate staging. For example, MRI distinguishes early stage (T1 or T2) from locally advanced (T3 or T4) tumors, identifies lymph nodes or distant metastases, and provides a basis for tailored treatment strategies. Patients with T1/T2 tumors, extramural invasion < 5 mm, and no nodal metastasis may undergo total mesorectal excision (TME) directly[17,18]. In contrast, patients with extramural invasion > 5 mm and 1-3 metastatic lymph nodes typically undergo short-course radiotherapy followed by TME, whereas patients with extramural invasion > 5 mm, positive circumferential resection margin (CRM), or ≥ 4 metastatic lymph nodes require long-course chemoradiotherapy before surgery. Additionally, MRI is indispensable for postoperative surveillance, enabling early detection of recurrence.
Despite the individual clinical utility of serum CEA levels and MRI in rectal cancer management, existing studies investigating their correlation are sparse and predominantly limited by small cohorts or inconsistent imaging protocols. Elucidating this relationship could refine the clinical interpretation of CEA, enhance diagnostic accuracy, and optimize therapeutic decision-making, ultimately improving patient outcomes and quality of life[19,20]. Using a larger sample size (n = 80) and standardized MRI acquisition techniques, the present study aimed to strengthen the supportive evidence in this under-researched area.
Data from 80 patients, who were diagnosed with primary rectal cancer at the authors’ hospital between July 2022 and August 2024, were included. Detailed demographic and clinical data (age, sex, tumor location, etc.) were recorded. Patients were stratified into subgroups according to their clinical characteristics and treatment protocols; for example: (1) T stage: T1-T2 vs T3-T4; (2) N stage: N0 vs N1-N2; and (3) CRM status: CRM-negative vs CRM-positive. This stratification facilitated an in-depth exploration of the correlations between the MRI features and serum CEA levels, thereby ensuring the accuracy and reliability of the findings.
Inclusion criteria: (1) Pathologically confirmed primary rectal cancer; (2) Availability of baseline MRI examinations performed before treatment with images meeting the quality standards for analysis; and (3) No history of antitumor therapy (surgery, chemotherapy, or radiotherapy) before MRI.
Exclusion criteria: (1) History of another malignancy; (2) Severe dysfunction of vital organs (heart, liver, and kidneys) contraindicating MRI; (3) MRI images with significant artifacts or poor quality that could impair analysis; and (4) Psychiatric disorders or cognitive impairment.
All patients underwent MRI using a Discovery MR750 scanner (GE Healthcare, Madison, WI, United States), which provides a high-field strength and resolution for detailed visualization of the rectal anatomy and surrounding tissues. Before imaging, patients fasted for 4-6 hours to minimize intestinal content, which could interfere with image quality.
T1-weighted imaging: Spin-echo (SE) sequence with the following parameters: (1) Repetition time (TR): 400-700 ms; (2) Echo time (TE): 8-15 ms; (3) Slice thickness: 3-5 mm; (4) Slice gap: 0.5-1 mm; (5) Field of view: 300-380 mm × 300-380 mm; and (6) Matrix: 256 × 256-320 × 320.
T2-weighted imaging: (1) Fast SE sequence, with TR 3000-5000 ms; (2) TE: 80-120 ms; and (3) Other parameters identical to those of T1-weighted imaging (T1WI).
Diffusion-weighted imaging: A single-shot echo-planar imaging sequence, with b-values of 0 and 1000 s/mm², TR of 3000-6000 ms, TE of 60-100 ms, and other parameters matching T1WI.
Contrast-enhanced MRI was performed when clinically indicated. A gadolinium-based contrast agent (e.g., gadopentetate dimeglumine) was administered intravenously at 0.1 mmol/kg, at an injection rate of 1.5-2.0 mL/second. Postcontrast scans were acquired during the arterial, venous, and delayed phases. Image analysis was performed independently by 2 experienced radiologists blinded to clinical data and serum CEA levels.
Tumor size was measured on T2-weighted imaging (T2WI) images at the largest tumor cross section, with the average of the longest and shortest diameters recorded.
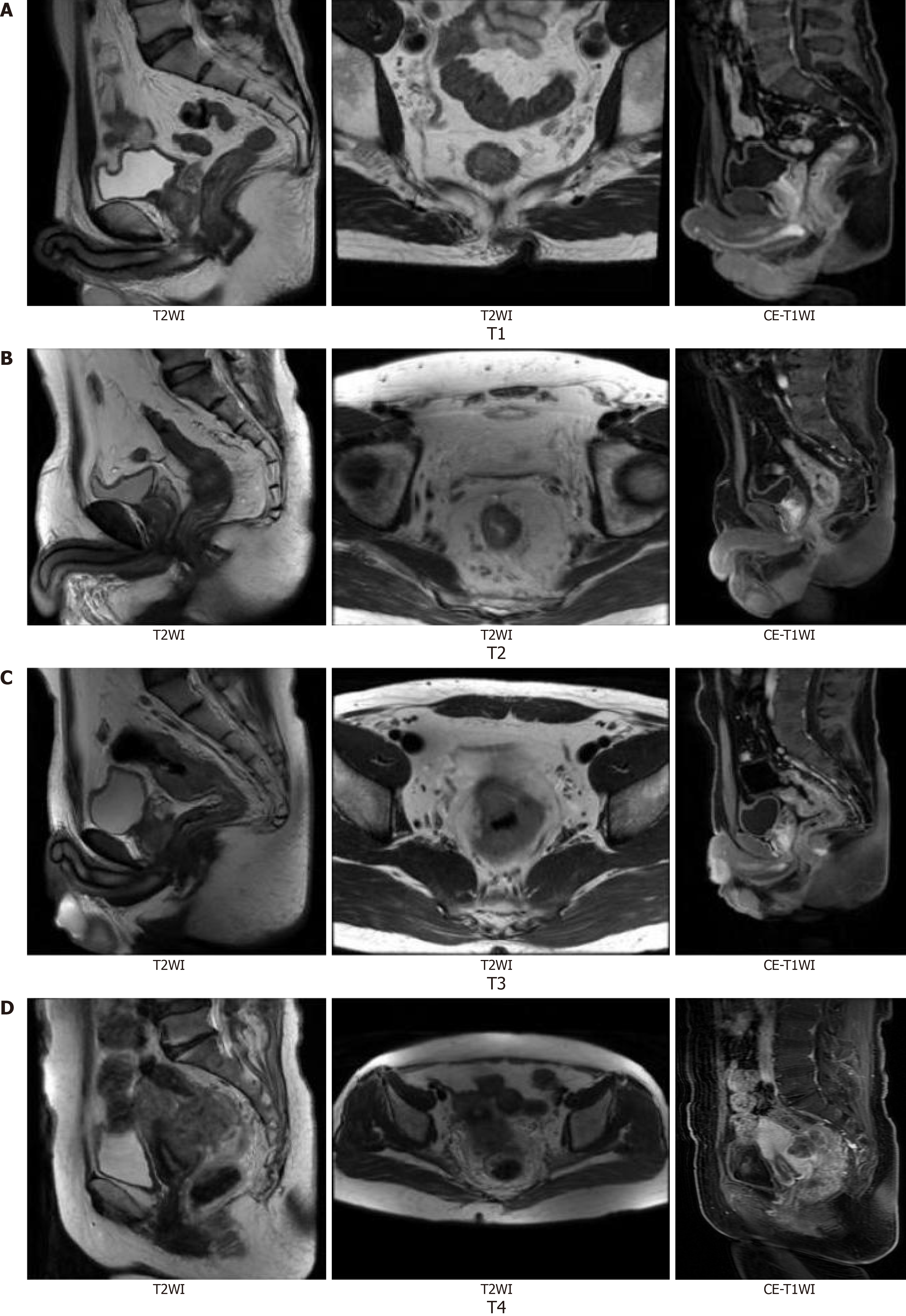
T stage: Determined as per the Union for International Cancer Control, 8th Edition TNM staging criteria: (1) T1: Tumor invades submucosa; (2) T2: Tumor invades muscularis propria; (3) T3: Tumor extends beyond the bowel wall; (4) T4: Tumor invades adjacent organs/structures; and (5) N stage: Lymph nodes were classified as metastatic if short-axis diameter ≥ 5 mm, irregular in shape, or heterogeneous in signal intensity (Figure 1).
CRM status: CRM-positive was defined as a tumor-to-margin distance < 1 mm according to the European Society for Medical Oncology guidelines. Extramural vascular invasion (EMVI) was defined as the presence of tumor signals within the perirectal vessels on T2WI, according to the National Comprehensive Cancer Network criteria. Tumor location was classified as the upper, middle, or lower rectum based on the anatomical segments. Discrepancies between radiologists were resolved through consensus discussion.
Fasting venous blood samples (5 mL) were collected from patients on the morning of their baseline MRI examination using vacuum tubes containing a separation gel. The samples were centrifuged at 3000 ×g for 10 minutes to isolate serum for CEA analysis. CEA levels were measured via electrochemiluminescence immunoassay (ECLIA) using a laboratory analyzer Cobas e601 (Roche Diagnostics, Rotkreuz, Switzerland) and Roche Diagnostics CEA assay kits. ECLIA yields high sensitivity, specificity, and rapid turnaround. All procedures were performed in strict accordance with manufacturer’s instructions. Quality control was performed every 24 hours using Roche PreciControl Tumor Markers 1 and 2 to ensure accuracy and reproducibility.
Data from 80 patients [44 male (55.0%), 36 female (45.0%)] diagnosed with primary rectal cancer were included in this study, with baseline characteristics summarized in Table 1. The age of the patients ranged from 42 years to 78 years, with a mean ± SD age of 62.3 ± 8.7 years. The body mass index (BMI) ranged from 18.5 kg/m² to 29.6 kg/m², with a mean BMI of 24.1 ± 3.4 kg/m². Regarding tumor location, 12 (15.0%) cases were classified as upper rectal cancer, 34 (42.5%) as middle rectal cancer, and 34 (42.5%) as lower rectal cancer. Statistical analysis revealed no significant differences in age, sex, BMI, or other baseline characteristics between the groups (all P > 0.05), indicating balanced intergroup comparability. These findings support the validity of the subsequent correlation analyses (Table 1).
| Characteristic | n | Percentage |
| Age (years) | 42-78 | |
| Average value (mean ± SD) | 62.3 ± 8.7 | |
| Gender | ||
| Male | 44 | 55.0 |
| Female | 36 | 45.0 |
| Body mass index (kg/m²) | 18.5-29.6 | |
| Average value (mean ± SD) | 24.1 ± 3.4 | |
| Tumor location | ||
| Upper rectum | 12 | 15.0 |
| Middle rectum | 34 | 42.5 |
| Lower rectum | 34 | 42.5 |
Results of the univariate analysis of MRI features and serum CEA levels are summarized in Table 2. Tumor size exhibited a significant positive correlation with serum CEA levels (Spearman’s correlation coefficient r = 0.456, P < 0.01), indicating that larger tumors were associated with higher serum CEA levels. Similarly, T stage was significantly positively correlated with serum CEA levels (r = 0.387, P < 0.01), suggesting a gradual increase in CEA levels with advancing T stage. A positive CRM was positively correlated with serum CEA level (r = 0.325, P < 0.05), implying that patients with CRM involvement had relatively elevated CEA levels. EMVI also exhibited a positive correlation with serum CEA levels
| Magnetic resonance imaging feature | n | Serum carcinoembryonic antigen level (ng/mL) (mean ± SD) | r value | P value |
| Tumor size (cm) | 0.456 | < 0.01 | ||
| ≤ 4 | 40 | 5.2 ± 1.8 | ||
| > 4 | 40 | 8.3 ± 2.5 | ||
| T-stage | 0.387 | < 0.01 | ||
| T1-T2 | 30 | 4.8 ± 1.6 | ||
| T3-T4 | 50 | 8.1 ± 2.9 | ||
| Circumferential resection margin | 0.325 | < 0.05 | ||
| Positive | 28 | 8.9 ± 3.3 | ||
| Negative | 52 | 5.2 ± 2.1 | ||
| Extramural vascular invasion | 0.298 | < 0.05 | ||
| Yes | 35 | 7.8 ± 2.7 | ||
| No | 45 | 5.3 ± 2.3 | ||
| Lymph node metastasis | 0.356 | < 0.01 | ||
| Yes | 40 | 8.5 ± 2.8 | ||
| No | 40 | 4.9 ± 1.9 |
Tumor size: Patients were stratified according to median tumor diameter (4 cm). The < 4 cm group exhibited significantly lower CEA levels than the > 4 cm group (P < 0.01).
T-stage: Mean CEA levels were lower in T1-T2 tumors (4.8 ± 1.6 ng/mL) and significantly elevated in T3-T4 tumors (8.1 ± 2.9 ng/mL, P < 0.01), indicating a positive correlation between CEA levels and tumor invasion depth.
CRM: CEA levels were significantly higher in the CRM-positive group (8.9 ± 3.3 ng/mL) compared with the CRM-negative group (5.2 ± 2.1 ng/mL, P < 0.05).
EMVI: Patients with EMVI demonstrated a 47% increase in mean CEA levels compared to those without EMVI (7.8 ± 2.7 ng/mL vs 5.3 ± 2.3 ng/mL).
Lymph node metastasis: The metastasis group exhibited a 73% elevation in CEA levels compared with the non-metastatic group (8.5 ± 2.8 ng/mL vs 4.9 ± 1.9 ng/mL, P < 0.01).
MRI features with statistical significance in the univariate analysis, tumor size, T-stage, CRM status, EMVI, and lymph node metastasis were included as independent variables in a multivariate logistic regression model. The results are summarized in Table 3. Tumor size [odds ratio (OR) = 2.563, 95%CI: 1.562-4.208, P < 0.01], T stage (OR = 1.875, 95%CI: 1.236-2.847, P < 0.01), and lymph node metastasis (OR = 1.684, 95%CI: 1.057-2.685, P < 0.05) were identified as independent risk factors that significantly influenced serum CEA levels. In contrast, CRM status (OR = 1.234, 95%CI: 0.856-1.782, P > 0.05) and EMVI (OR = 1.156, 95%CI: 0.789-1.697, P > 0.05) did not demonstrate independent effects on serum CEA levels in the multivariate analysis. The lack of significance of EMVI may reflect its close association with lymph node metastasis because tumor infiltration into the perirectal vessels often precedes lymphatic dissemination. This collinearity may attenuate the independent predictive value of elevated CEA levels. Nevertheless, EMVI remains a critical marker of advanced disease and systemic spread, consistent with its established role in risk stratification[20]. These results suggest that tumor size, T stage, and lymph node metastasis are critical MRI features that are closely associated with serum CEA levels in patients with primary rectal cancer, exhibiting a significant independent predictive value for evaluating serum CEA levels (Table 3). Tumor size, T-stage, and lymph node metastasis were identified as independent risk factors that were significantly associated with elevated serum CEA levels (all P < 0.05). CRM status (CRM status and EMVI) did not show statistically significant effects on serum CEA levels (P > 0.05).
| Independent variable | B | SE | Wald | Odds ratio | 95%CI | P value |
| Tumor size | 0.942 | 0.256 | 13.578 | 2.563 | 1.562-4.208 | < 0.01 |
| T-stage | 0.629 | 0.201 | 9.745 | 1.875 | 1.236-2.847 | < 0.01 |
| Circumferential resection margin status | 0.212 | 0.198 | 1.146 | 1.234 | 0.856-1.782 | > 0.05 |
| Extramural vascular invasion | 0.145 | 0.205 | 0.503 | 1.156 | 0.789-1.697 | > 0.05 |
| Lymph node metastasis | 0.521 | 0.239 | 4.736 | 1.684 | 1.057-2.685 | < 0.05 |
Model construction: A predictive model was constructed using tumor size, T stage, and lymph node metastasis as independent variables and serum CEA levels as the dependent variable. The model development process and performance metrics are listed in Table 4. The model demonstrated a sensitivity of 76.5% and specificity of 82.3%, indicating its ability to reliably identify patients with elevated serum CEA levels while accurately excluding those with low CEA levels. The area under the curve (AUC) was 0.856 (95%CI: 0.792-0.920), exceeding the threshold of 0.8, confirming the high predictive accuracy of the model for serum CEA levels in patients with primary rectal cancer. The Hosmer-Lemeshow test yielded a P value of 0.765 (P > 0.05), indicating good model calibration and reliability of the predicted outcomes. This predictive model serves as an effective clinical tool to assess serum CEA levels in patients diagnosed with primary rectal cancer, thereby enhancing the precision of treatment planning and prognostic evaluation (Table 4)
| Indicator | Value |
| Sensitivity (%) | 76.5 |
| Specificity (%) | 82.3 |
| Area under the curve | 0.856 |
| 95%CI | 0.782-0.930 |
| P value of Hosmer-Lemeshow test | 0.765 |
Stratified analysis of model performance: A further stratified analysis of the predictive model performance is presented in Table 5. Across subgroups stratified according to T stage and lymph node metastasis status, the model yielded an AUC > 0.7, indicating consistent predictive utility in all subgroups. Notably, in the subgroup with T3-T4 stage disease and lymph node metastasis, the AUC reached 0.912 (95%CI: 0.865-0.958), reflecting a high predictive accuracy for serum CEA levels in patients with advanced disease. In contrast, the subgroup with stage T1-T2 disease and no lymph node metastasis exhibited a relatively low but clinically meaningful AUC of 0.735 (95%CI: 0.642-0.828). This stratified analysis comprehensively demonstrates the robust performance of the model across heterogeneous patient populations, providing a reference for clinicians to apply the model based on individual patient profiles (Table 5).
| Subgroup | n | Area under the curve | 95%CI |
| Stage T1-T2 and no lymph node metastasis | 18 | 0.735 | 0.623-0.847 |
| Stage T1-T2 and with lymph node metastasis | 12 | 0.802 | 0.698-0.906 |
| Stage T3-T4 and no lymph node metastasis | 21 | 0.834 | 0.721-0.947 |
| Stage T3-T4 and with lymph node metastasis | 19 | 0.912 | 0.835-0.989 |
The present study comprehensively investigated the correlation between baseline MRI features and serum CEA levels in patients diagnosed with primary rectal cancer and revealed a significant association between these parameters. In univariate analysis, MRI characteristics, such as tumor size, T-stage, CRM status, EMVI, and lymph node metastasis, were all significantly correlated with serum CEA levels. Larger tumor size was associated with higher serum CEA levels, which is likely attributable to enhanced tumor cell proliferation and metabolic activity in larger lesions, leading to increased CEA secretion into the bloodstream. T stage, which reflects tumor invasion depth, demonstrated a progressive increase in serum CEA levels with advancing stage, suggesting that elevation of CEA levels parallels tumor aggressiveness. A positive CRM, indicative of tumor involvement at the surgical resection margin, was correlated with elevated CEA levels, potentially signaling greater local invasiveness and a higher risk for recurrence or metastasis. EMVI, a pathway for hematogenous tumor spread, has been linked to increased CEA levels, implying systemic dissemination of cancer cells via the circulatory system. Lymph node metastasis, a key prognostic marker, was associated with markedly higher serum CEA levels compared with non-metastatic cases, further validating the role of CEA in assessing metastatic progression[20,21].
Multivariate analysis identified tumor size, T stage, and lymph node metastasis as independent risk factors for elevated serum CEA levels. Tumor size directly reflects tumor burden, with larger tumors likely driving greater CEA production. An advanced T-stage signifies deeper tissue infiltration and higher malignant potential, potentially amplifying CEA expression. Lymph node metastasis, a critical indicator of tumor spread, triggers a significant increase in serum CEA levels, underscoring its utility in monitoring disease progression. Clinically, these findings highlight the importance of integrating tumor size, T-stage, and lymph node status to predict serum CEA levels, thereby informing personalized therapeutic strategies and prognostic evaluations[22,23].
The predictive model, constructed using tumor size, T stage, and lymph node metastasis as independent variables and serum CEA level as the dependent variable, demonstrated high clinical utility. The model achieved a sensitivity of 76.5%, a specificity of 82.3%, and an AUC of 0.856. The Hosmer-Lemeshow test (P = 0.765) confirmed good model calibration. This model provides clinicians with a robust tool for accurately evaluating serum CEA levels in patients diagnosed with primary rectal cancer. By integrating MRI features, physicians can predict serum CEA levels, assess disease severity, and optimize treatment strategies. For example, patients predicted to have elevated CEA levels may benefit from aggressive neoadjuvant chemoradiotherapy for downstaging tumors, thereby improving surgical outcomes and survival rates.
Despite its findings, this study had several limitations. The relatively small sample size may have limited the generalizability of the results. Future studies should expand the cohort to include patients from diverse geographical regions and ethnic backgrounds to enhance the reliability and external validity of the results.
Results of this study underscore the value of MRI-based risk stratification combined with serum CEA monitoring to guide the individualized management of rectal cancer, ultimately aiming to balance treatment efficacy with quality of life.
| 1. | Emile SH, Horesh N, Garoufalia Z, Gefen R, Dourado J, Wignakumar A, Wexner SD. Household income is independently associated with overall and cancer-specific survival after proctectomy for rectal cancer: A surveillance, epidemiology, and end results-based analysis. Am J Surg. 2025;242:116191. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Wale A, Brown G. ASO Author Reflections: Diagnostic Certainty in Characterizing Liver Lesions in Rectal Cancer: Abbreviated Liver MRI Versus CT. Ann Surg Oncol. 2025;32:2481-2482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Gan Y, Hu Q, Shen Q, Lin P, Qian Q, Zhuo M, Xue E, Chen Z. Comparison of Intratumoral and Peritumoral Deep Learning, Radiomics, and Fusion Models for Predicting KRAS Gene Mutations in Rectal Cancer Based on Endorectal Ultrasound Imaging. Ann Surg Oncol. 2025;32:3019-3030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 4. | Chuang JP, Tsai HL, Chen PJ, Huang CW, Su WC, Chang TK, Chen YC, Li CC, Yeh YS, Wang JY. Smoking and Elevated Preneoadjuvant Chemoradiotherapy Serum Carcinoembryonic Antigen Levels Are Associated With High Tumor Regression Grade and Poor Survival in Patients With Locally Advanced Rectal Cancer. Kaohsiung J Med Sci. 2025;41:e70008. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Tsukamoto R, Sugimoto K, Ii Y, Irie T, Kawaguchi M, Kobari A, Tsuchiya Y, Honjo K, Kawai M, Ishiyama S, Takahashi M, Sakamoto K. Prognostic Impact of the Postoperative Carcinoembryonic Antigen Level after Curative Resection of Locally Advanced Rectal Cancer. J Anus Rectum Colon. 2025;9:69-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Xie H, Wei L, Tang S, Gan J. Serum albumin-carcinoembryonic antigen ratio as an effective clinical tool for predicting recurrence and overall survival in patients with rectal cancer. Front Nutr. 2024;11:1521691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Fu S, Xia T, Li Z, Zhu J, Zeng Z, Li B, Xie S, Li W, Xie P. Baseline MRI-based radiomics improving the recurrence risk stratification in rectal cancer patients with negative carcinoembryonic antigen: A multicenter cohort study. Eur J Radiol. 2025;182:111839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Lv B, Li D, Li J, Shang K, Wu K, Jin E, Li X. Prediction of Synchronous Serum CEA Expression Status Based on Baseline MRI Features of Primary Rectal Cancer Lesions Pre-treatment: A Retrospective Study. Sci Rep. 2024;14:31469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Okumura T, Hotta K, Imai K, Ito S, Kishida Y, Takada K, Kawaguchi D, Mori Y, Tanaka Y, Tsushima T, Kawata N, Maeda Y, Yoshida M, Yamamoto Y, Minamide T, Ishiwatari H, Sato J, Matsubayashi H, Ono H. Efficacy of texture and color enhancement imaging for the visibility and diagnostic accuracy of non-polypoid colorectal lesions. DEN Open. 2025;5:e380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Yao Q, Yang WY. Evaluating organ preservation strategies versus radical surgery in T2N0 rectal cancer: survival outcomes and tumor size impact. Int J Colorectal Dis. 2025;40:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | McMahon RK, O'Cathail SM, Steele CW, Nair HS, Platt JJ, McMillan DC, Horgan PG, Roxburgh CS. Circulating Markers of Systemic Inflammation, Measured After Completion of Neoadjuvant Therapy, Associated With Response in Locally Advanced Rectal Cancer. Dis Colon Rectum. 2025;68:713-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Li QY, Yan XY, Guan Z, Sun RJ, Lu QY, Li XT, Zhang XY, Sun YS. A method of matching nodes between MRI and pathology with MRI-based 3D node map in rectal cancer. Abdom Radiol (NY). 2025;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Dou L, Cai A, Song S, Wang G, He S. A treatment option for rectal gastrointestinal stromal tumor: endoscopic submucosal dissection combined with endoscopic hand-suturing. Endoscopy. 2025;57:E167-E168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Wirth U, Schardey J, Scholz F, Niedermaier T, Germer CT, Kroesen AJ, Pantelis D, Reissfelder C, Rentsch M, Ritz JP, Schäfer N, Andrassy J, Werner J, Kühn F. Clinical Features in Patients With Early-Onset Colorectal Cancer: An Evaluation of Data From the StuDoQ Database. Dtsch Arztebl Int. 2025;122:235-239. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Qin J, Dong W, Zhao F, Liu T, Chen M, Zhang R, Zhao Y, Zhang C, Wang W. Prediction of metachronous liver metastasis in mid-low rectal cancer using quantitative perirectal fat content from high-resolution MRI. Magn Reson Imaging. 2025;118:110338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Lee GC. Surveillance and Management of Dysplasia and Malignancy in Inflammatory Bowel Disease. Surg Clin North Am. 2025;105:313-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Fallon EA, Awiwi MO, Bhutiani N, Helmink B, Scally CP, Mansfield P, Fournier K, Vikram R, Uppal A, White MG. Peritoneal Cancer Index Correlates with Radiographic Assessment of Colorectal Carcinomatosis. Ann Surg Oncol. 2025;32:2923-2931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Wale A, Harris H, Brown G. Diagnostic Certainty in Characterizing Liver Lesions in Rectal Cancer: Abbreviated Liver MRI versus CT. Ann Surg Oncol. 2025;32:2435-2445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Tang X, Zhuang Z, Jiang L, Zhu H, Wang D, Zhang L. A Preoperative CT-based Multiparameter Deep Learning and Radiomic Model with Extracellular Volume Parameter Images Can Predict the Tumor Budding Grade in Rectal Cancer Patients. Acad Radiol. 2025;32:4002-4012. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Gong X, Ye Z, Shen Y, Song B. Enhancing the role of MRI in rectal cancer: advances from staging to prognosis prediction. Eur Radiol. 2025;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 21. | Xu F, Hong J, Wu X. An Integrative Clinical and Intra- and Peritumoral MRI Radiomics Nomogram for the Preoperative Prediction of Lymphovascular Invasion in Rectal Cancer. Acad Radiol. 2025;32:3989-4001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Hu T, Rong Z, Cai C, Feng Y, Zhang Z, Cai G, Sun Y, Tong T. Impact of MRI risk assessment on the survival benefits of neoadjuvant chemoradiotherapy in patients with stage II-III rectal cancer: A retrospective cohort study. Eur J Radiol. 2025;184:111954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Xu J, Zhong M, Peng W, Wu M, Wang R, Tan S. Correlation study of functional magnetic resonance index and clinicopathological features of rectal cancer. Abdom Radiol (NY). 2024;49:2368-2386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |