Published online Feb 15, 2024. doi: 10.4251/wjgo.v16.i2.543
Peer-review started: September 24, 2023
First decision: December 12, 2023
Revised: December 13, 2023
Accepted: January 11, 2024
Article in press: January 11, 2024
Published online: February 15, 2024
Processing time: 131 Days and 2.9 Hours
Solitary fibrous tumors (SFT) are rare spindle cell tumors that are usually benign. A total of 10 cases of SFTs in the upper esophagus have ever been reported. Here, we report the anesthetic management of a patient with a large isolated fibrous tumor of the upper esophagus compressing the tracheal membrane. We also provide a literature review of the current research.
We report the case of a 49 year old male with “cough aggravation and wheezing after exercise”, who underwent esophagectomy for a large isolated fibrous tumor compressing the tracheal membrane in the upper esophagus. We advise the use of a single-lumen tube with a blocker in patients with difficult airways to reduce the incidence of airway injury and fibrinoscopy at all stages of the perioperative period to guide airway management. This case study is the first report of the anesthetic management of a large, isolated fibrous tumor compressing the tracheal membrane in the upper esophagus.
This rare case emphasizes the importance of perioperative management of anesthesia in patients with large isolated fibrous tumors of the upper esophagus that compress the tracheal membrane. The use of blocker reduce the incidence of airway injury and fibrinoscopy at the perioperative period to guide airway mana
Core Tip: Tracheobronchial injury is rare, but the mortality rate is high. A patient with large isolated fibrous tumor in the upper esophagus are at a high risk of airway injury during surgery due to the compression of the tracheal membrane, poor airway expandability. Our management experience shows that airway tools are preferred to single-lumen tubes with blockers for patients with difficult airways, which reduces the incidence of airway injury. Perioperative application of fibrinoscopy is necessary to monitor airway safety in real time and close cooperation with the operator reduces airway injury.
- Citation: Yu JJ, Pei HS, Meng Y. Large isolated fibrous tumors in the upper esophagus: A case report. World J Gastrointest Oncol 2024; 16(2): 543-549
- URL: https://www.wjgnet.com/1948-5204/full/v16/i2/543.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v16.i2.543
Tracheobronchial injury (TBI) is rare but has a mortality rate and can lead to subcutaneous emphysema, mediastinal emphysema, pneumothorax, dyspnea, hemoptysis, pericardial pneumothorax, and shock. The causes of TBI include traumatic, medical, and inhalation injuries. Medically induced injuries mainly occur during surgical procedures, tracheal intubation, and bronchoscopy. Tracheoscopy is a key method for confirming the diagnosis of TBI and aiding in airway management. We provide a rare report of a patient with a large isolated fibrous tumor in the upper esophagus who underwent resection of the esophageal mass and was at high risk of airway injury due to the hardness of the tumor, compression of the tracheal membrane, and poor airway expandability. We provide evidence that airway tools reduce the incidence of airway injuries compared to single-lumen tubes with blockers. In addition, we describe the perioperative application of fibrinoscopy for patient monitoring of airway safety in real time. This report also provides new ideas for the anesthetic management of patients with giant isolated fibrous tumors of the upper esophagus.
A 49-year-old male patient (176 cm and 82 kg) complained of a worsening cough and wheezing after exercising for > 1 month.
The patient complained of coughing and wheezing for more than a month, with no discomfort after exercise.
The patient had no history of hypertension, diabetes mellitus, coronary heart disease.
There was no family history of hereditary diseases.
The patient had a temperature of 36.4 °C, a heart rate of 85 beats/min, a respiratory rate of 18 breaths/min, and a blood pressure (BP) of 123/83 mm Hg. The patient was conscious and physical examination was unremarkable. The breath rate in both lungs was slightly low and no rales were heard. There was no elevation in the precordial region, rhythm regulation, and no additional heart or pericardial friction sounds were heard.
Laboratory results revealed that the hemoglobin test was 108.0 g/L and the hematocrit (HCT) test was 34%. Other tests including blood biochemistry and coagulation function revealed no significant abnormalities.
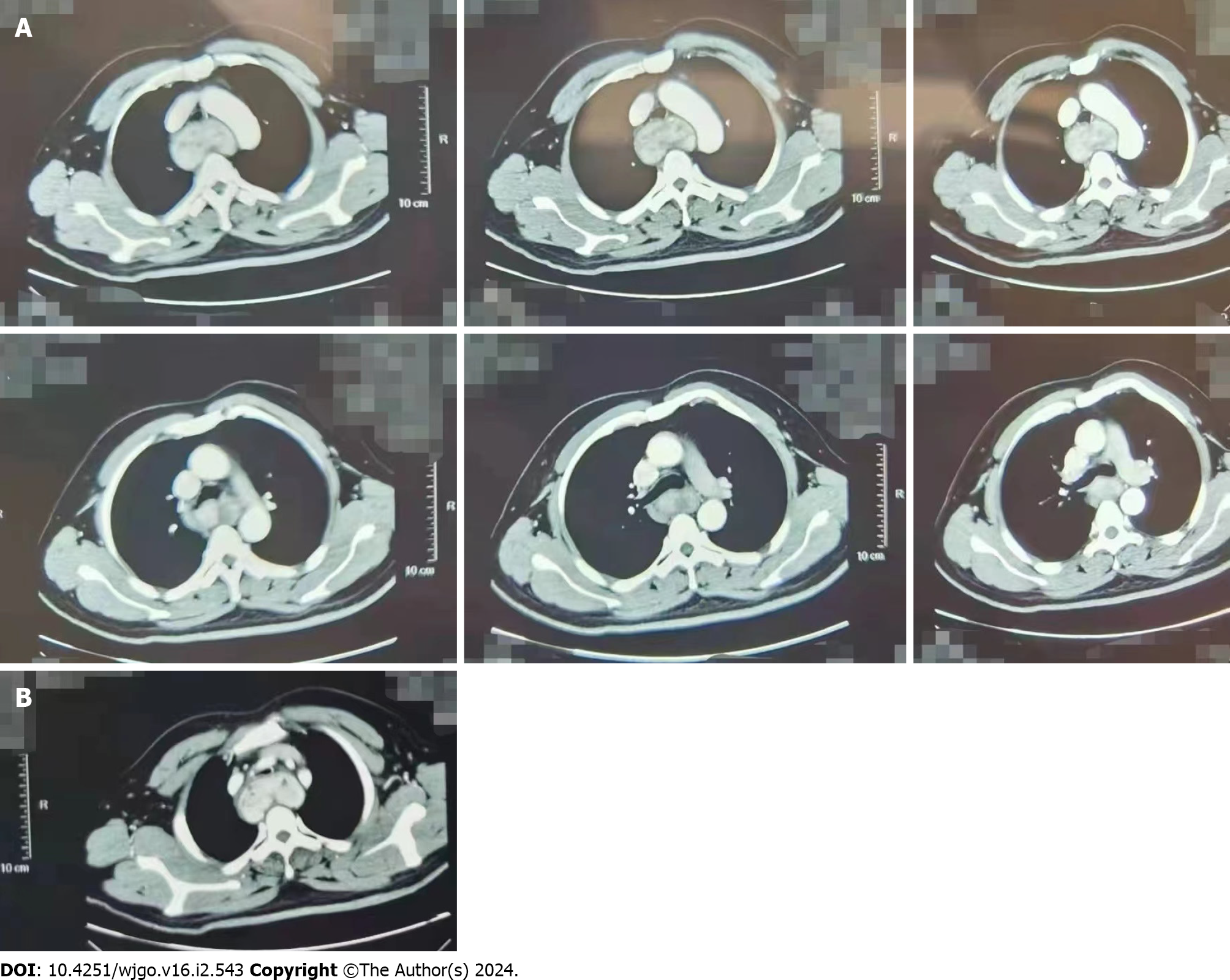
A chest enhancement computed tomography (CT) scan revealed a rich blood supply occupying the lesion in the posterior superior mediastinal esophageal travel area. This suggested a smooth muscle tumor in the submucosal layer of the esophageal lesion. The mid-esophagus was abnormally strengthened, and the trachea was narrowed by compression. The CT of the neck showed a rich blood supply occupying the lesion in the esophageal travel area of the posterior superior mediastinum, which was diagnosed as an extraesophageal and intertracheal tumor (Figure 1).
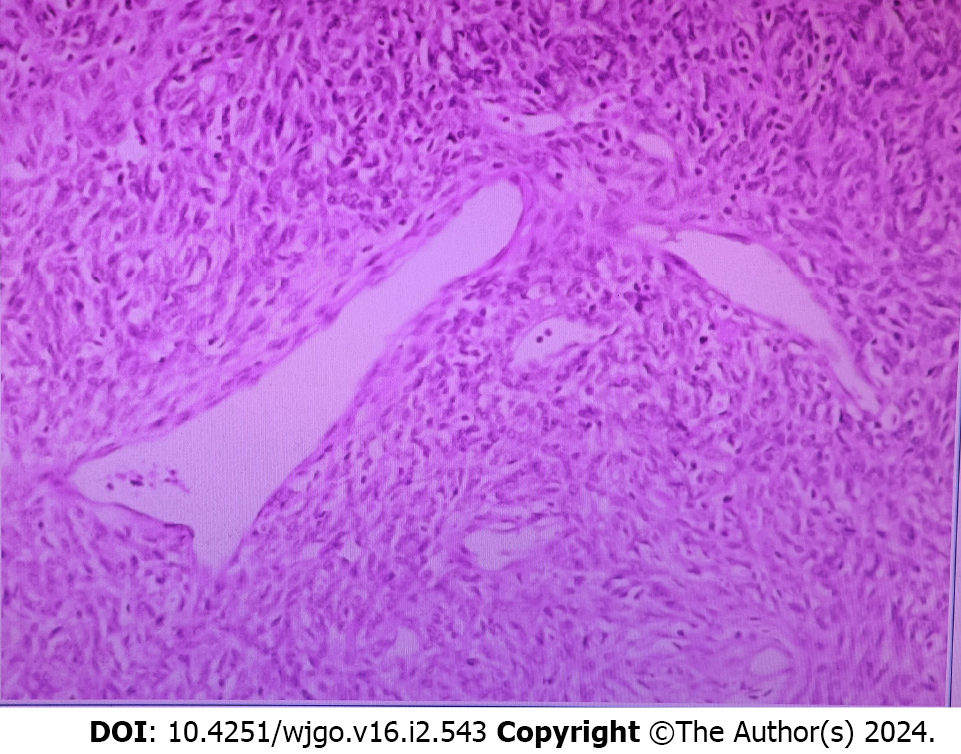
The patient was finally diagnosed with an isolated fibrous tumor of the upper esophagus. The postoperative pathological diagnosis was consistent with that of an isolated fibrous tumor (Figure 2). The tumor measured 7 cm × 6 cm × 3 cm.
After admission, venous access to the left upper extremity was opened, and BP, electrocardiogram, SpO2, and bispectral index (BIS) were routinely monitored. The following measurements were obtained: BP: 140/75 mmHg; heart rate (HR): 100 beats/min; SpO2: 296%; and 96 BIS values. The left-hand Allen test was negative, invasive arterial manometry was performed by left radial artery puncture placement, and basal arterial blood gases were measured: FiO2: 0.21; PaO2: 89.9 mmHg; PaCO2: 41.4 mmHg; and HCT: 34.0%. To anesthetize the patient, oxygen was administered for 3 min with face mask denitrogenation, and sufentanil 30 μg, etomidate 18 mg, and rocuronium 50 mg were injected separately. In addition, a 7.5 mm single-lumen tracheal tube was inserted through the mouth 3 min later, with the tube fixed 22 cm from the incisor. Hand-controlled respiratory airway resistance was slightly high, and bilateral lung breathing sounds were heard on auscultation. The mechanical ventilation parameters were set as FiO2: 100%; tidal volume: 8 mL/kg; respiratory rate: 12-15 breaths/min; peak airway pressure: 24-26 mmHg; PETCO2: 32-37 mmHg. A double-lumen central venous catheter was inserted in the right internal jugular vein. After adequate aspiration, a 9F blocker was inserted through the single-lumen tracheal tube under the guidance of a 2.8 mm diameter positioned ciliofibroscope to block the right lung. An ultrasound-guided T6 paravertebral nerve block (20 mL of 0.18% bupivacaine) was performed after left lateral recumbency. Anesthesia was maintained with 0.05-0.20 μg/kg/min remifentanil by continuous intravenous pumping and 2%-3% sevoflurane by inhalation were used for static inhalation compound general anesthesia. Additional cisatracurium (3 mg) was added intermittently to maintain inotropic relaxation. The surgery was performed in the left lateral position via the right thorax. The right lung was blocked and the left single lung was ventilated. The respiratory parameters for single-lung ventilation were as follows: FiO2: 100%; tidal volume: 6 mL/kg; and respiratory rate: 13-15 breaths/min. Increased airway resistance after left lateral recumbency, with a peak airway pressure of 28-30 mmHg and PETCO2 of 38-47 mmHg was measured. When the tumor was removed from the right chest, the peak airway pressure rose to 40 mmHg, the ventilator alarmed, and mechanical ventilation was stopped immediately. He immediately com
The patient recovered well and was discharged without any abnormalities in postoperative routine blood and blood biochemistry indicators or respiratory complications. The postoperative pathological diagnosis was consistent with that of an isolated fibrous tumor (Figure 2). The tumor measured 7 cm × 6 cm × 3 cm. At the two-month postoperative follow-up, the patient had no respiratory complications.
This article reports on the esophageal mass resection of a patient with a large isolated fibrous tumor of the upper esophagus compressing the tracheal membrane. We also provide a summary of the current literature.
Solitary fibrous tumors (SFT) are rare, and mesenchymal tumors often originate from CD34-positive dendritic mesenchymal cells[1]. Only 10 cases have been reported to date[2-7]. SFTs are usually asymptomatic in the early stages; however, as the tumor grows, symptoms of pressure can appear at the corresponding site. Depending on the size and location of the tumor, symptoms such as dysphagia, cough, pain, dyspnea, and pulmonary osteoarthropathy[4,5] can present. Tumors located between the upper esophagus and the trachea present with varying degrees of dysphagia and respiratory symptoms as their size increases. Pathological examination is the gold standard for diagnosing SFT, which is usually defined by a well-defined round or ovoid mass with an intact envelope, some of which may be tipped, where the cut surface is greyish-white, tough, and elastic. Microscopically, the tumor cells are spindle-shaped with elongated nuclei, with no obvious heterogeneity, and rare nuclear division. The interstitial stroma is lax, with collagen fibers of varying thickness and morphology between the tumor cells. The interstitial vessels are abundant, with glassy changes in the vessel walls[4]. CT examination of the lungs is the most important and basic examination protocol for this tumor, which is usually a bounded clear mass, often consistent with skeletal muscle density and a significant blood supply with heterogeneous contrast enhancement[5]. CT plays an important role in diagnosis and treatment by determining which key structures are compressed (Figure 1) and what hemodynamic and airway consequences are expected during the perioperative period. Given that most SFTs exhibit benign biological behavior, the clinical management of esophageal SFTs is mainly based on radical surgical resection with endoscopic assistance, as reported in two cases[6,7], and supplemented by radiotherapy when necessary.
In this patient’s case, the tumor was located in the posterior superior mediastinum and the airway was narrowed due to compression of the tracheal membrane (as seen on the CT) via the large, hard, tumor that had a rich blood supply. Tumors located in the upper and middle esophagus occur on the right side of the chest, whereas those in the lower part of the esophagus occur on the left side of the chest[6]. The choice of airway tools for single-lung ventilation is influenced by different procedures, softness of the tumor tissue, and the degree of tracheal membrane compression. Preoperatively, the patient’s cardiopulmonary function and airway status should be evaluated, the anesthetic plan and single-lung ventilation airway tools should be carefully selected, and a contingency plan should be prepared. Intraoperatively, close attention should be paid to the compression of the airway by the operator. Emphasis should be placed on tracheal intubation under fibrinoscopic guidance, real-time attention to airway patency, and detection of tracheal membrane integrity during the perioperative period using fibrinoscopy. Airway integrity should be tested again before extubation at the end of the operation, and choking should be avoided during the awakening period, and airway integrity should be tested again before extubation.
One-lung ventilation is a key technique for ensuring smooth performance of thoracic surgery. Available airway tools include double-lumen endobronchial tubes, bronchial blockers (BB), and single-lumen bronchial tubes. The single-lumen bronchial tube needs to be inserted into one side of the bronchus, which makes it difficult to ventilate the operated side of the lung. There are fewer models of bronchial tubes and difficulties in model selection, so they are rarely used clinically. The double-lumen bronchial catheter is the most commonly used clinical airway tool for single-lung ventilation; however, as the double-lumen bronchial catheter is thicker and stiffer than BB, there is a potential for airway injury during tracheal intubation and postoperative soreness in the throat is significantly higher than that of BB[8-10]. The BB is easy to place, faster, and can also achieve single-lung ventilation, especially for patients with difficult intubation[9]. In addition, postoperative single-lumen tubes can be retained to avoid the risk of postoperative tube replacement, and intraoperative position change is required several times to avoid catheter displacement, to reduce the friction between the catheter and trachea, and reduce the incidence of postoperative airway injury[10].
Studies have shown that the incidence of tracheal injury due to endotracheal intubation is 0.005%, with an increased incidence of 0.05%-0.19% when a double-lumen tube is inserted[11]. Tracheal injury after intubation usually occurs as an intermediate laceration in the middle third of the tracheal membrane[12], which can extend to the main bronchus. TBI can be caused by esophageal, thyroid, or rigid bronchoscopy. If the trachea is injured during the procedure, the tracheal tube obscuring the tracheal laceration may result in a delayed onset of tracheal injury symptoms. Bronchoscopy is a key method for confirming the diagnosis of TBI and helping manage the airway.
In patients with hard tumors, tracheal membrane compression, and poor airway expandability, the use of a double-lumen tube increases the risk of airway injury or failed intubation; therefore, the use of a thin, reinforced wire single-lumen tube combined with a blocker is recommended. A single-lumen tube was inserted under the guidance of a fibrinoscope in a position horizontal to the lower part of the tumor to prevent intraoperative airway obstruction. Before extubation at the end of the operation, fibrinoscopy was routinely performed to check airway integrity and avoid serious respiratory complications.
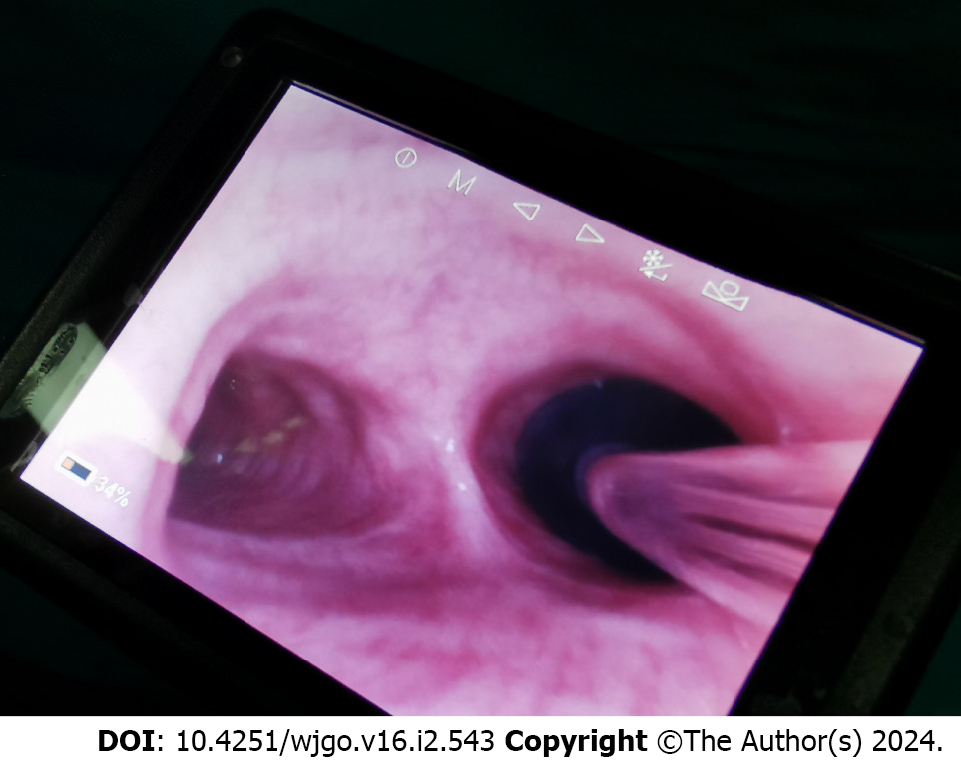
In this case, an isolated fibrous tumor of the upper esophagus was operated in the left lateral position via the right chest. The tumor was hard and located between the outer esophagus and the tracheal membrane, resulting in narrowing of the upper tracheal segment under pressure and poor expandability, so the airway instrument was chosen to be a 7.5 mm reinforced wire single-lumen tube combined with a blocker for left one-lung ventilation (Figure 3). The conventional single-lumen tracheal intubation was performed in the horizontal position with the conventional intubation depth, the peak airway pressure was slightly higher, and breath sounds could be heard in both lungs on auscultation. The peak airway pressure increased after left lateral recumbency, and the peak airway pressure suddenly increased when the tumor was free through the right chest. The airway was occluded and the cilio-scope could not pass through. Immediately checking the operating field, it was found that the assistant was pulling the tumor hard to the right in order to provide sufficient space for the operator to operate, and for this reason, it was considered that the surgical operation caused further pressure on the tracheal membrane. Immediately, the assistant was asked to pull the tumor in the opposite direction, that is, the lower left side, to reduce the pressure on the tracheal membrane, and the airway was restored to patency instantly. Afterwards, a single-lumen tracheal tube was inserted through the lower edge of the tumor under the guidance of fibrinoscopy, and no further airway obstruction occurred, and the operation was carried out smoothly. After the operation, the single-lumen catheter was retracted to the original position, and the integrity of the trachea was checked again by ciliofibroscopy, and there was no damage to the tracheal membrane.
In the present case, the successful application of a fibrinoscopy-guided single-lumen tube with a blocker ensured perioperative safety and provided individualized and precise medical treatment to avoid perioperative airway complications. This case reminds us of the need for a detailed preoperative history and reasonable selection of single-lung ventilation airway tools based on the tumor site, size, texture, airway compression site, degree of airway stenosis, and airway expandability, as shown on CT (Figures 1 and 3). The airway safety is monitored in real time with the application of ciliofibroscopy in the following four stages: for tracheal intubation, the single-lumen tracheal tube needs to be inserted below the tumor under ciliofibroscopic guidance; for BB placement, the BB needs to be inserted to the appropriate position of the target bronchus under ciliofibroscopic guidance; after complete resection of the mass, the single-lumen tube needs to be retracted above the mass and the airway integrity needs to be checked via ciliofibroscopy; before extubation, avoidance of Before extubation, avoid choking and check the airway integrity again by fibrinoscopy. In addition, preoperative and intraoperative communication with the operator is required to reduce the airway injury caused by the surgical operation (Table 1).
| Item | Timeline | |
| Preoperative | 1 | Cough worsened and wheezing after exercise for more than 1 month |
| 2 | No previous history of hypertension, diabetes, or coronary artery disease | |
| 3 | Enhanced CT of the chest and CT of the neck showed a rich blood supply occupying lesion in the esophageal travel area of the posterior superior mediastinum, considering an extraesophageal and intertracheal tumor lesion | |
| 4 | The surgery was performed under general anesthesia with static suction | |
| Perioperative | 5 | After admission, the left upper extremity venous access was opened and BP, ECG, SpO2, and BIS were routinely monitored |
| 6 | Invasive BP was monitored and arterial blood gas analysis was conducted | |
| 7 | Induction of conventional anesthesia; Maintenance of anesthesia was performed by static inhalation compound general anesthesia | |
| 8 | Airway tool of choice: Single-lumen tube with blocker. Single-lumen tube with blocker inserted under fibrinoscopic guidance | |
| 9 | During the free exploration of the tumor, the airway resistance increased abruptly, and emergency fibrinoscopy was performed. The operator adjusted the position of the tumor to restore airway patency and advanced the single-lumen tube under fibrinoscopic guidance to below the tumor | |
| 10 | Intraoperative, postoperative and before extubation, fibrinoscopy was used to detect an intact and uninjured airway | |
| 11 | After the operation, the vital signs were stable and there were no respiratory complications. He was returned to the ward | |
| Postoperative | 12 | Vital signs were stable upon return to the room, with no respiratory complications |
| 13 | The patient recovered well and was successfully discharged from the hospital | |
| 14 | At the two-month postoperative follow-up, the patient had no respiratory complications | |
Anesthetic management of patients with large isolated fibrous tumors in the upper esophagus compressing the tracheal membrane is rare and unique. The application of ciliofibroscopy at all stages of the perioperative period can be used to guide airway management and reduce airway complications. Anesthesiologists should develop a strict anesthetic plan, a procedure for using fibrinoscopy at each stage of the perioperative period, and pay close attention to airway injuries caused by surgical operations in order to optimize the perioperative management of patients and provide safer and more precise medical services.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kheiralla OAM, Saudi Arabia S-Editor: Lin C L-Editor: A P-Editor: Yuan YY
| 1. | Martin-Broto J, Mondaza-Hernandez JL, Moura DS, Hindi N. A Comprehensive Review on Solitary Fibrous Tumor: New Insights for New Horizons. Cancers (Basel). 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 95] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 2. | Zamora AK, Chopra S, Sahakian A, Kim AW. Not Just Your Ordinary Tumor: A Solitary Fibrous Tumor of the Esophagus. Semin Thorac Cardiovasc Surg. 2020;32:176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 3. | Yeung J, de Perrot M. Commentary: Solitary Fibrous Tumor of the Esophagus-Rare but With Typical Characteristics. Semin Thorac Cardiovasc Surg. 2020;32:179-180. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Yan Q, Yuan JP, Ren JQ. A case of isolated fibrous tumor of esophagus. Linchuang Yu Shiyan Binglixue Zazhi. 2020;875-876. [DOI] [Full Text] |
| 5. | Li H, Hu B, Li T, Jin M, Hao J. A rare case of giant solitary fibrous tumor of the esophagus. Ann Thorac Surg. 2009;88:2019-2021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Mubarak MF, Shah JN, Bolton JS, Bansal M, El Chafic AH. Endoscopic resection of a giant solitary fibrous tumor of the esophagus. VideoGIE. 2018;3:343-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Zhu XS, Dai YC, Chen ZX. Giant Solitary Fibrous Tumor of Esophagus Resected by Endoscopic Submucosal Dissection. Ann Thorac Surg. 2015;100:2340-2343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Zhao L, Zhang X, Gao C, He J, Han Z, Li L. A comparison of bronchial blocker under artificial pneumothorax and double-lumen endobronchial tube for lung isolation in thoracoscopic enucleation of oesophageal leiomyoma. J Cardiothorac Surg. 2021;16:322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | He WQ, Li YS, Zhang XH, Yi B, Lu KZ. Application of bronchial blocking catheter in combined thoracolaparoscopic radical esophagectomy for esophageal cancer. Disanjunyidaxue Xuebao. 2018;40:1579-1583. [DOI] [Full Text] |
| 10. | Zou GS, Yang J, Feng ZG. Double-lumen endotracheal tube versus bronchial blocker in one lung ventilation. Linchuang Mazuixue Zazhi. 2012;28:557-559. |
| 11. | Wanj JN, Wang KC, Huang HD, Bai C. Current status and outlook of diagnosis and treatment of tracheobronchial injury. Zhongguo Huxi Yu Weizhongjianhu Zazhi. 2021;20:219-223. |
| 12. | Boutros J, Marquette CH, Ichai C, Leroy S, Benzaquen J. Multidisciplinary management of tracheobronchial injury. Eur Respir Rev. 2022;31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |