Published online Jun 15, 2025. doi: 10.4251/wjgo.v17.i6.106645
Revised: April 11, 2025
Accepted: May 21, 2025
Published online: June 15, 2025
Processing time: 102 Days and 6.8 Hours
Since its introduction in 1991, laparoscopic right colectomy has been the standard surgical treatment for benign and malignant right colon diseases. Extracorporeal anastomosis (ECA) is the most commonly used anastomotic technique. However, intracorporeal anastomosis (ICA) has emerged as a promising alternative because of its potential advantages. Recently, Wu et al provided compelling evidence supporting superiority of ICA over ECA, demonstrating reduced blood loss, smaller incisions, and faster postoperative recovery without increased complications. Despite these benefits, ICA presents certain challenges such as longer operative times and technical difficulties. However, advances in minimally in
Core Tip: Intracorporeal anastomosis (ICA) in laparoscopic right colectomy offers significant advantages over extracorporeal anastomosis, including a reduced incision size, faster postoperative recovery, and lower risk of complications. The study by Wu et al reinforced these benefits, demonstrating improved short-term outcomes without an increase in complications. Despite challenges, such as a longer learning curve, the integration of robotic surgery may enhance the feasibility of ICA. Future research, including randomized controlled trials, is necessary to establish ICA as a standard technique in minimally invasive colorectal surgery.
- Citation: Bae SU. Elevating surgical standards: The role of intraperitoneal isoperistaltic side-to-side anastomosis in colon cancer surgery. World J Gastrointest Oncol 2025; 17(6): 106645
- URL: https://www.wjgnet.com/1948-5204/full/v17/i6/106645.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i6.106645
Since its inception in 1991, laparoscopic right colectomy (LRC) has emerged as the accepted surgical procedure for both benign and malignant right colon disorders. It is generally accepted to be feasible in terms of oncological radicalism and positive short-term clinical results[1-3]. We read with great interest the article by Wu et al[4] titled, "Is intraperitoneal isoperistaltic side-to-side anastomosis a safe surgical procedure in radical colon cancer surgery", published in the World Journal of Gastrointestinal Oncology. The authors presented an insightful analysis comparing intracorporeal anastomosis (ICA) and extracorporeal anastomosis (ECA) in laparoscopic right hemicolectomy, providing valuable evidence on the advantages of ICA in minimally invasive colorectal surgery. Given the increasing adoption of laparoscopic and robotic techniques, the role of ICA has garnered significant attention, and its findings further reinforce the feasibility and benefits of this approach.
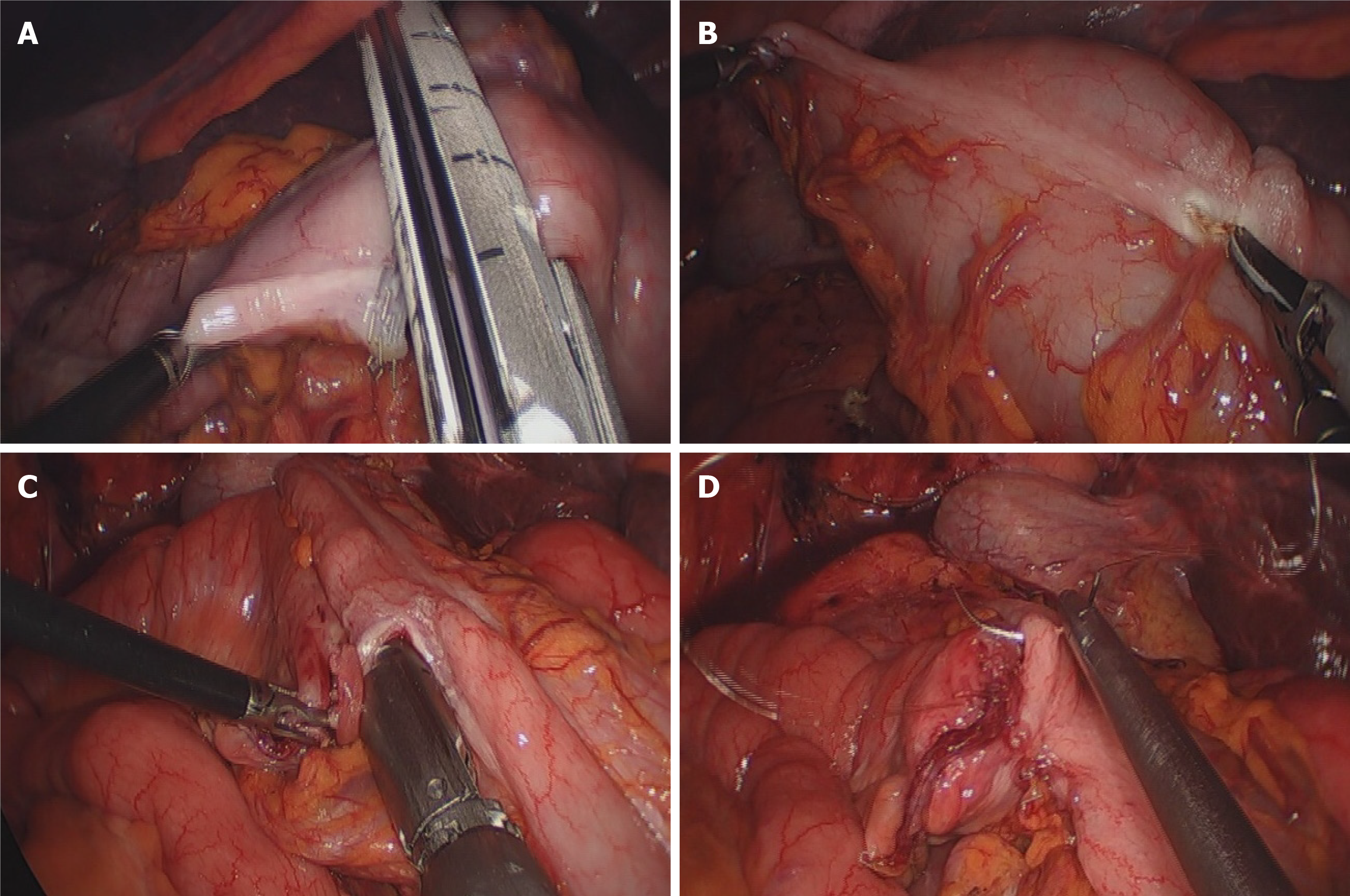
The ECA is the most frequently used laparoscopic anastomotic technique for the treatment of colonic malignancies. ICA has emerged as a promising alternative to ECA for right hemicolectomy because of its potential to improve postoperative recovery and minimize surgical trauma (Figure 1)[5,6]. Unlike ECA, which requires bowel externalization through an extended incision, ICA allows for complete intra-abdominal anastomosis, thus reducing unnecessary bowel traction and mesenteric tension. This technique has been associated with several advantages, including reduced incision size, lower rates of postoperative pain, faster return of bowel function, and decreased risk of incisional hernias[1,7,8]. Studies have demonstrated that ICA is associated with a shorter time to first flatus and defecation than ECA, potentially due to reduced bowel manipulation and better preservation of the mesenteric vasculature. Our previous study showed that ICA could reduce the incidence of postoperative ileus after LRC compared to ECA after LRC[7].
Wu et al’s study provides compelling evidence supporting these advantages[4]. Their propensity score-matched analysis demonstrated that ICA resulted in significantly reduced blood loss, smaller incision size, and earlier postoperative gastrointestinal recovery than ECA. Notably, their findings showed no significant increase in postoperative complications, reinforcing the safety profile of ICA. Stratified analysis based on tumor location provided additional insights, particularly highlighting the benefits of ICA in right-sided colon cancer. The rigorous methodology of the study, including the careful selection of cases and the use of statistical matching to minimize bias, adds credibility to the conclusions.
Although ICA offers multiple benefits, certain challenges remain. A primary concern is the longer operative time associated with this technique. Some studies suggested that the ICA group experienced a longer operative time with technical difficulties, while others reported a reduced total operative time when compared to the ECA group[7,9-11]. Laparoscopic suturing and intracorporeal stapling require advanced technical proficiency, and surgeons must follow a steep learning curve to achieve ICA proficiency. This is particularly relevant in centers where minimally invasive colorectal surgery is still evolving. Another consideration is the potential risk of intra-abdominal infection, although evidence suggests that meticulous surgical techniques and appropriate intraoperative sterilization can mitigate this risk. This can lead to the formation of a postoperative intra-abdominal abscess and infection at the surgical site, both of which are associated with postoperative ileus. Mechanical gastrointestinal preparation and prophylactic antibiotics[12] play an important role in the prevention of postoperative infectious complications, as reported by Scarborough et al[13]. We conducted mechanical bowel preparation one day prior to surgery and positioned the gauze under the anastomotic site to prevent spillage of bowel content into the abdominal cavity during the anastomotic procedure.
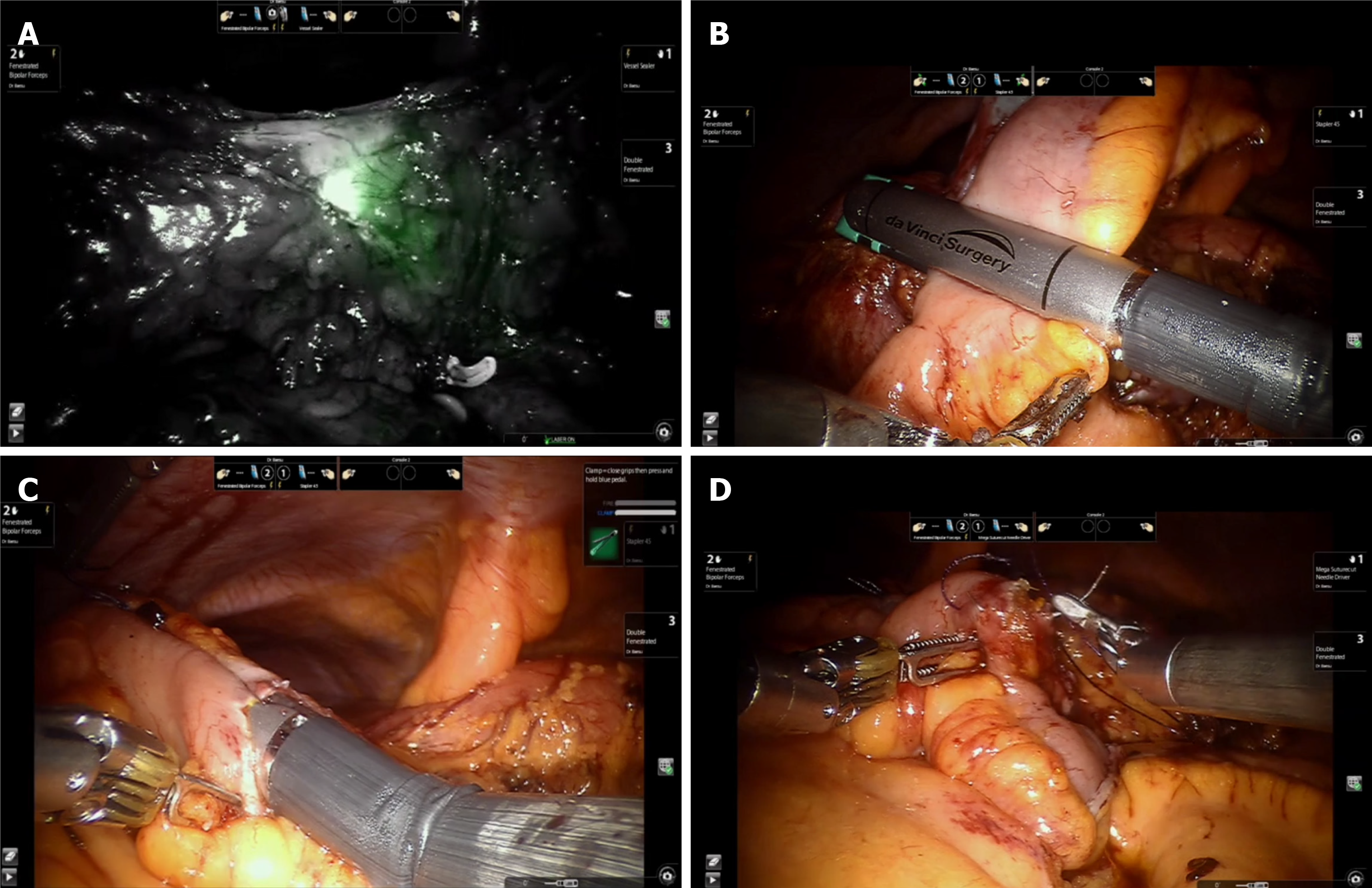
A surgical robotic system has been recently introduced to the colorectal field, and this system was devised to address the inherent limitations of laparoscopic surgery. Although the cost and role of robotics in colon surgery are controversial, surgeons prefer ICA to robotic colectomy[12,14]. Once the common enterotomy opening (where the linear stapler was inserted) was closed with a continuous-flow suture using wristed instruments, the robotic approach for ICA could be appreciated (Figure 2). This benefit is particularly valuable when sawn anastomosis is preferred. Furthermore, the wristed robotic stapler facilitates intestinal transection with enhanced ease and ergonomics.
This study by Wu et al[4] contributes significantly to the growing body of literature advocating the use of ICA in right hemicolectomy. Their findings align with those of previous research, demonstrating superior short-term outcomes with ICA and further validating its role in modern colorectal surgery. However, to establish ICA as the standard of care, multicenter randomized controlled trials should be conducted to confirm its oncological safety, standardized training programs should be developed to accelerate the learning curve, and integration of robotic platforms needs to be explored to enhance surgical precision.
ICA represents an important advancement in minimally invasive right hemicolectomies. Wu et al’s findings have strengthened the evidence supporting this technique and underscored its potential for improving patient outcomes[4]. With continued research and refinement of surgical techniques, ICA has the potential to become the preferred approach for anastomosis in laparoscopic and robotic colorectal surgeries.
| 1. | Arezzo A, Passera R, Ferri V, Gonella F, Cirocchi R, Morino M. Laparoscopic right colectomy reduces short-term mortality and morbidity. Results of a systematic review and meta-analysis. Int J Colorectal Dis. 2015;30:1457-1472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Yang IJ, Seo M, Oh HK, Lee J, Suh JW, Kim DW, Kang SB. Surgical Outcomes of Single-Port Laparoscopic Surgery Compared With Conventional Laparoscopic Surgery for Appendiceal Mucinous Neoplasm. Ann Coloproctol. 2021;37:239-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Schlinkert RT. Laparoscopic-assisted right hemicolectomy. Dis Colon Rectum. 1991;34:1030-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 130] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Wu B, Zhu JT, Lin HX, Dai YH, Lin TS, Huang AL, Chen YN, Li YW, Wang HB, Chen YF, Chen DH, Yu HD, You J, Hong QQ. Is intraperitoneal isoperistaltic side-to-side anastomosis a safe surgical procedure in radical colon cancer surgery. World J Gastrointest Oncol. 2025;17:99124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Reference Citation Analysis (0)] |
| 5. | Frigault J, Avoine S, Drolet S, Letarte F, Bouchard A, Gagné JP, Thibault C, Grégoire RC, Bouthillette NJ, Gosselin M, Bouchard P. Intracorporeal versus extracorporeal anastomosis in laparoscopic right hemicolectomy: a retrospective cohort study of anastomotic complications. Ann Coloproctol. 2023;39:147-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Lee N, Lee SY, Kim CH, Kwak HD, Ju JK, Kim HR. The Relationship Between High-Output Stomas, Postoperative Ileus, and Readmission After Rectal Cancer Surgery With Diverting Ileostomy. Ann Coloproctol. 2021;37:44-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Bollo J, Turrado V, Rabal A, Carrillo E, Gich I, Martinez MC, Hernandez P, Targarona E. Randomized clinical trial of intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy (IEA trial). Br J Surg. 2020;107:364-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 108] [Article Influence: 18.0] [Reference Citation Analysis (1)] |
| 8. | Carnuccio P, Jimeno J, Parés D. Laparoscopic right colectomy: a systematic review and meta-analysis of observational studies comparing two types of anastomosis. Tech Coloproctol. 2014;18:5-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Shapiro R, Keler U, Segev L, Sarna S, Hatib K, Hazzan D. Laparoscopic right hemicolectomy with intracorporeal anastomosis: short- and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc. 2016;30:3823-3829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 106] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 10. | Fabozzi M, Allieta R, Brachet Contul R, Grivon M, Millo P, Lale-Murix E, Nardi M Jr. Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc. 2010;24:2085-2091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Martinek L, You K, Giuratrabocchetta S, Gachabayov M, Lee K, Bergamaschi R. Does laparoscopic intracorporeal ileocolic anastomosis decreases surgical site infection rate? A propensity score-matched cohort study. Int J Colorectal Dis. 2018;33:291-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Mori S, Kita Y, Baba K, Tanabe K, Wada M, Yoshino S, Nishida N, Iino S, Setoyama T, Maemura K, Ohtsuka T. A sutureless overlapped anastomosis technique using linear staplers with reinforced bioabsorbable material in robotic right colectomy with intracorporeal anastomosis. Colorectal Dis. 2024;26:754-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 13. | Scarborough JE, Mantyh CR, Sun Z, Migaly J. Combined Mechanical and Oral Antibiotic Bowel Preparation Reduces Incisional Surgical Site Infection and Anastomotic Leak Rates After Elective Colorectal Resection: An Analysis of Colectomy-Targeted ACS NSQIP. Ann Surg. 2015;262:331-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 227] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 14. | Cleary RK, Silviera M, Reidy TJ, McCormick J, Johnson CS, Sylla P, Cannon J, Lujan H, Kassir A, Landmann R, Gaertner W, Lee E, Bastawrous A, Bardakcioglu O, Pandey S, Attaluri V, Bernstein M, Obias V, Franklin ME Jr, Pigazzi A. Intracorporeal and extracorporeal anastomosis for robotic-assisted and laparoscopic right colectomy: short-term outcomes of a multi-center prospective trial. Surg Endosc. 2022;36:4349-4358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |