Published online May 15, 2025. doi: 10.4251/wjgo.v17.i5.104011
Revised: February 23, 2025
Accepted: March 25, 2025
Published online: May 15, 2025
Processing time: 155 Days and 23.5 Hours
Low-grade appendiceal mucinous neoplasms (LAMNs) are a class of histologically well-differentiated adenomas that can proliferate outside the appendix in the form of malignant tumours, resulting in the accumulation of external appen
A 68-year-old man underwent a routine physical examination at our hospital on May 17, 2022. The patient had no symptoms of abdominal pain, bloating, or weight loss, and his tumour marker levels were normal. The faecal occult blood test was negative, and no abnormalities were identified on physical examination. Colonoscopy revealed a submucosal protrusion at the appendiceal orifice. During endoscopic ultrasound, uneven echoes were observed in the appendix cavity. A contrast-enhanced computed tomography scan of the abdomen revealed a nodular thickening at the base of the appendix, with a diameter of approximately 1 cm. When all the examination results were considered, we suspected the lesion to be an appendiceal mucinous tumour. Laparoscopic surgery was performed using the double purse-string suture method. Postoperative pathology suggested a low-grade mucinous cystadenoma of the appendix with no involvement of the margins. A repeat colonoscopy 18 months after surgery revealed no significant abnormality at the appendiceal orifice. A contrast-enhanced computed tomography scan of the abdomen suggested only postoperative changes.
This study describes a case of LAMN that was treated by resecting the mass at the appendiceal orifice via the double purse-string suture technique and provides new insights on the diagnosis and treatment of LAMNs.
Core Tip: Low-grade appendiceal mucinous neoplasms are a class of histologically well-differentiated adenomas. For low-grade appendiceal mucinous neoplasms with mass formation at the appendiceal orifice, if no metastatic lesion is indicated by imaging, the appendix and the mass at the appendiceal orifice should be completely resected. Our technique mainly targeted a mass approximately 1 cm from the opening of the appendix. We made the first pouch 1 cm from the root of the appendix, thus ensuring the anatomical integrity of the ileocecal valve. If conventional cutting closure is used, the anatomy of the ileocecal flap may be destroyed.
- Citation: Liu D, Xing YL, Chen D. Low-grade appendiceal mucinous neoplasm at appendiceal orifice treated via appendectomy with double purse-string suture method: A case report. World J Gastrointest Oncol 2025; 17(5): 104011
- URL: https://www.wjgnet.com/1948-5204/full/v17/i5/104011.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i5.104011
Compared with other gastrointestinal tract tumours, appendiceal neoplasms are rare, but their incidence is increasing[1]. The choice of treatment for low-grade appendiceal mucinous neoplasms (LAMNs) in the absence of appendiceal perforation and abdominal metastatic lesions is to ensure that the surgery can completely remove the appendix and the mass. In patients with LAMNs presenting as appendiceal orifice masses, a simple appendectomy does not ensure complete removal of the mass and may even result in medically induced abdominal dissemination. In patients with an appendiceal orifice mass of 1 cm or less, a double purse-string suture can be used to ensure complete resection.
The patient has no body uncomfortable, requested a colonoscopy.
The patient had no symptoms of abdominal pain, bloating, or weight loss.
The patient denied a history of hypertension, diabetes, hepatitis, tuberculosis, and trauma.
The patient had no personal or family history of tumours.
Physical examination was negative.
The tumour markers of the patient were normal. Faecal occult blood test was negative.
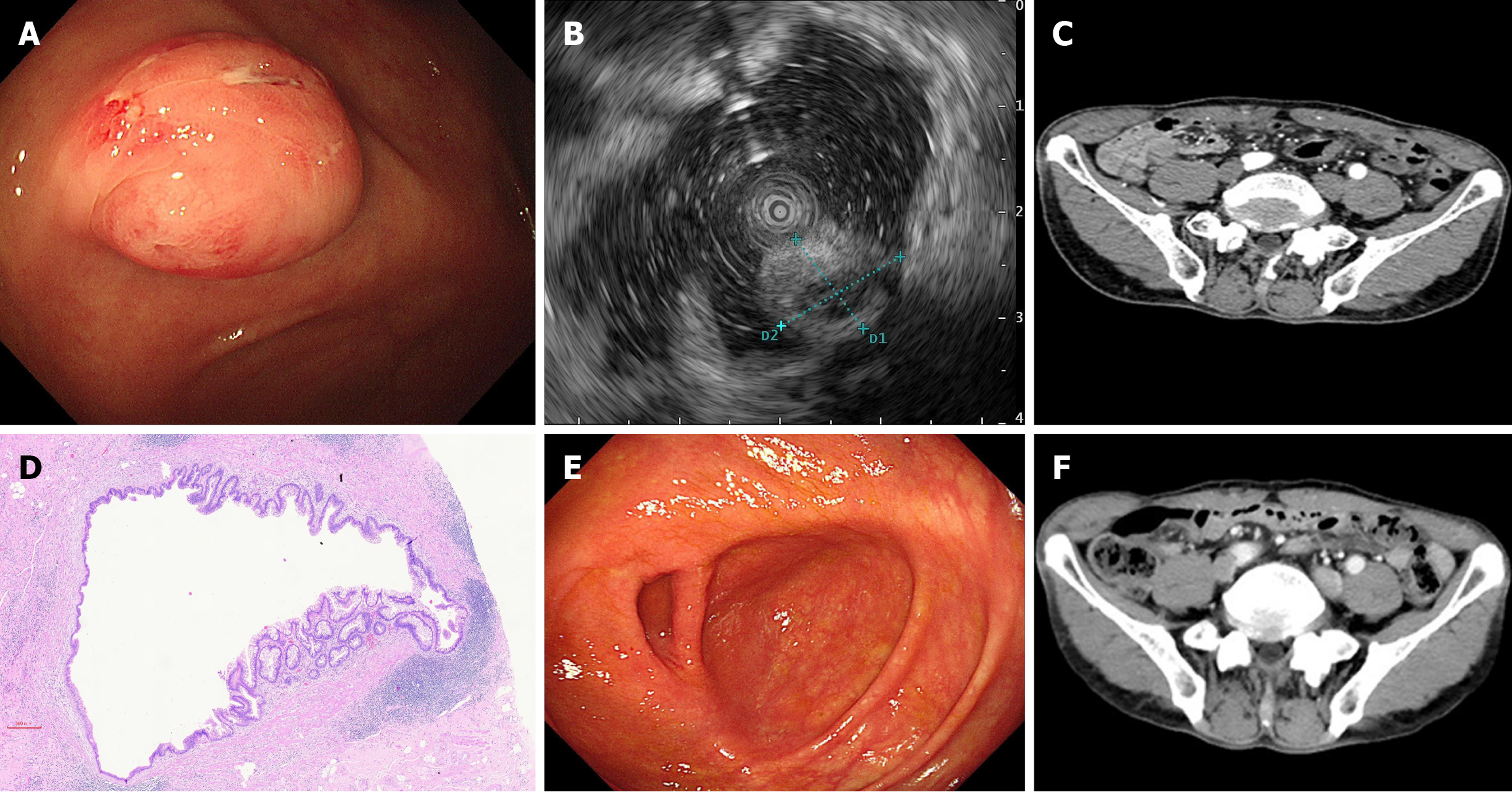
Colonoscopy revealed a submucosal protrusion at the opening of the appendix (Figure 1A). During endoscopic ultrasound, uneven echoes were observed in the appendix cavity (Figure 1B). A contrast-enhanced computed tomography (CT) scan of the abdomen revealed a nodular thickening at the base of the appendix, with a diameter of approximately 1 cm (Figure 1C).
Postoperative pathology revealed a low-grade mucinous cystadenoma of the appendix with no involvement of the margins (Figure 1D).
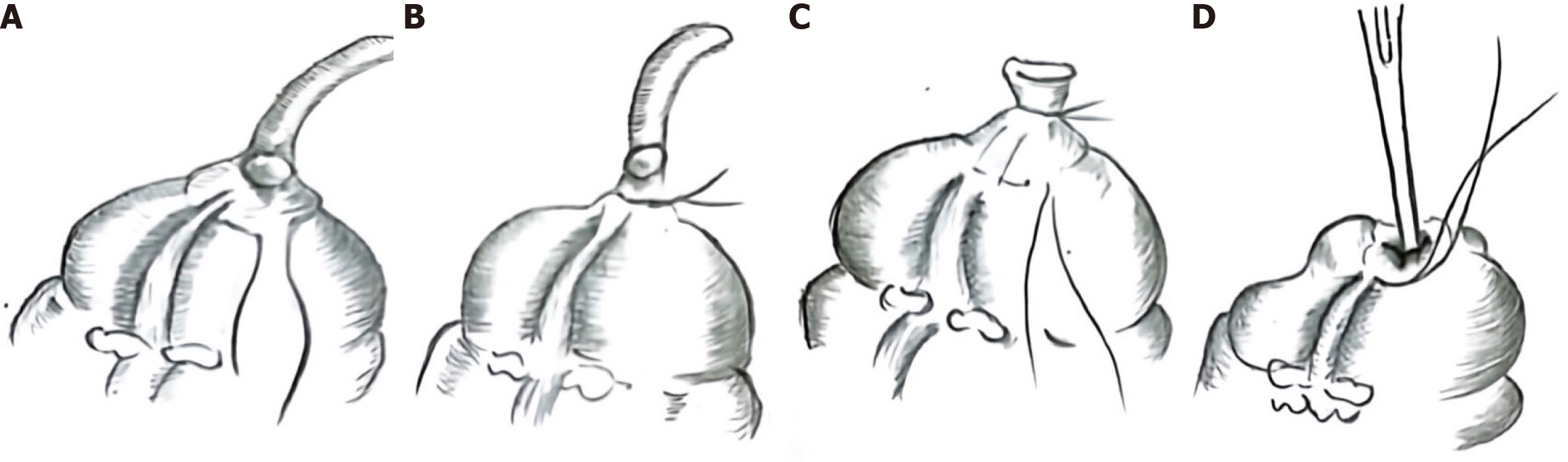
Before surgery, we communicated with the patient’s family regarding the surgical methods, including the double purse-bag method and the double purse-bag method. Due to the cost of surgery, the patient’s family chose the double purse-bag method. Laparoscopic surgery was performed on May 21, 2022. The patient received bowel preparation prior to the planned surgery. Absorbable surgical sutures, model 3-0, were used throughout surgery. During the operation, we did not find any surface mucin or mucin in the right iliac fossa or Morrison’s pouch. The double purse-string suture technique was performed by creating a purse-string suture approximately 1.0 cm below the swelling, at the appendiceal orifice. The incision was made 0.5 cm from the ligature line, and the appendix and swelling at the orifice were completely excised (Figure 2A and B), and a second purse-string suture was performed 1.0 cm from the ligature line, with the remaining end embedded and sutured into the purse (Figure 2C and D).
The patient recovered well after surgery. A repeat colonoscopy 18 months after surgery revealed no significant abnormality at the appendiceal orifice (Figure 1E). A contrast-enhanced CT scan of the abdomen suggested only postoperative changes (Figure 1F).
The World Health Organization classifies the majority of non-invasive tumours of epithelial origin as LAMNs, which are essentially a histologically well-differentiated type of adenoma. However, they can proliferate outside the appendix in a manner resembling the growth of malignant tumours, leading to the accumulation of mucus outside the appendix. In contrast, high-grade appendiceal mucinous neoplasms present a greater degree of cellular atypia than LAMNs, indicating their more aggressive nature[2,3]. Appendiceal neoplasms can cause appendix perforation and abdominal dissemination. When peritoneal dissemination produces large amounts of mucus, it is defined as pseudomyxoma peritonei. Surgical treatment can be used for patients with low-grade or high-grade appendix neoplasms and peritoneal metastasis. In the absence of perforation of the appendix or involvement of the peritoneum, it is important to avoid perforation of the appendix and tumour implantation during the surgical process and to maintain the integrity of the resected tumour.
Most studies have shown that LAMNs that are confined to the appendix, without perforation or peritoneal metastasis, can be cured with a simple appendectomy, which has a low recurrence rate[4]. For LAMNs with mass formation at the appendiceal orifice, if no metastatic lesion is indicated by imaging, the appendix and the mass at the appendiceal orifice should be completely resected. Anatomically, the ileocecal valve is located 2.0-3.0 cm from the opening of the appendix, and our technique mainly targeted a mass approximately 1 cm from the opening of the appendix. We made the first pouch 1 cm from the root of the appendix, thus ensuring the anatomical integrity of the ileocecal valve. If a conventional cutting closure is used, the anatomy of the ileocecal flap may be destroyed. If only the appendix is resected, there is a high probability of positive resection margins. For patients with positive resection margins, some guidelines currently recommend additional procedures, such as a typhlectomy, ileocecal resection or right hemicolectomy[5,6].
In this case, the patient presented with a mass at the orifice of the appendix measuring approximately 1 cm. We opted for the double purse-string suture technique and successfully removed the appendix and the mass at the orifice of the appendix completely. Therefore, the double purse-string suture technique may be an effective and feasible surgical approach for LAMNs. The patient will be followed up for 10 years with annual abdominal/pelvic CT scans and tumour markers including carcinoembryonic antigen and cancer antigens 125 and 19-9. CA199 is a tumour marker that can be used to monitor tumour progression and recurrence.
The authors sincerely thank the participant for his willingness to participate in this study.
| 1. | Marmor S, Portschy PR, Tuttle TM, Virnig BA. The rise in appendiceal cancer incidence: 2000-2009. J Gastrointest Surg. 2015;19:743-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 129] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 2. | Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, Washington KM, Carneiro F, Cree IA; WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76:182-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2554] [Cited by in RCA: 2440] [Article Influence: 488.0] [Reference Citation Analysis (3)] |
| 3. | Carr NJ, Cecil TD, Mohamed F, Sobin LH, Sugarbaker PH, González-Moreno S, Taflampas P, Chapman S, Moran BJ; Peritoneal Surface Oncology Group International. A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia: The Results of the Peritoneal Surface Oncology Group International (PSOGI) Modified Delphi Process. Am J Surg Pathol. 2016;40:14-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 515] [Article Influence: 57.2] [Reference Citation Analysis (0)] |
| 4. | Polydorides AD, Wen X. Clinicopathologic parameters and outcomes of mucinous neoplasms confined to the appendix: a benign entity with excellent prognosis. Mod Pathol. 2022;35:1732-1739. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Gupta AR, Brajcich BC, Yang AD, Bentrem DJ, Merkow RP. Necessity of posttreatment surveillance for low-grade appendiceal mucinous neoplasms. J Surg Oncol. 2021;124:1115-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Chicago Consensus Working Group. The Chicago Consensus on peritoneal surface malignancies: Management of appendiceal neoplasms. Cancer. 2020;126:2525-2533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |