Published online Mar 15, 2024. doi: 10.4251/wjgo.v16.i3.598
Peer-review started: October 21, 2023
First decision: December 6, 2023
Revised: December 6, 2023
Accepted: January 16, 2024
Article in press: January 16, 2024
Published online: March 15, 2024
Processing time: 143 Days and 3.2 Hours
Colorectal carcinoma is common, particularly on the left side. In 20% of patients, obstruction and ileus may be the first clinical manifestations of a carcinoma that has advanced (stage II, III or even IV). Diagnosis is based on clinical presentation, plain abdominal radiogram, computed tomography (CT), CT colonography and positron emission tomography/CT. The best management strategy in terms of short-term operative or interventional and long-term oncological outcomes re
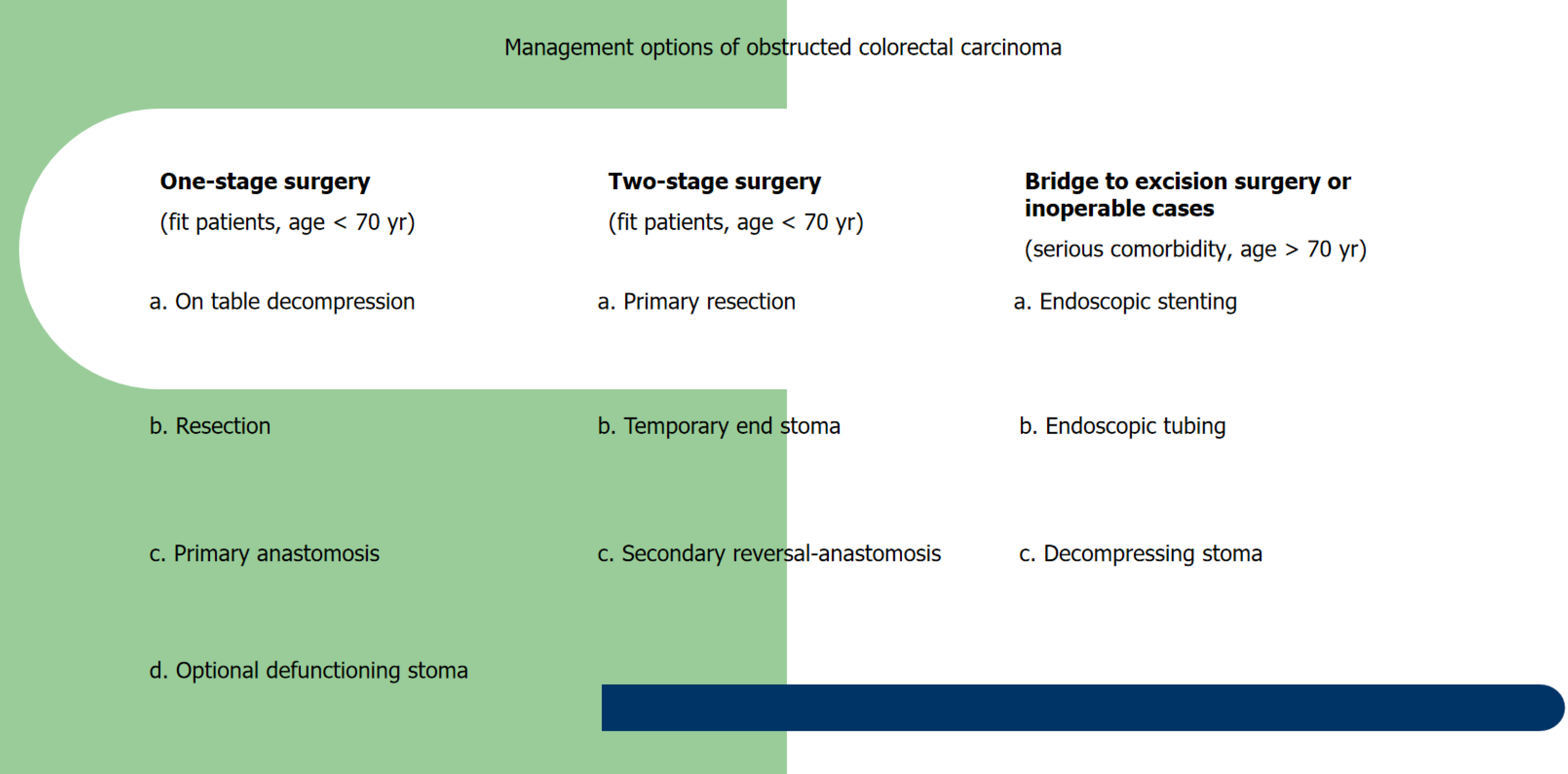
Core Tip: Acute obstruction is common in patients with more advanced colorectal carcinoma and may be the first manifestation mainly of left-sided obstruction and in elderly individuals. Emergency decompression is mandatory. Emergency surgical resection and primary anastomosis accompanied or not accompanied by proximal defunctioning stoma must be the first treatment choice for fit patients under 70 years. Hartmann’s two-stage procedure, although more preferable, must be the second alternative choice. Emergency endoscopic self-expendable metal stents must be preferred in unfit patients as a bridge to surgery and for palliative treatment in all inoperable cases. However, these basic management principles constitute a general direction. Decision-making is important and should be individualized.
- Citation: Pavlidis ET, Galanis IN, Pavlidis TE. Management of obstructed colorectal carcinoma in an emergency setting: An update. World J Gastrointest Oncol 2024; 16(3): 598-613
- URL: https://www.wjgnet.com/1948-5204/full/v16/i3/598.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v16.i3.598
Colorectal carcinoma is common, with its incidence increasing in young adults, and left-sided obstruction being the most common. It is the third most common carcinoma, after lung, and breast or prostate carcinoma and the second leading cause of cancer-related deaths, after lung carcinoma, in the United States and Western Europe, causing more than 50000 deaths annually in the United States[1-3]. Early detection and proper management improves survival and avoids complications (mainly obstruction, perforation, bleeding, and fistula)[4-8].
In 20%-30% of patients, mainly geriatrics, obstruction and ileus may be the first clinical manifestations of carcinoma that has advanced (stage II, III, or even IV)[2,9-12]. It is a potentially fatal condition that requires emergency intestinal decompression[3,13], and various models that predict the risk of mortality have been developed[14]. On the other hand, obstruction is the most common cause (75%-80%) of presentation to the emergency department among patients with colorectal carcinoma[15]. Younger age (under 50 years), males, and those with ascending colon obstruction have a greater possibility of presenting to the emergency department for care[3,8]. Subsequently, colorectal cancer screening is necessary to prevent obstruction. Screening is recommended, particularly for those with predisposing factors such as a family history of colorectal cancer or sleep apnea[2].
Strategies for the emergency management of left-sided obstruction in patients with colorectal cancer have been des
The growth pattern of colorectal carcinoma has been estimated. The median doubling time was 211 d, and the median rate of increase in tumor volume was 34.1% per 62 d[21].
The best management strategy in terms of short-term operative or interventional and long-term oncological outcomes remains unknown[16,22,23]. Early decompression is crucial because it prevents further bowel distention, ischemia and perforation, leading to fecal peritonitis and septic shock[23,24].
For left-sided obstruction, the first choice should be either emergency surgery or endoscopic decompression by self-expendable metal stent placement[10,22,25-27] or rectal tubes[19,28-31] as a bridge to surgery. However, there have been conflicting aspects. Stenting is not considered to be the gold standard. It may be related to possible perforation that causes septic subsequences leading to severe sepsis and septic shock. In addition, micro-perforation may promote cancer cell diffuse dissemination and distant metastasis. For rectal carcinoma, stenting is associated with technical difficulties and more stent migration[17,32].
The operative plan should be either one-stage or two-stage resection or, rarely, three-stage resection. One-stage resec
Operative management of such emergency cases, regardless of preoperative multimorbidity or not, is related to higher risks of mortality and morbidity than nonoperative interventional management[35]. It is well known that both diabetes mellitus and liver cirrhosis increase the risks of postoperative morbidity and mortality, especially in patients treated with colorectal surgery and in those requiring emergency treatment. Thus, such morbidities should be considered when se
A model was recently constructed that could accurately predict the risk of 30-day mortality after emergency operation for acute abdomen, including colorectal obstruction. It is based on a scoring system including 13 preoperative factors and may be valuable in deciding to perform an emergency operation, considering its kind, duration, and intensity[37].
Choosing the best management strategy can be challenging, and the choice should be evaluated under careful consideration of the patient’s physical status and the condition caused by the present disease, taking into account that for co
One-stage resection with primary anastomosis is more convenient but has increased risks of anastomotic leakage and morbidity[24]. Subtotal or total resection is a less common alternative[17].
Two-stage resection (Hartmann’s procedure) is safer and the most widely used procedure worldwide despite tempo
Damage control surgery in high-risk frail patients has been less frequently performed since it can be successfully sub
The role of minimally invasive surgery (laparoscopic or robotic) is still a subject of debate. Initial emergency laparoscopic management has been performed in approximately 20% of cases[41]; after initial stenting as a bridge to surgery, elective laparoscopic management has been performed in 32% of cases[24]. However, although emergency laparoscopic-assisted management is advantageous to some extent, it requires much expertise due to inherent difficulties in dissecting the distended colon and the risks of rupture and subsequent septic complications[41].
The decompressing stent as a bridge to elective surgery more substantially reduces the risks of morbidity and mortality than emergency surgery for decompression and has equivalent medium-term overall and disease-free survival rates[42]. Its combination with neoadjuvant chemotherapy or radiation for rectal cancer may have a positive effect on oncological outcomes[43].
Genetic studies may be needed mainly to prevent and, less commonly, diagnose colorectal carcinoma in cases of ano
This narrative review evaluates the current knowledge on severe obstruction in patients with colorectal carcinoma, emphasizing proper diagnosis and emergency management. This study was based on a large body of literature published in PubMed until September 2023, focusing particularly on full-text papers published only in the English language over the last five years.
Large bowel obstruction may be predominantly located on the left side (65%) but also the right side (35%)[45], as the boundary is considered to be the splenic flexure. They have the same clinical manifestation of obstructive ileus but some
Diagnosis is based on clinical examination and imaging. The onset is characterized by suspension of gas and feces, abdominal distension, deep pain or fullness, and nausea or possible vomiting. Vomiting is more apparent and earlier on the right side, while the distention is more obvious on the left side[15].
Plain abdominal radiogram shows marked colon dilation with possible small bowel dilation and air-fluid levels[46].
Computed tomography (CT) is needed to confirm tumor existence and its precise location. CT is the first choice ima
Colonoscopy can assess the entire colon and confirm the presence of a tumor in cases requiring differentiation from pseudo-obstruction (Ogilvie’s syndrome)[2,12,47-49].
This need for complete colon evaluation in patients with left-sided obstruction is mandatory because it may reveal another proximal synchronous neoplastic lesion in 3%-11% of cases, which modifies the management policy. However, this is often impossible because the endoscope cannot pass through the obstruction caused by the tumor or provides li
A large retrospective study conducted in China including 1474 patients operated on for obstructed colorectal carci
Another study conducted in China including 472 patients evaluated a new serum biomarker of chemokine ligand-7 that has been proposed for the diagnosis and prognosis of obstructed colorectal carcinoma[51].
Liquid biopsy could detect circulating cancer cells or their parts in serum before and after stenting mainly for prospec
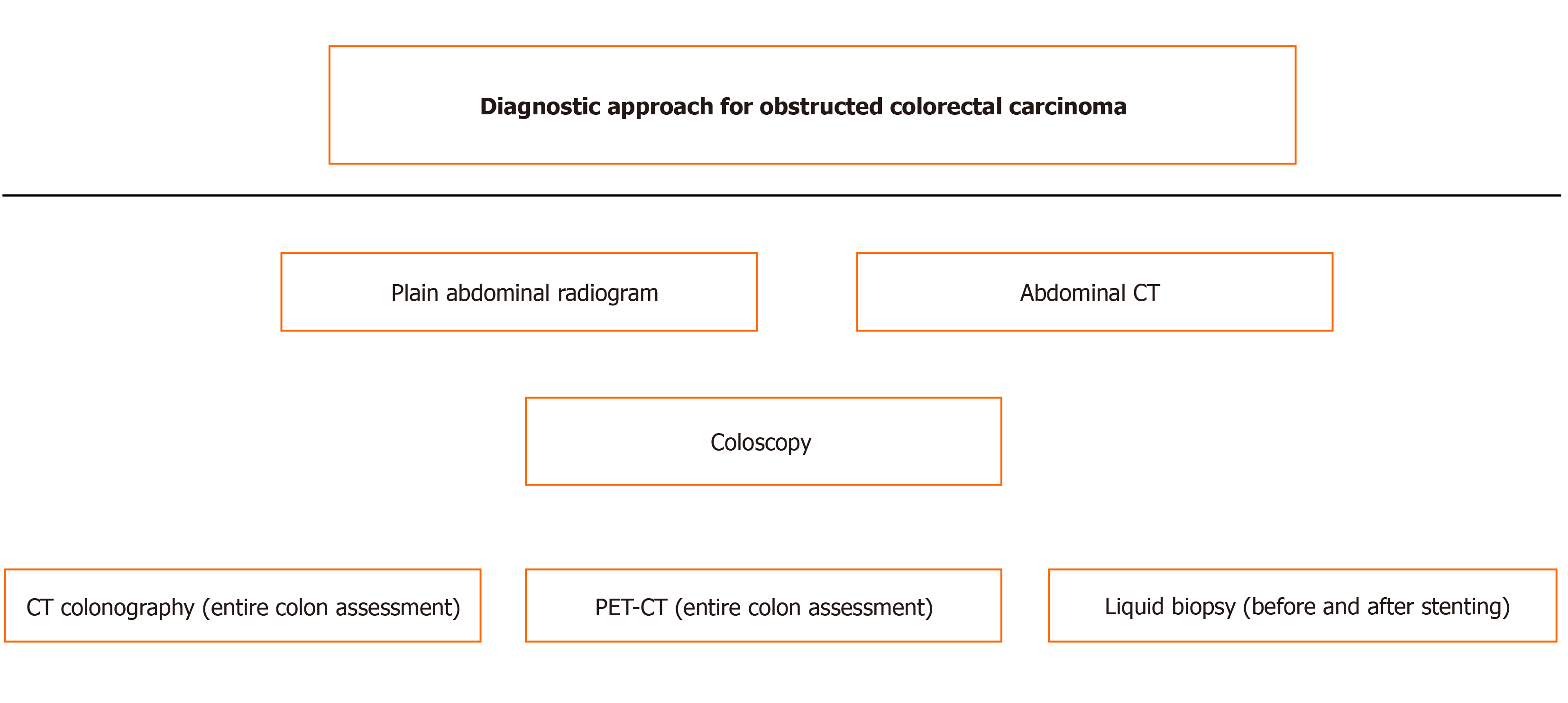
The surgical risk score has been found to be a reliable independent factor for predicting morbidity and mortality, which could be helpful in management decision-making[54]. The diagnostic steps are shown schematically in Figure 1.
In the World Society of Emergency Surgery guidelines, right colectomy is the treatment method of choice for right-sided obstruction. Self-expandable metallic stents are related to better short-term outcomes than emergency surgery for decom
According to the European Society of Gastrointestinal Endoscopy, although initially in 2014, the use of self-expandable metallic stents as a bridge to surgery was strongly discouraged but, since 2020, has been recommended after discussion and decision sharing with patients highly likely to be cured by surgical intervention. The time interval until surgical in
In the American Society of Colon and Rectal Surgeons guidelines, either emergency therapeutic radical resection or SEMS as a bridge-to-surgery mainly laparoscopic resection, are recommended. The choice of management should be individualized according to patient-related factors, equipment availability and expertise of the center. The rate of su
The current management policy depends on the location of acute obstruction. For right-sided curable obstruction, a therapeutic surgical intervention is indicated in most cases[18]. For left-sided obstruction, various choices exist, including curative resection accompanied or not accompanied by primary anastomosis, endoscopic stent placement usually or drainage placement, and diverting stoma formation[15,22,24,57]. It should be individualized in most cases[23] and accord
A large study conducted in Denmark and the United Kingdom (Yorkshire) assessed the trends in the surgical mana
Emergency decompression, either decompressing stoma or endoscopic stenting as a bridge to subsequent surgical resection on an elective basis, is considered to be highly beneficial for high-risk patients, particularly in geriatric frail patients equal to or above 70 years[60].
A large retrospective multicenter study conducted in the Netherlands including almost all hospitals (75 out of 77) and 2587 patients with curative resection of obstructed left-sided colorectal carcinoma (among them, 345 cases of decom
Another debatable issue concerns the optimal time interval between acute decompression and second-time curative resection. A comparative study conducted in the Netherlands including 168 patients with a time between decompression and repeat resection less than and more than 4 wk found a decrease in mortality (1.8% vs 12.3%) and an increase in 5-year survival (75% vs 51.4%)[62].
Self-expendable metal stents were introduced almost 20 years ago to relieve left-sided colorectal carcinoma stenosis. Since then, much progress has been made in improving the quality of equipment material, interventional techniques and expertise. There is no disagreement for their use in inoperable cases for palliative treatment[32,63-66], which in addition is more cost-effective and has shorter hospitalization than emergency surgery[67]. However, whether they should be applied as a bridge to surgery in suitable patients with potentially curable tumors, who could undergo therapeutic sur
The main argument in favor of stenting is based on the high possibility of a subsequent elective resection procedure instead of a high-risk emergency resection that has increased risks of morbidity and mortality[25,66,68-70]. Furthermore, it may increase the possibility of primary anastomosis limiting the creation of stomas and the chance for laparoscopic operations[1,32,39,65,71].
On the other hand, fears and reservations have to do with the risk of perforation and mainly microperforations that facilitate the spread of cancer cells. “Do not touch”, a basic postulate of traditional oncological surgery, means avoiding any manipulations of the tumor to prevent its dissemination. Notably, manipulations are not extrinsically high-risk but rather intrinsically high-risk (endoluminal) as there is a risk of partially fragmenting the tumor, thus opening the lumen[13,31,32,52,53].
Two cycles of preoperative chemotherapy with fluorouracil, leucovorin and oxaliplatin have been recommended to manage any cancer cell dissemination after stenting as a bridge to surgery restricting any potential unwilling effect of stent application[72]. It seems reasonable, but there are not survival data supporting this choice.
Self-expendable metal stents may be covered or uncovered and have diameters ranging between 10 and 25 mm and lengths between 60 and 12 mm[32,63,73]. A covered stent exhibited a higher migration rate and lower obstruction rate than an uncovered stent. Among the most commonly used are WallFlex, Niti-S, HANAROSTENT Naturfit, and JE
The use of supper-flexible metal stents has been proposed for the management of acute obstruction, where passing the stent through the right and left colonic curve may be difficult as it may be highly tortuous[74].
An interesting case in which a fully covered self-expandable metal stent was used for cecostomy to relieve an in
A systematic review and meta-analysis revealed that uncovered metal stents were related to fewer complications, tumor overgrowth, stent migration or need for reinsertion, and more stent patency; thus, they are more preferable to covered metal stents[76].
Migration is the main disadvantage of covered stents, which may occur in up to 40% of cases. A recent prospective randomized control trial conducted in Korea including 60 patients compared two types of covered stents, i.e., Flare and ComV. They found the following acceptable and comparable short-term results: (1) Technical success of 90% vs 96.7%; (2) clinical success of 85.2% vs 75.9%; and (3) stent migration of 11.1% vs 13.8%[77].
Perforation and peritonitis are more likely to occur after stenting in cases of benign acute obstructions. Thus, in benign cases, careful stenting is required due to an inherent high risk of perforation (22.4%), as suggested by a large nationwide study conducted in the United States including 4257 patients with self-expendable metal stent placement for relief of acute large bowel obstruction[78]. The evaluation of short-term stenting outcomes is shown in Table 1.
| Ref. | Patients (Nu) | Study | Tech success (%) | Clin success (%) | Perfo-ration (%) | Migration occlusion (%) |
| Recuenco et al[39] | 69 | Single center retrospective Spain | 97.5 | 91.3 | 13 | 2.9 |
| Angulo McGrath et al[63] | 92 | Single center retrospective Spain | 92.4 | 89.1 | 9.8 | - |
| Sasaki et al[81] | 202 | Single center retrospective Japan | 97.5 | 96 | 0 | 2.5 |
| Yan et al[49] | 434 | Single center retrospective China | 98.6 | 94.9 | 1,4 | 0.5 |
| Kuwai et al[87] | 208 | Multicenter prospective Japan | 99 | 92.8 | 1.9 | 1.3 |
| Lee et al[77] | 60 | Single center retrospective Korea | 93.3 | 80.5 | 5.3 | 12.5 |
Balloon dilatation is not recommended before stenting. Plain abdominal radiogram after stenting is necessary to assess the stent position and to exclude perforation based on the absence of intraabdominal free-air[48,79]. A multicenter retro
A nationwide retrospective cohort study conducted in the United States including 9706 patients with left-sided obstructed colorectal carcinoma found that a minority of 9.7% underwent stenting as a bridge to surgery, while most of them underwent emergency surgery. The bridging rate increased from 7.7% in 2010 to 16.4% in 2016. It was related to a lower incidence of stoma formation than emergency surgery and had comparable short-term outcomes in terms of morbidity and mortality rates. There were no long-term oncological outcomes[1].
There have been conflicting aspects about the safety and long-term oncological outcomes of self-expendable metal stents used as a bridge to surgery for left-sided acute obstruction in patients with colorectal carcinoma. A recent study conducted in Spain including 110 such patients showed a technical success rate of 95.7% and clinical effectiveness rate of 91.3%; a perforation rate of 13% and migration, occlusion rate of 2.9%; a higher rate following laparoscopic colectomy; a lower rate of colostomy, morbidity and mortality than emergency curative resection; and similar rates with the latter of overall survival and disease-free survival[39].
Another recent study conducted in Spain including 92 patients with obstructed left-sided colorectal carcinoma (two-thirds as bridging and one-third for palliation of inoperable tumor) reported a technical success rate of 92.4%, clinical effectiveness rate of 89.1% and perforation rate of 9.8%[63].
Another recent study conducted in Japan assessing the use of self-expendable metal stents with low axial force in 202 patients for the management of left-sided obstruction in patients with colorectal carcinoma, the technical success rate was 97.5%, clinical effectiveness rate was 96%, stent migration rate was 1%, stent occlusion rate was 1.5%, and there was no perforation attributed to that type of stent[81].
A retrospective study conducted in China including 434 patients using a two-person method reported a technique success rate of 98.6%, clinical effectiveness rate of 94.9% and complication rate of 4.4%. These included mainly bowel perforation (1.4%), stent migration (0.5%), stent detachment (0.7%) and stool impaction (1.4%)[49].
In a retrospective comparative study conducted in Japan including 48 patients with left-sided colorectal carcinoma, as a bridge to surgery, decompression by self-expendable metal stents or transanal tubes had similar complication and 5-year survival rates but the stenting group had better clinical success rates, shorter time to oral intake and better albumin levels[28]. Likewise, a systematic review and meta-analysis showed results in favor of metal stents, even in obstructions located in the right colon[29]. The comparison of results between stenting and tubing as a bridge to surgery is shown in Table 2.
| Ref. | Patients (Nu) | Study | Clin success | Complications | Survival |
| Inoue et al[28] | 48 | Single center retrospective Japan | Better in stenting (100% vs 80.6%) | Similar (0 vs 4%) | Equivalent (5-yr: 69.5% vs 38.4%) |
| Xu et al[29] | 704 | Meta-analysis China | Better in stenting (94.5% vs 86.1%) | Fewer in stenting (6.9% vs 12.4%) | - |
| Kagami et al[30] | 53 | Single center retrospective Japan | Better in stenting (100% vs 81.8%) | Fewer in stenting (0 vs 18.2%) | Equivalent (3-yr: 73% vs 80.9%) |
| Matsuda et al[89] | 581 | Meta-analysis Japan | Better in stenting (93.2% vs 77.3%) | Equivalent (5.5% vs. 11.7%) | - |
| Numata et al[31] | 225 | Multicenter prospective Japan | Better in stenting (92.6% vs 75.3%) | Fewer posto-perative in stenting (21.1% vs 33.3%) | Similar (3 yr: 87.1% vs 90.5%) |
| Takahashi et al[53] | 35 | Single center prospective Japan | Similar (88% vs 90%) | Similar (12% vs 10%) | 1Increased circulating DNA on day 7 in stenting (992 vs 308 ng/mL) |
| Suzuki et al[18] | 40 | Single center retrospective Japan | Similar (89.5% vs 85.7%) | Similar (10.5% vs 14.2%) | Better in tubing (5 yr: 79.5% vs 32%) |
A retrospective comparative study conducted in Egypt including 65 patients with American Society of Anesthesiologists (ASA) scores ≥ III, acute obstruction and an inoperable case of colorectal carcinoma stage IV located in the rectosigmoid region assessed the short-term outcomes of both stenting and Hartmann’s operation. They reported tech
A retrospective study conducted in the United States including 199 patients who underwent stenting for obstructed inoperable colorectal carcinoma stage IV found a high technical success rate but not proportional clinical effectiveness. The perforation rate was comparable in patients treated with and without bevacizumab[83].
Another retrospective comparative study conducted in Spain including 95 patients with obstructed inoperable colo
A recent systematic review and meta-analysis including 10 studies and 1273 patients found higher perineural and lymphatic invasion after stenting as a bridge to surgery that led to worse overall survival than initial surgery[85].
Another recent systematic review and meta-analysis including 27 studies and 3894 patients after stenting as a bridge to surgery found similar results for initial surgery, 3-year and 5-year disease-free survival and overall survival[86]. Com
| Ref. | Patients (Nu) | Study | Morbidity | Mortality | Long-term outcome |
| McKechnie et al[24] | 9403 | Meta-analysis Canada | Similar (27.2% vs 27.8%) | Improved in stenting (4.4% vs 6.1%) | Equivalent (insufficient data) |
| Paniagua García-Señoráns et al[42] | 251 | Single centre Retrospective Spain | Improved in stenting (36% vs 62.5%) | Equivalent (5.3% vs 6.3%) | Equivalent (3-yr DFS: 31.4.6% vs 33.4%, 3-yr OS: 37.5% vs 36.1%) |
| Wang et al[70] | 78 | Single centre Retrospective China | Similar (16.2% vs 26.8%) | Similar (0 vs 4.9%) | Similar (median overall survival: 36 months for both groups) |
| Hadaya et al[1] | 9706 | Nation-wide United States | Similar (12.2% vs 14.4%) | Similar (1.2% vs 3.4%) | Undetermined |
| Balciscueta et al[85] | 1273 | Meta-analysis Spain | - | - | Worse in stenting; 1Higher risk of perineural (45.6% vs 32.6%)- lymphatic (47.4 % vs 42%) invasion |
| Spannenburg et al[86] | 3894 | Meta-analysis Australia | Improved in stenting (26.09% vs 41.4%) | Improved in stenting (6.5% vs 8.1%) | Similar recurrence (31% vs 25%) |
| Boeding et al[101] | 600 | Meta-analysis Netherlands | Improved in stenting (30% vs 42%) | Improved in stenting (1.2% vs 7.2%) | Similar (5-yr DFS: 65.6% vs 63.1%, 5-yr OS: 66.9% vs 64%) |
In a recent multicenter prospective study conducted in 46 Japanese hospitals, WallFlex stents were implanted in 208 patients with left-sided obstruction of colorectal carcinoma (stage II and III) and not only were short-term outcomes evaluated but also long-term oncological outcomes. They found interesting rates: (1) Overall survival: 1-year of 94.1%, 3-year of 77.4%, 5-year of 67.4%; (2) relapse free survival: 1-year of 81.6%, 3-year of 65.6%, 5-year of 57.9%; (3) technical success of 99% and clinical success rate of 92.8%; (4) perforation of 1.9% and migration, occlusion rate of 1.3%; and (5) overall recurrence of 31% and it was poorer in four perforation cases. These long-term outcomes have been considered satisfactory and attributed to a notably low perforation rate[87].
A retrospective nationwide comparative study conducted in Sweden including 196 patients with acute obstruction colorectal carcinoma assessed the long-term outcomes between stenting and colostomy as a bridge to surgery. They found comparable long-term outcomes but less permanent colostomy, more surgical resections, and shorter hospitalization in the stenting group[88].
Endoscopic transanal drainage tubes (retrograde bowel drainage tubes or Dennis colorectal tubes) have been used as alternatives to endoscopic self-expendable metal stents as bridges to surgery for decompression of acute left-sided co
However, metal stents have been proven to be more effective and related to fewer complications than drainage tubes[28,29]. Likewise, a study conducted in Japan including 53 patients with obstructed left-sided colorectal carcinoma com
A meta-analysis including 581 patients compared the short-term outcomes between endoscopic transanal tubes and self-expandable metal stents for decompression as a bridge to surgery in obstructed colorectal carcinoma. They found that stenting and tubing had equivalent morbidity and mortality after surgery[89].
A recent multicenter study conducted in Japan including 10 hospitals and 225 patients with obstructed colorectal carcinoma compared transanal decompression tubes and self-expandable metal stents. They found similar long-term outcomes, i.e., 3-year relapse-free survival (66.7% vs 69.9%) and 3-year overall survival (90.5% vs 87.1%), between the tubing and stenting groups. However, the short-term outcome showed that stenting was favored over tubing regarding less stoma formation, fewer complications and shorter hospitalization[31].
Another study conducted in Japan including 35 patients with obstructed colorectal carcinoma performed genomic analysis (liquid biopsy) in addition to clinical outcome assessment and compared transanal tubes and self-expandable metal stents. They found similar short-term outcomes, but stenting increased the levels of circulating cell-free DNA and circulating tumor DNA in plasma, in contrast to no increase in the tubing group. This was attributed to mechanical com
Otherwise, for right-sided obstructed colorectal carcinoma, although the method of choice must be emergency curative surgical resection, a study conducted in Japan including 40 patients compared endoscopic tubes (transanal or transnasal) and endoscopic self-expandable metal stents as the choice for bridging to surgery and found similar morbidity, clearly better 5-year overall survival (79.5% vs 32%), and 3-year disease-free survival (68.9% vs 45.9%) rates in the tubing group than in the stenting group[18]. The advantages and disadvantages of tubing and stenting are shown in Table 4.
| Method | Advantages | Disadvantages |
| Endoscopic stenting | Higher clinical success; fewer complications | More expensive |
| Endoscopic tubing | Lower cost | Lower clinical success; more complications |
Surgery constitutes the main treatment option for obstructed colorectal carcinoma stage II or III, aiming for a potent sustainable or permanent cure[17,19,24,90]. For right-sided obstruction involving the cecum, ascending colon, hepatic flexure, and transverse colon, the operative plan is clear and depends basically on therapeutic right colectomy with ex
A recent nationwide retrospective study conducted in the Netherlands including 525 patients with obstructed right-sided colon carcinoma found that primary resection and anastomosis were performed in 88% of patients with defunctioning ileostomy (25%), and staged resection after stenting or tubing was used as a bridge to surgery in 5% of cases[20].
A French nationwide retrospective study including 776 patients with right obstructed colon cancer showed primary resection 92% accompanied by anastomosis 82% with added defunctioning loop ileostomy 3.6% or accompanied by dou
In addition to radical traditional right colectomy, extended right colectomy removes the entire transverse colon with both flexures when the carcinoma involves the transverse colon, and primary ileocolic anastomosis is the method of first choice. A defunctioning proximal loop ileostomy may sometimes be preferred. Additionally, excision without anasto
For left-sided obstruction involving the splenic flexure, descending colon, sigmoid, and rectum, there are several different operative plans, but the optimal management is conflicting. Wide resection with extended lymphadenectomy, including total mesocolon or mesorectal excision, primary anastomosis or Hartmann’s procedure, is the most widely used. Other operative options include subtotal or total colectomy with ileorectal anastomosis, when large dilatation and ischemic changes of the colon exist, urgent decompressing colostomy followed by surgical resection in the first stage and anastomosis in the second stage (two-stage procedure) and colostomy reversal in the third stage (three-stage procedure)[16].
The French nationwide study including 1500 patients with obstructed left-sided colorectal carcinoma found that their primary management was based on endoscopic stenting in 18% of cases. Emergency surgical management consists of diverting colostomy (38%), segmental colectomy (27%), Hartmann’s procedure (20%), and subtotal colectomy (15%). By multivariate analysis, diverting colostomy and segmental colectomy had a better prognosis than the other two operative options. They advocated, as surgical options, diverting colostomy in high-risk patients, and Hartmann’s procedure or subtotal colectomy in cases with ischemia or perforation[90].
For left-sided acute obstruction, the choice of emergency decompression colostomy or endoscopic stenting depends on the management plan. The former is preferable in operable cases, while the latter is preferable in inoperable cases as palliative treatment[92].
A systematic review and meta-analysis showed primary anastomosis was more frequent in patients with decom
Total mesocolon excision, which is of great importance for harvested lymph node extended dissection and determines the radicality of surgical resection affecting the oncological outcome, has been found that after sigmoidectomy for car
Various methods have been applied for stoma creation, either ileostomy or colostomy, to avoid the main complication of parastomal hernia. It may occur in 40% of cases within 2 years, affecting quality of life and causing obstructive ileus[94].
Pelvic exenteration even in the emergency setting, such as acute obstruction of rectal carcinoma, could be performed safely in terms of radicality, offering satisfactory results with a 3-year overall survival of 54.4%[33].
For splenic flexure location (5%), there are operative difficulties, which increase morbidity and mortality; thus, much attention must be paid during surgery. Similar technical difficulties may be encountered with stent placement in such locations. A recent large French multicenter study including 58 centers and 2325 patients with obstructed colorectal car
The previously mentioned French nationwide study including all 1957 patients with obstructive colorectal cancer recently compared the results of 56 centers with different hospital volumes. They found that it did not affect the outcomes of emergency management alone, but when the outcome of overall management was assessed, it influenced the mor
A retrospective study conducted in China including 839 patients with emergency surgery for obstructed colorectal carcinoma evaluated a modified ERAS protocol (enhanced recovery after surgery). They found faster bowel movements, fewer complications and shorter hospitalization[96].
The incidence of surgical site infections, the main cause of nosocomial infections, is increased after emergency surgery for obstructed colorectal carcinoma[97].
It has been reported that in inoperable obstructed carcinoma with peritoneal metastases, debulking surgery could improve symptom relief and survival without increasing morbidity and mortality[98].
One-stage resection with on-table bowel decompression and irrigation accompanied by primary anastomosis must be the preferred choice in younger (under 70 years), fit patients without major comorbidities, with ASA score I or II[17,40,99,100]. A recent systematic review including 9 studies and 600 patients with obstructed right-sided colorectal carcinoma found that one-stage surgery had more complications (42% vs 30%) and higher mortality (7.2% vs 1.2%) but similar 5-year overall and disease-free survival when compared to staged treatment[101].
A distended colon without any preparation discourages many surgeons from performing primary anastomosis, thus preferring Hartmann’s procedure. However, the performance of anastomosis and the addition of a defunctioning stoma may overcome these fears. Given Hartmann’s procedure reversal can occur at least 3-6 months after the initial operation, or even never, sometimes disturbing the quality of life[102], it is often more complicated and copious than reversal within one month of a right-sided loop transverse colostomy or loop ileostomy; thus, this addition could be a reasonable al
A recent retrospective multicenter study conducted in Japan including 520 patients with obstructed colorectal car
Although the routine use of prophylactic intraabdominal drainage for colorectal anastomosis is not recommended in general, for emergency primary anastomosis due to obstructed colorectal carcinoma, it is a justifiable choice[104].
This approach basically avoids the need for primary anastomosis and includes: (1) The most widely applicable Hart
Emergency stoma for urgent decompression may be either transverse colostomy (right-left) and sigmoid colostomy or loop ileostomy of the terminal ileum. Second, elective surgical resection and anastomosis can be performed in operable cases[46].
The site of colostomy depends on the tumor location and preference of the surgeon. Comparing transverse colostomy to sigmoid colostomy, no other difference was found, but the latter had a lower risk of prolapse than the former[7].
A recent study conducted in Taiwan including 191 patients with left-sided obstructed colorectal carcinoma showed that the two-stage procedure had more complications (57.1% vs 36%) than the three-stage procedure, including mainly surgical site infection and wound dehiscence. In addition, they found similar rates of anastomotic leakage, 5-year overall survival (33% vs 35%), and 5-year disease-free survival (60% vs 58.4%)[16]. There are well-defined incriminating factors for wound dehiscence after colorectal carcinoma surgery[107], which must be considered, particularly in emergency surgery.
Decompressing colostomy as a bridge to surgery for left-sided obstructed colorectal carcinoma is being more frequently performed. A recent nationwide study conducted in 75 Dutch hospitals including 236 patients who underwent emergency decompression colostomy and 472 patients who underwent emergency resection for left-sided obstructed colorectal carcinoma compared the results of these two management options. They found that primary decompression colostomy was accompanied by more subsequent laparoscopic resections and anastomoses (56.8% vs 9.2%) than primary resection, lower 90-d mortality (1.7% vs 7.2%) and permanent stoma (23.4% vs 42.4%) rates, and higher 3-year overall survival rates (79.4% vs 73.3%). This two-stage surgical management approach could be followed to improve outcomes, particularly in elderly individuals over 70 years[108].
It has been found that the reversal of Hartmann’s procedure is associated with a notable morbidity of 34%, including mainly surgical site infection (22%) and anastomotic leakage (5%), and mortality of 8.3%, especially in patients with obesity and a high ASA score (≥ 3)[106].
Neoadjuvant chemotherapy after emergency decompressing stoma creation and before subsequent elective resection may be an option that could improve the prognosis[109].
This approach has not gained wide acceptance and follows a two-stage procedure, the primary decompressing stoma was created, which was left in site for possible protection of secondary anastomosis and would be closed a third time[16].
The applicability of emergency laparoscopic surgery for left-sided obstructed colorectal carcinoma is limited[24]. A na
It is well known that emergency surgery reduces long-term survival in cancer patients. It has also been confirmed in emergency colorectal resection[111]. A recent study conducted in Austria including 59 patients (4.5%) who underwent emergency colectomy for colorectal carcinoma among 1297 patients treated with elective colectomy for colorectal car
A recent nationwide retrospective study conducted in the Netherlands including 525 patients managed for obstructed (7%) and 6891 patients managed for nonobstructive (93%) right-sided colon carcinoma found that in all stages, obstruc
Mortality after emergency surgery for obstructed colorectal carcinoma reaches up to 11.72%. Various high-risk pre
Obstructions involving the splenic flexure have a worse prognosis than those in other locations[46]. Obese patients with obstructive colorectal cancer exhibit more severe clinical presentation than those without obesity and similar postoperative morbidity but more colostomy complications in left-sided cases[113].
Comorbidities such as cardiovascular, cerebral, chronic obstructive disease and diabetes mellitus may affect the oncological outcome of colorectal carcinoma patients, including acute obstruction[114].
After emergency surgery for obstructed colorectal carcinoma, elderly patients have increased morbidity and reduced survival, mainly those over 84 years[105]. The finding of an obstructive colorectal carcinoma on coloscopy predicts more advanced stage and reduced overall survival[115]. Some prognostic systems, such as the modified inflammation marker Glasgow score, may predict the long-term oncological outcome in obstructed colorectal carcinoma[116].
Obstructed colorectal carcinoma is common in the emergency setting and is the main cause of colon-related obstructive ileus mainly in elderly patients. It requires emergency decompression to prevent more severe complications. For right-sided obstructions, one-stage emergency resection surgery and primary anastomosis are widely accepted. For left-sided obstructions, there are conflicting aspects. Emergency one-stage on-table bowel decompression, surgical resection and primary anastomosis accompanied or not, by loop right transverse colostomy or loop ileostomy, must be the method of choice for fit patients under 70 years. However, in daily clinical practice, the two-stage Hartmann’s procedure is favored worldwide. In unfit patients, emergency decompression by endoscopic self-expandable metal stents mainly or decom
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Feng B, China; Qi L, China; Yan B, China S-Editor: Qu XL L-Editor: A P-Editor: Xu ZH
| 1. | Hadaya J, Verma A, Sanaiha Y, Mabeza RM, Chen F, Benharash P. Preoperative stents for the treatment of obstructing left-sided colon cancer: a national analysis. Surg Endosc. 2023;37:1771-1780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 2. | Samuel G, Kratzer M, Asagbra O, Kinderwater J, Poola S, Udom J, Lambert K, Mian M, Ali E. Facilitators and barriers to colorectal cancer screening in an outpatient setting. World J Clin Cases. 2021;9:5850-5859. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Singh P, Patel K, Arya P, Singh E, Mishra A. A Comparison of Emergency First Presentations of Colorectal Cancer in Under-50 and Over-50 Year-Old Patients. J Invest Surg. 2020;33:514-519. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Esswein K, Ninkovic M, Gasser E, Barenberg L, Perathoner A, Kafka-Ritsch R. Emergency resection is an independent risk factor for decreased long-term overall survival in colorectal cancer: a matched-pair analysis. World J Surg Oncol. 2023;21:310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 5. | Rudolph C, Engholm G, Pritzkuleit R, Storm HH, Katalinic A. Colorectal Cancer Survival in German-Danish Border Regions-A Registry-Based Cohort Study. Cancers (Basel). 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Tan WJ, Lin W, Sultana R, Foo FJ, Tang CL, Chew MH. A prognostic score predicting survival following emergency surgery in patients with metastatic colorectal cancer. ANZ J Surg. 2021;91:2493-2498. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Dylen MYC, Lee JWK, Ting LY, Ragupathi T, Yu NJ, Lim F, Farouk R, Seng CC. Transverse Colostomy Differs in Outcomes Compared to Sigmoid Colostomy: A Cohort Analysis. J Invest Surg. 2022;35:783-787. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 8. | Ali G, Shaukat A, Masood S, Akram B, Ghaffar A, Gondal KM. A Profile of Colorectal Tumors Presenting as Emergency. J Coll Physicians Surg Pak. 2021;31:74-78. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Ndlovu N, Kader S, Moodley Y, Cheddie S, Madiba TE. A South African central hospital's experience with malignant colorectal obstruction. S Afr J Surg. 2023;61:139-143. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Lauro A, Binetti M, Vaccari S, Cervellera M, Tonini V. Obstructing Left-Sided Colonic Cancer: Is Endoscopic Stenting a Bridge to Surgery or a Bridge to Nowhere? Dig Dis Sci. 2020;65:2789-2799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Schootman M, Jeffe DB, Ratnapradipa KL, Eberth JM, Davidson NO. Increased 30-Day Mortality Risk in Patients With Diabetes Mellitus After Colon Cancer Surgery: A Mediation Analysis. Dis Colon Rectum. 2020;63:290-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Bento JH, Bianchi ET, Tustumi F, Leonardi PC, Junior UR, Ceconello I. Surgical Management of Malignant Intestinal Obstruction: Outcome and Prognostic Factors. Chirurgia (Bucur). 2019;114:343-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Seo SY, Kim SW. Endoscopic Management of Malignant Colonic Obstruction. Clin Endosc. 2020;53:9-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Chan HC, Huang CC, Chattopadhyay A, Yeh KH, Lee WC, Chiang CJ, Lee HY, Cheng SH, Lu TP. Predicting Colon Cancer-Specific Survival for the Asian Population Using National Cancer Registry Data from Taiwan. Ann Surg Oncol. 2022;29:853-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | EuroSurg Collaborative. Acute PresentatiOn of coLorectaL cancer - an internatiOnal snapshot (APOLLO): Protocol for a prospective, multicentre cohort study. Colorectal Dis. 2023;25:144-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Lin YZ, Cheng HH, Huang SC, Chang SC, Lan YT. Comparison of two-stage and three-stage surgery for obstructing left-sided colon cancer. ANZ J Surg. 2022;92:1466-1471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Yoo RN, Cho HM, Kye BH. Management of obstructive colon cancer: Current status, obstacles, and future directions. World J Gastrointest Oncol. 2021;13:1850-1862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Suzuki Y, Moritani K, Seo Y, Takahashi T. Comparison of decompression tubes with metallic stents for the management of right-sided malignant colonic obstruction. World J Gastroenterol. 2019;25:1975-1985. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Mege D, Manceau G, Beyer-Berjot L, Bridoux V, Lakkis Z, Venara A, Voron T, Brunetti F, Sielezneff I, Karoui M; AFC (French Surgical Association) Working Group. Surgical management of obstructive right-sided colon cancer at a national level results of a multicenter study of the French Surgical Association in 776 patients. Eur J Surg Oncol. 2018;44:1522-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Boeding JRE, Elferink MAG, Tanis PJ, de Wilt JHW, Gobardhan PD, Verhoef C, Schreinemakers JMJ. Surgical treatment and overall survival in patients with right-sided obstructing colon cancer-a nationwide retrospective cohort study. Int J Colorectal Dis. 2023;38:248. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Burke JR, Brown P, Quyn A, Lambie H, Tolan D, Sagar P. Tumour growth rate of carcinoma of the colon and rectum: retrospective cohort study. BJS Open. 2020;4:1200-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 22. | Giordano A, Podda M, Montori G, Botteri E, Fugazzola P, Ortenzi M, Guerrieri M, Vettoretto N, Agresta F, Sartori A, Bergamini C, Martellucci J, Guariniello A, Fransvea P, Azzinnaro A, Scatizzi M, Catena F, Coccolini F, Ansaloni L, Sartelli M, Sapienza P, Mingoli A, Prosperi P. Colonic Resection, Stoma, or Self-expanding Metal Stents for Obstructive Left Colon Cancer: the CROSCO-1 study protocol. Minerva Surg. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 23. | Girardot-Miglierina A, Kefleyesus A, Clerc D, Grass F, Demartines N, Hübner M, Hahnloser D. [Obstructed colon cancer: which strategy in 2022?]. Rev Med Suisse. 2022;18:1192-1199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | McKechnie T, Springer JE, Cloutier Z, Archer V, Alavi K, Doumouras A, Hong D, Eskicioglu C. Management of left-sided malignant colorectal obstructions with curative intent: a network meta-analysis. Surg Endosc. 2023;37:4159-4178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 25. | Chan DKH, Tan KK. Stenting versus surgery in obstructed malignant colorectal cancer-a review of short and long-term results. J Gastrointest Oncol. 2020;11:486-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Lam J, Chauhan V, Lam I, Kannappa L, Salama Y. Colorectal stenting in England: a cross-sectional study of practice. Ann R Coll Surg Engl. 2020;102:451-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Webster PJ, Aldoori J, Burke DA. Optimal management of malignant left-sided large bowel obstruction: do international guidelines agree? World J Emerg Surg. 2019;14:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Inoue H, Arita T, Kuriu Y, Shimizu H, Kiuchi J, Yamamoto Y, Konishi H, Morimura R, Shiozaki A, Ikoma H, Kubota T, Fujiwara H, Okamoto K, Otsuji E. Emergency Management of Obstructive Colorectal Cancer - A Retrospective Study of Efficacy and Safety in Self-expanding Metallic Stents and Trans-anal Tubes. In Vivo. 2021;35:2289-2296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 29. | Xu J, Zhang S, Jiang T, Zhao YJ. Transanal drainage tubes vs metallic stents for acute malignant left-sided bowel obstruction: A systematic review and meta-analysis. Medicine (Baltimore). 2020;99:e18623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Kagami S, Funahashi K, Ushigome M, Koike J, Kaneko T, Koda T, Kurihara A, Nagashima Y, Yoshino Y, Goto M, Mikami T, Chino K. Comparative study between colonic metallic stent and anal tube decompression for Japanese patients with left-sided malignant large bowel obstruction. World J Surg Oncol. 2018;16:210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 31. | Numata K, Numata M, Shirai J, Sawazaki S, Okamoto H, Godai T, Katayama Y, Atsumi Y, Kazama K, Uchiyama M, Kohmura T, Mushiake H, Sugano N, Higuchi A, Kato A, Iguchi K, Rino Y, Shiozawa M. Short- and long-term outcomes of transanal decompression tube and self-expandable metallic stent for obstructive colorectal cancer based on a multicenter database (KYCC2110). J Surg Oncol. 2023;128:1372-1379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 32. | Binetti M, Lauro A, Tonini V. Colonic stent for bridge to surgery for acute left-sided malignant colonic obstruction: A review of the literature after 2020. World J Clin Oncol. 2022;13:957-966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 33. | Thiptanakit C, Chowchankit I, Panya S, Kanjanasilp P, Malakorn S, Pattana-Arun J, Sahakitrungruang C. Urgent Pelvic Exenteration: Should the Indication Be Extended? Dis Colon Rectum. 2018;61:561-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Nekkanti SS, Jajoo B, Mohan A, Vasudevan L, Peelay Z, Kazi M, Desouza A, Saklani A. Empty pelvis syndrome: a retrospective audit from a tertiary cancer center. Langenbecks Arch Surg. 2023;408:331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 35. | Rosen CB, Roberts SE, Wirtalla CJ, Keele LJ, Kaufman EJ, Halpern SD, Reilly PM, Neuman MD, Kelz RR. The Conditional Effects of Multimorbidity on Operative Versus Nonoperative Management of Emergency General Surgery Conditions: A Retrospective Observational Study Using an Instrumental Variable Analysis. Ann Surg. 2023;278:e855-e862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Johnson KM, Newman KL, Green PK, Berry K, Cornia PB, Wu P, Beste LA, Itani K, Harris AHS, Kamath PS, Ioannou GN. Incidence and Risk Factors of Postoperative Mortality and Morbidity After Elective Versus Emergent Abdominal Surgery in a National Sample of 8193 Patients With Cirrhosis. Ann Surg. 2021;274:e345-e354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 37. | Eugene N, Kuryba A, Martin P, Oliver CM, Berry M, Moppett IK, Johnston C, Hare S, Lockwood S, Murray D, Walker K, Cromwell DA; NELA Project Team. Development and validation of a prognostic model for death 30 days after adult emergency laparotomy. Anaesthesia. 2023;78:1262-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 38. | Kaufman EJ, Keele LJ, Wirtalla CJ, Rosen CB, Roberts SE, Mavroudis CL, Reilly PM, Holena DN, McHugh MD, Small D, Kelz RR. Operative and Nonoperative Outcomes of Emergency General Surgery Conditions: An Observational Study Using a Novel Instrumental Variable. Ann Surg. 2023;278:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 39. | Recuenco CB, Septiem JG, Díaz JA, Vasallo IJT, de la Madriz AA, Carneros VJ, Rodríguez JLR, Navalón JMJ, Miramón FJJ. Effect of self-expandable metal stent on morbidity and mortality and oncological prognosis in malignant colonic obstruction: retrospective analysis of its use as curative and palliative treatment. Int J Colorectal Dis. 2022;37:475-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 40. | Pisano M, Zorcolo L, Merli C, Cimbanassi S, Poiasina E, Ceresoli M, Agresta F, Allievi N, Bellanova G, Coccolini F, Coy C, Fugazzola P, Martinez CA, Montori G, Paolillo C, Penachim TJ, Pereira B, Reis T, Restivo A, Rezende-Neto J, Sartelli M, Valentino M, Abu-Zidan FM, Ashkenazi I, Bala M, Chiara O, De' Angelis N, Deidda S, De Simone B, Di Saverio S, Finotti E, Kenji I, Moore E, Wexner S, Biffl W, Coimbra R, Guttadauro A, Leppäniemi A, Maier R, Magnone S, Mefire AC, Peitzmann A, Sakakushev B, Sugrue M, Viale P, Weber D, Kashuk J, Fraga GP, Kluger I, Catena F, Ansaloni L. 2017 WSES guidelines on colon and rectal cancer emergencies: obstruction and perforation. World J Emerg Surg. 2018;13:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 244] [Cited by in RCA: 193] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 41. | Zwanenburg ES, Veld JV, Amelung FJ, Borstlap WAA, Dekker JWT, Hompes R, Tuynman JB, Westerterp M, van Westreenen HL, Bemelman WA, Consten ECJ, Tanis PJ; Dutch Snapshot Research Group. Short- and Long-term Outcomes After Laparoscopic Emergency Resection of Left-Sided Obstructive Colon Cancer: A Nationwide Propensity Score-Matched Analysis. Dis Colon Rectum. 2023;66:774-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 42. | Paniagua García-Señoráns M, Sánchez Santos R, Cano Valderrama Ó, Vigorita V, de Castro Parga ML, Cea Pereira S, Rodríguez Fernández L, Moncada Iribarren E. Stent as bridge to surgery decreases postoperative complications without worsening oncological outcomes: retrospective unicentric cohort study and stent placement protocol. Surg Endosc. 2023;37:6298-6307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 43. | Moutzoukis M, Argyriou K, Kapsoritakis A, Christodoulou D. Endoscopic luminal stenting: Current applications and future perspectives. World J Gastrointest Endosc. 2023;15:195-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 44. | Wang S, Fan Z. The role of GSTM1 gene polymorphism in pathophysiology, evaluation, and management of constipation of anorectal outlet obstruction. Cell Mol Biol (Noisy-le-grand). 2021;67:163-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 45. | Mege D, Manceau G, Beyer L, Bridoux V, Lakkis Z, Venara A, Voron T, de'Angelis N, Abdalla S, Sielezneff I, Karoui M; AFC (French Surgical Association) Working Group. Right-sided vs. left-sided obstructing colonic cancer: results of a multicenter study of the French Surgical Association in 2325 patients and literature review. Int J Colorectal Dis. 2019;34:1021-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 46. | Labiad C, Manceau G, Mege D, Cazelles A, Voron T, Bridoux V, Lakkis Z, Abdalla S, Karoui M; AFC (French Surgical Association) Working Group. Emergency surgery for obstructive splenic flexure colon cancer: results of a multicentric study of the French Surgical Association (AFC). Updates Surg. 2022;74:107-115. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 47. | McGarry J, Ng ZQ, Ryan F, Theophilus M. Utility of CT colonography and/or PET-CT preoperatively in obstructing left-sided colorectal cancers - a systematic review. ANZ J Surg. 2023;93:1487-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 48. | Matsuda A, Yamada T, Takahashi G, Matsumoto S, Yokoyama Y, Sonoda H, Ohta R, Shinji S, Sekiguchi K, Kuriyama S, Kanaka S, Yoshida H. Postoperative infectious complications have a negative oncological impact in patients after stent placement with malignant large bowel obstruction. Int J Colorectal Dis. 2023;38:2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 49. | Yan FH, Zhang Y, Bian CL, Liu XS, Chen BC, Wang Z, Wang H, Ji-Fu E, Yu ED. Self-expanding metal stent insertion by colorectal surgeons using a two-person approach colonoscopy without fluoroscopic monitoring in the management of acute colorectal obstruction: a 14-year experience. World J Surg Oncol. 2021;19:194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 50. | Cao Y, Ke S, Gu J, Mao F, Yao S, Deng S, Yan L, Wu K, Liu L, Cai K. The Value of Haematological Parameters and Tumour Markers in the Prediction of Intestinal Obstruction in 1474 Chinese Colorectal Cancer Patients. Dis Markers. 2020;2020:8860328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 51. | Li L, Zhang L, Zhang T, Qi X, Cheng G, Xia L. Serum Chemokine CXCL7 as a Potential Novel Biomarker for Obstructive Colorectal Cancer. Front Oncol. 2020;10:599363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 52. | Ishibashi R, Yoshida S, Odawara N, Kishikawa T, Kondo R, Nakada A, Hakuta R, Takahara N, Tanaka E, Sekiba K, Seimiya T, Ohnaga T, Otsuka M, Koike K. Detection of circulating colorectal cancer cells by a custom microfluid system before and after endoscopic metallic stent placement. Oncol Lett. 2019;18:6397-6404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 53. | Takahashi G, Yamada T, Iwai T, Takeda K, Koizumi M, Shinji S, Uchida E. Oncological Assessment of Stent Placement for Obstructive Colorectal Cancer from Circulating Cell-Free DNA and Circulating Tumor DNA Dynamics. Ann Surg Oncol. 2018;25:737-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 54. | Collard MK, Moszkowicz D, Clause-Verdreau AC, Beauchet A, Cudennec T, Vychnevskaia K, Malafosse R, Peschaud F. Postoperative morbidity and mortality for malignant colon obstruction: the American College of Surgeon calculator reliability. J Surg Res. 2018;226:112-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 55. | van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Götz M, van Halsema EE, Hill J, Manes G, Meisner S, Rodrigues-Pinto E, Sabbagh C, Vandervoort J, Tanis PJ, Vanbiervliet G, Arezzo A. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2020. Endoscopy. 2020;52:389-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 199] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 56. | Vogel JD, Felder SI, Bhama AR, Hawkins AT, Langenfeld SJ, Shaffer VO, Thorsen AJ, Weiser MR, Chang GJ, Lightner AL, Feingold DL, Paquette IM. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Colon Cancer. Dis Colon Rectum. 2022;65:148-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 190] [Article Influence: 63.3] [Reference Citation Analysis (1)] |
| 57. | Rodrigues-Pinto E, Morais R, Coelho C, Pereira P, Repici A, Macedo G. Bridge-to-surgery versus emergency surgery in the management of left-sided acute malignant colorectal obstruction - Efficacy, safety and long-term outcomes. Dig Liver Dis. 2019;51:364-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 58. | Aicher BO, Betancourt-Ramirez A, Grossman MD, Heise H, Schroeppel TJ, Hernandez MC, Zielinski MD, Kongkaewpaisan N, Kaafarani HMA, Wagner A, Grabo D, Scott M, Peck G, Chang G, Matsushima K, Cullinane DC, Cullinane LM, Stocker B, Posluszny J, Simonoski UJ, Catalano RD, Vasileiou G, Yeh DD, Agrawal V, Truitt MS, Pickett M, Dultz L, Muller A, Ong AW, San Roman JL, Barth N, Fackelmayer O, Velopulos CG, Hendrix C, Estroff JM, Gambhir S, Nahmias J, Jeyamurugan K, Bugaev N, O'Meara L, Kufera J, Diaz JJ, Bruns BR. Validation of the American Association for the Surgery of Trauma Emergency General Surgery Grading System for Colorectal Resection: An EAST Multicenter Study. Am Surg. 2022;88:953-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 59. | Taylor JC, Iversen LH, Burke D, Finan PJ, Iles MM, Morris EJA, Quirke P; YCR BCIP Study Group. Differences in the management of patients requiring an emergency resection for colonic cancer in two European populations. BJS Open. 2022;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 60. | Zattoni D, Christoforidis D. How best to palliate and treat emergency conditions in geriatric patients with colorectal cancer. Eur J Surg Oncol. 2020;46:369-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 61. | Veld JV, Amelung FJ, Borstlap WAA, Eise van Halsema E, Consten ECJ, Siersema PD, Ter Borg F, Silvester van der Zaag E, Fockens P, Bemelman WA, Elise van Hooft J, Tanis PJ; Dutch Snapshot Research Group. Changes in Management of Left-Sided Obstructive Colon Cancer: National Practice and Guideline Implementation. J Natl Compr Canc Netw. 2019;17:1512-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 62. | de Roos MAJ, Hugen N, Hazebroek EJ, Spillenaar Bilgen EJ. Delayed surgical resection of primary left-sided obstructing colon cancer is associated with improved short- and long-term outcomes. J Surg Oncol. 2021;124:1146-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 63. | Angulo McGrath I, Martínez Burgos M, Bracho González M, Durán Campos A, Marín García D, Vázquez Pedreño L, Jiménez Pérez M. Experience in the treatment of obstructive colorectal cancer with self-expandable colon prosthesis in a tertiary hospital. Rev Esp Enferm Dig. 2022;114:626-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 64. | Kim M, Rai M, Teshima C. Interventional Endoscopy for Palliation of Luminal Gastrointestinal Obstructions in Management of Cancer: Practical Guide for Oncologists. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 65. | Morino M, Arezzo A, Farnesi F, Forcignanò E. Colonic Stenting in the Emergency Setting. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 66. | Alonso-Hernández N, Segura-Sampedro JJ, Soldevila Verdeguer CM, Ochogavía Seguí A, Olea Martinez-Mediero JM, Fernández Isart M, Gamundi Cuesta M, González-Argente XF. Results of a national survey on the use of stents for the treatment of colonic obstruction. Cir Esp (Engl Ed). 2020;98:533-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 67. | Young CJ, Zahid A. Randomized controlled trial of colonic stent insertion in non-curable large bowel obstruction: a post hoc cost analysis. Colorectal Dis. 2018;20:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 68. | Lim TZ, Tan KK. Endoscopic stenting in colorectal cancer. J Gastrointest Oncol. 2019;10:1171-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 69. | Ormando VM, Palma R, Fugazza A, Repici A. Colonic stents for malignant bowel obstruction: current status and future prospects. Expert Rev Med Devices. 2019;16:1053-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 70. | Wang Y, Hu H, Wang M, Han X, Zhang Q, Yu L, Chen Y, Wang G. Self-expanding metallic stent as a bridge to surgery versus emergency surgery for acute obstructive colorectal cancer: a retrospective study. Cancer Manag Res. 2019;11:2709-2718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 71. | Asbjarnardottir MG, Valsdottir EB, Sigurdsson HK, Moller PH. [Stenting for colorectal cancer obstruction in Icelandic patients]. Laeknabladid. 2020;106:569-573. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 72. | Liu JJ, Ma TH, Qin QY, Wang L. Stent placement followed by preoperative chemotherapy and elective surgery for acute malignant colorectal obstruction: Six cases of report. World J Gastrointest Oncol. 2019;11:264-269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 73. | Weston BR, Patel JM, Pande M, Lum PJ, Ross WA, Raju GS, Lynch PM, Coronel E, Ge PS, Lee JH. Efficacy of uncovered colonic stents for extrinsic versus intrinsic malignant large bowel obstruction. Surg Endosc. 2021;35:4511-4519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 74. | Yang K, Zhu YQ, Chen NW, Wang ZG, Cheng YS. Super-Flexible Through-the-Scope Self-Expandable Metallic Stent Insertion for the Management of Malignant Tortuous Hepatic or Splenic Flexure Colonic Obstruction. Chin Med J (Engl). 2018;131:1381-1384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 75. | Lim CH, McDonald NM, Freeman ML, Amateau SK. Percutaneous cecostomy with fully covered self-expandable metal stent for initial management of severe malignant colon obstruction. Endoscopy. 2017;49:E313-E315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 76. | Mashar M, Mashar R, Hajibandeh S. Uncovered versus covered stent in management of large bowel obstruction due to colorectal malignancy: a systematic review and meta-analysis. Int J Colorectal Dis. 2019;34:773-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 77. | Lee JS, Lee HS, Kim ES, Jung MK, Jung JT, Kim HG, Lee DW, Kim DJ, Lee YJ, Yang CH; Daegu-Gyeongbuk Gastrointestinal Study Group (DGSG). Comparison of different types of covered self-expandable metal stents for malignant colorectal obstruction. Surg Endosc. 2021;35:4124-4133. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 78. | Kwaan MR, Ren Y, Wu Y, Xirasagar S. Colonic Stent Use by Indication and Patient Outcomes: A Nationwide Inpatient Sample Study. J Surg Res. 2021;265:168-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 79. | Hsu J, Sevak S. Management of Malignant Large-Bowel Obstruction. Dis Colon Rectum. 2019;62:1028-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 80. | Donlon NE, Kelly ME, Narouz F, McCormick PH, Larkin JO, Mehigan BJ. Colonic stenting as a bridge to surgery in malignant large bowel obstruction: oncological outcomes. Int J Colorectal Dis. 2019;34:613-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 81. | Sasaki T, Yoshida S, Isayama H, Narita A, Yamada T, Enomoto T, Sumida Y, Kyo R, Kuwai T, Tomita M, Moroi R, Shimada M, Hirata N, Saida Y. Short-Term Outcomes of Colorectal Stenting Using a Low Axial Force Self-Expandable Metal Stent for Malignant Colorectal Obstruction: A Japanese Multicenter Prospective Study. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 82. | Mahfouz MF, Salama TMS, Afifi AH, Dabous HMK. Effectiveness and early postoperative outcomes of palliative endoluminal stenting versus Hartmann's procedure in acute malignant bowel obstruction in high-risk patients. Ann Coloproctol. 2022;38:141-145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 83. | Lee JH, Emelogu I, Kukreja K, Ali FS, Nogueras-Gonzalez G, Lum P, Coronel E, Ross W, Raju GS, Lynch P, Thirumurthi S, Stroehlein J, Wang Y, You YN, Weston B. Safety and efficacy of metal stents for malignant colonic obstruction in patients treated with bevacizumab. Gastrointest Endosc. 2019;90:116-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 84. | Seoane Urgorri A, Saperas E, O'Callaghan Castella E, Pera Román M, Raga Gil A, Riu Pons F, Barranco Priego L, Dedeu Cusco JM, Pantaleón Sánchez M, Bessa Caserras X, Álvarez-González MA. Colonic stent vs surgical resection of the primary tumor. Effect on survival from stage-IV obstructive colorectal cancer. Rev Esp Enferm Dig. 2020;112:694-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 85. | Balciscueta I, Balciscueta Z, Uribe N, García-Granero E. Perineural invasion is increased in patients receiving colonic stenting as a bridge to surgery: a systematic review and meta-analysis. Tech Coloproctol. 2021;25:167-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 86. | Spannenburg L, Sanchez Gonzalez M, Brooks A, Wei S, Li X, Liang X, Gao W, Wang H. Surgical outcomes of colonic stents as a bridge to surgery versus emergency surgery for malignant colorectal obstruction: A systematic review and meta-analysis of high quality prospective and randomised controlled trials. Eur J Surg Oncol. 2020;46:1404-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 87. | Kuwai T, Tamaru Y, Kusunoki R, Yoshida S, Matsuzawa T, Isayama H, Maetani I, Shimada M, Yamada T, Saito S, Tomita M, Koizumi K, Shiratori T, Enomoto T, Saida Y. Long-term outcomes of standardized colonic stenting using WallFlex as a bridge to surgery: Multicenter prospective cohort study. Dig Endosc. 2022;34:840-849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 88. | Axmarker T, Leffler M, Lepsenyi M, Thorlacius H, Syk I. Long-term survival after self-expanding metallic stent or stoma decompression as bridge to surgery in acute malignant large bowel obstruction. BJS Open. 2021;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 89. | Matsuda A, Yamada T, Matsumoto S, Sakurazawa N, Kawano Y, Sekiguchi K, Matsutani T, Miyashita M, Yoshida H. Short-term outcomes of a self-expandable metallic stent as a bridge to surgery vs. a transanal decompression tube for malignant large-bowel obstruction: a meta-analysis. Surg Today. 2019;49:728-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 90. | Mege D, Manceau G, Bridoux V, Voron T, Sabbagh C, Lakkis Z, Venara A, Ouaissi M, Denost Q, Kepenekian V, Sielezneff I, Karoui M; AFC (French Surgical Association) Working Group. Surgical management of obstructive left colon cancer at a national level: Results of a multicentre study of the French Surgical Association in 1500 patients. J Visc Surg. 2019;156:197-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 91. | Bertelsen CA, Elfeki H, Neuenschwander AU, Laurberg S, Kristensen B, Emmertsen KJ. The risk of long-term bowel dysfunction after resection for sigmoid adenocarcinoma: a cross-sectional survey comparing complete mesocolic excision with conventional surgery. Colorectal Dis. 2018;20:O256-O266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 92. | Trigui A, Rejab H, Akrout A, Harbi H, Kachaou A, Fendri S, Frikha MF, Mzali R. [Comparison between endoscopic stenting and colostomy in the management of obstructing cancer of the left colon: Literature review]. Presse Med. 2019;48:173-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 93. | Gavriilidis P, de'Angelis N, Wheeler J, Askari A, Di Saverio S, Davies JR. Diversion, resection, or stenting as a bridge to surgery for acute neoplastic left-sided colonic obstruction: a systematic review and network meta-analysis of studies with curative intent. Ann R Coll Surg Engl. 2021;103:235-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 94. | Tabusa H, Blazeby JM, Blencowe N, Callaway M, Daniels IR, Gunning A, Hollingworth W, McNair AG, Murkin C, Pinkney TD, Rogers CA, Smart NJ, Reeves BC. Protocol for the UK cohort study to investigate the prevention of parastomal hernia (the CIPHER study). Colorectal Dis. 2021;23:1900-1908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 95. | Aubert M, Mege D, Manceau G, Bridoux V, Lakkis Z, Venara A, Voron T, Abdalla S, Beyer-Berjot L, Sielezneff I, Sabbagh C, Karoui M; AFC (French Surgical Association) Working Group. Impact of hospital volume on outcomes after emergency management of obstructive colon cancer: a nationwide study of 1957 patients. Int J Colorectal Dis. 2020;35:1865-1874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 96. | Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer: A propensity score matching analysis. Medicine (Baltimore). 2018;97:e12348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 97. | Colás-Ruiz E, Del-Moral-Luque JA, Gil-Yonte P, Fernández-Cebrián JM, Alonso-García M, Villar-Del-Campo MC, Durán-Poveda M, Rodríguez-Caravaca G. Incidence of surgical site infection and risk factors in rectal surgery: A prospective cohort study. Cir Esp (Engl Ed). 2018;96:640-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 98. | Chen PJ, Wang L, Peng YF, Chen N, Wu AW. Surgical intervention for malignant bowel obstruction caused by gastrointestinal malignancies. World J Gastrointest Oncol. 2020;12:323-331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 99. | Danzi M, Grimaldi L, De Capua M, Tammaro N, Danzi R, Sivero L. Obstructing left sided colorectal cancer. A retrospective single Center study. Ann Ital Chir. 2019;90:121-126. [PubMed] |
| 100. | Malakorn S, Stein SL, Lee JH, You YN. Urgent Management of Obstructing Colorectal Cancer: Divert, Stent, or Resect? J Gastrointest Surg. 2019;23:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 101. | Boeding JRE, Ramphal W, Rijken AM, Crolla RMPH, Verhoef C, Gobardhan PD, Schreinemakers JMJ. A Systematic Review Comparing Emergency Resection and Staged Treatment for Curable Obstructing Right-Sided Colon Cancer. Ann Surg Oncol. 2021;28:3545-3555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 102. | Capona R, Hassab T, Sapci I, Aiello A, Liska D, Holubar S, Lightner AL, Steele SR, Valente MA. Surgical intervention for mechanical large bowel obstruction at a tertiary hospital: Which patients receive a stoma and how often are they reversed? Am J Surg. 2021;221:594-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 103. | Kondo A, Okano K, Kumamoto K, Kobara H, Nagahara T, Wato M, Shibatoge M, Minato T, Masaki T, Suzuki Y; Kagawa Gastroenterology Forum. Surgical management and outcomes of obstructive colorectal cancer in elderly patients: A multi-institutional retrospective study. Surgery. 2022;172:60-68. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 104. | Podda M, Di Saverio S, Davies RJ, Atzeni J, Balestra F, Virdis F, Reccia I, Jayant K, Agresta F, Pisanu A. Prophylactic intra-abdominal drainage following colorectal anastomoses. A systematic review and meta-analysis of randomized controlled trials. Am J Surg. 2020;219:164-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 105. | Manceau G, Mege D, Bridoux V, Lakkis Z, Venara A, Voron T, Sielezneff I, Karoui M; French Surgical Association Working Group. Emergency Surgery for Obstructive Colon Cancer in Elderly Patients: Results of a Multicentric Cohort of the French National Surgical Association. Dis Colon Rectum. 2019;62:941-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 106. | Kartal K, Citgez B, Koksal MH, Besler E, Akgun İE, Mihmanli M. Colostomy reversal after a Hartmann's procedure Effects of experience on mortality and morbidity. Ann Ital Chir. 2019;90:539-544. [PubMed] |
| 107. | Söderbäck H, Gunnarsson U, Martling A, Hellman P, Sandblom G. Incidence of wound dehiscence after colorectal cancer surgery: results from a national population-based register for colorectal cancer. Int J Colorectal Dis. 2019;34:1757-1762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 108. | Veld JV, Amelung FJ, Borstlap WAA, van Halsema EE, Consten ECJ, Dekker JWT, Siersema PD, Ter Borg F, van der Zaag ES, Fockens P, Bemelman WA, de Wilt JHW, van Hooft JE, Tanis PJ; Dutch Snapshot Research Group. Decompressing Stoma a s Bridge to Elective Surgery is an Effective Strategy for Left-sided Obstructive Colon Cancer: A National, Propensity-score Matched Study. Ann Surg. 2020;272:738-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 109. | Manceau G, Voron T, Mege D, Bridoux V, Lakkis Z, Venara A, Beyer-Berjot L, Abdalla S, Sielezneff I, Lefèvre JH, Karoui M; AFC (French Surgical Association) Working Group. Prognostic factors and patterns of recurrence after emergency management for obstructing colon cancer: multivariate analysis from a series of 2120 patients. Langenbecks Arch Surg. 2019;404:717-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 110. | Yuan X, Liu W, Ye L, Wu M, Hu B. Combination of endoscopic incision and balloon dilation for treatment of a completely obstructed anastomotic stenosis following colorectal resection: A case report. Medicine (Baltimore). 2019;98:e16292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 111. | Lavanchy JL, Vaisnora L, Haltmeier T, Zlobec I, Brügger LE, Candinas D, Schnüriger B. Oncologic long-term outcomes of emergency versus elective resection for colorectal cancer. Int J Colorectal Dis. 2019;34:2091-2099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 112. | Mihailov R, Firescu D, Constantin GB, Mihailov OM, Hoara P, Birla R, Patrascu T, Panaitescu E. Mortality Risk Stratification in Emergency Surgery for Obstructive Colon Cancer-External Validation of International Scores, American College of Surgeons National Surgical Quality Improvement Program Surgical Risk Calculator (SRC), and the Dedicated Score of French Surgical Association (AFC/OCC Score). Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 113. | Genser L, Manceau G, Mege D, Bridoux V, Lakkis Z, Venara A, Voron T, Bege T, Sielezneff I, Karoui M; on behalf of the AFC (French Surgical Association) Working Group. 30-Day Postoperative Morbidity of Emergency Surgery for Obstructive Right- and Left-Sided Colon Cancer in Obese Patients: A Multicenter Cohort Study of the French Surgical Association. Dig Surg. 2020;37:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 114. | Quintana JM, Anton-Ladislao A, Lázaro S, Gonzalez N, Bare M, Fernandez-de-Larrea N, Redondo M, Escobar A, Sarasqueta C, Garcia-Gutierrez S, Aguirre U; REDISSEC-CARESS/CCR group. Effect of comorbidities on long-term outcomes of colorectal cancer patients. Eur J Cancer Care (Engl). 2022;31:e13561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 115. | Abu Baker F, Taher R, Ganayem M, Mari A, Oren G, Kopelman Y. Obstructive colon cancers at endoscopy are associated with advanced tumor stage and poor patient outcome. A retrospective study on 398 patients. Eur J Gastroenterol Hepatol. 2021;33:50-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 116. | Sato R, Oikawa M, Kakita T, Okada T, Abe T, Yazawa T, Tsuchiya H, Akazawa N, Sato M, Ohira T, Harada Y, Okano H, Ito K, Ohuchi N, Tsuchiya T. Preoperative change of modified Glasgow prognostic score after stenting predicts the long-term outcomes of obstructive colorectal cancer. Surg Today. 2020;50:232-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |