Published online Nov 15, 2022. doi: 10.4251/wjgo.v14.i11.2288
Peer-review started: August 16, 2022
First decision: September 23, 2022
Revised: September 28, 2022
Accepted: October 17, 2022
Article in press: October 17, 2022
Published online: November 15, 2022
Processing time: 90 Days and 20.1 Hours
Inflammatory pseudotumor-like follicular dendritic cell sarcoma (IPT-like FDCS) is rare with a low malignant potential. Hepatic IPT-like FDCS has similar clinical features to hepatocellular carcinoma (HCC), making it extremely difficult to distinguish between them in clinical practice. We describe the case of a young female patient diagnosed with HCC before surgery, which was pathologically diagnosed as IPT-like FDCS after the left half of the liver was resected. During 6 mo of follow-up, the patient recovered well with no signs of recurrence or metastasis.
A 23-year-old female patient with a 2-year history of hepatitis B presented to the Affiliated Hospital of Guizhou Medical University. She was asymptomatic at presentation, and the findings from routine laboratory examinations were normal except for slightly elevated alpha-fetoprotein levels. However, ultrasonography revealed a 3-cm diameter mass in the left hepatic lobe, and abdominal contrast-enhanced computed tomography revealed that the tumor had asymmetrical enhancement during the arterial phase, which declined during the portal venous phase, and had a pseudo-capsule appearance. Based on the findings from clinical assessments and imaging, the patient was diagnosed with HCC, for which she was hospitalized and had undergone laparoscopic left hepatectomy. However, the tumor specimens submitted for pathological analyses revealed IPT-like FDCS. After surgical removal of the tumor, the patient recovered. In addition, the patient continued to recover well during 6 mo of follow-up.
Hepatic IPT-like FDCS is difficult to distinguish from HCC. Hepatectomy may provide beneficial outcomes in non-metastatic hepatic IPT-like FDCS.
Core Tip: Inflammatory pseudotumor-like follicular dendritic cell sarcoma (IPT-like FDCS) is a type of FDCS with low malignant potential. We investigated the clinical and pathological characteristics, diagnosis, and treatment in a 23-year-old woman diagnosed with hepatic IPT-like FDCS. She underwent laparoscopic left hepatectomy, with an uneventful postoperative course. It is difficult to distinguish hepatic IPT-like FDCS from hepatocellular carcinoma based on clinical features. Therefore, most patients with hepatic IPT-like FDCS are found after surgery. However, surgery may be the best treatment option for patients with hepatic IPT-like FDCS. At present, no abnormality has been found in the patient during the 6-mo follow-up.
- Citation: Fu LY, Jiang JL, Liu M, Li JJ, Liu KP, Zhu HT. Surgical treatment of liver inflammatory pseudotumor-like follicular dendritic cell sarcoma: A case report. World J Gastrointest Oncol 2022; 14(11): 2288-2294
- URL: https://www.wjgnet.com/1948-5204/full/v14/i11/2288.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v14.i11.2288
Follicular dendritic cell sarcoma (FDCS) is a rare tumor with nonspecific clinical features. FDCS cannot be diagnosed based on clinical findings alone; therefore, its diagnosis depends on pathological examinations of surgically resected tumor specimens. Pathologically, most FDCSs express at least two FDC markers, including CD21, CD35, and CNA-42. There are two morphologic variants of this tumor: Conventional and inflammatory pseudotumor (IPT)-like[1]. The etiology and pathogenesis of IPT-like FDCS are not clear. Its occurrence may coincide with Epstein-Barr virus (EBV) infection, because in cases with confirmed IPT-like FDCS, the positive rate of Epstein-Barr encoding region (EBER) through in situ hybridization was as high as 92.1%[2]. EBV-encoded small RNA exists in all tumor cells, and hybridization imprinting tests confirmed that the virus exists in the form of a monoclonal free body, suggesting that EBV infection occurred before FDC tumor proliferation. CD21, the receptor molecule expressed on the surface of FDC, is the receptor of EBV; therefore, scholars speculate that EBV plays an important role in tumor formation. IPT-like FDCS cells are irregularly arranged and IPT-like FDCS presents with lymphocytic infiltrate, with a positive in situ hybridization test for (EBV)-encoded RNA[3]. Most IPT-like FDCSs affect the liver and spleen. Herein, we report a rare case of a female patient with liver IPT-like FDCS in the context of hepatitis B virus infection. We investigated the clinical and pathological characteristics, diagnosis, and treatment of IPT-like FDCS.
A 23-year-old female patient with an underlying hepatitis B virus infection presented, with no symptoms, at the Affiliated Hospital of Guizhou Medical University.
She was asymptomatic.
She had received entecavir as treatment for her hepatitis B infection 2 years previously.
The patient had an unremarkable personal and family history.
There were no significant findings on initial physical examination.
Laboratory analyses provided the following findings: Hemoglobin, 134 g/L; white blood cell count, 5.23 × 109 cells/L; platelet count, 149 × 109 cells/L; red blood cell count, 4.50 × 109 cells/L; anti-HB test results, positive; serum levels of albumin, 50.40 g/L; aspartate aminotransferase level, 39.50 U/L; alanine aminotransferase level, 23.80 U/L; alkaline phosphatase level, 80 U/L; total bilirubin level, 15.40 μmol/L; direct bilirubin level, 5.20 μmol/L; total bilirubin level, 10.20 μmol/L; hepatitis B viral DNA, 2.35e+01 IU/mL (normal ≤ 10 UI/mL); and alpha-fetoprotein (AFP) level, 12.31 ng/mL (normal = 0.00–7.00 ng/mL).
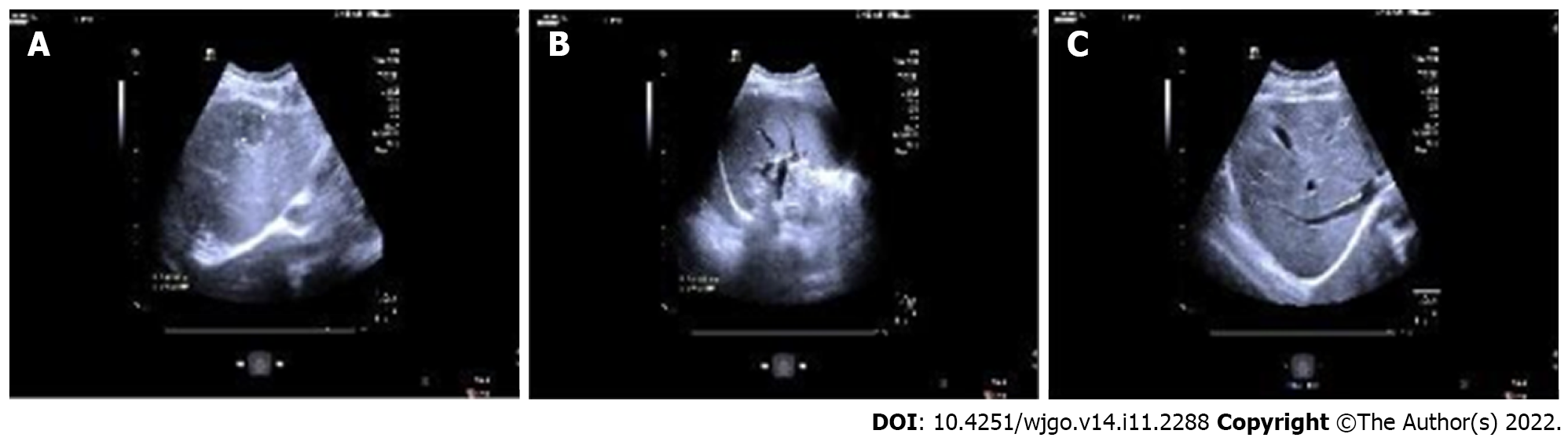
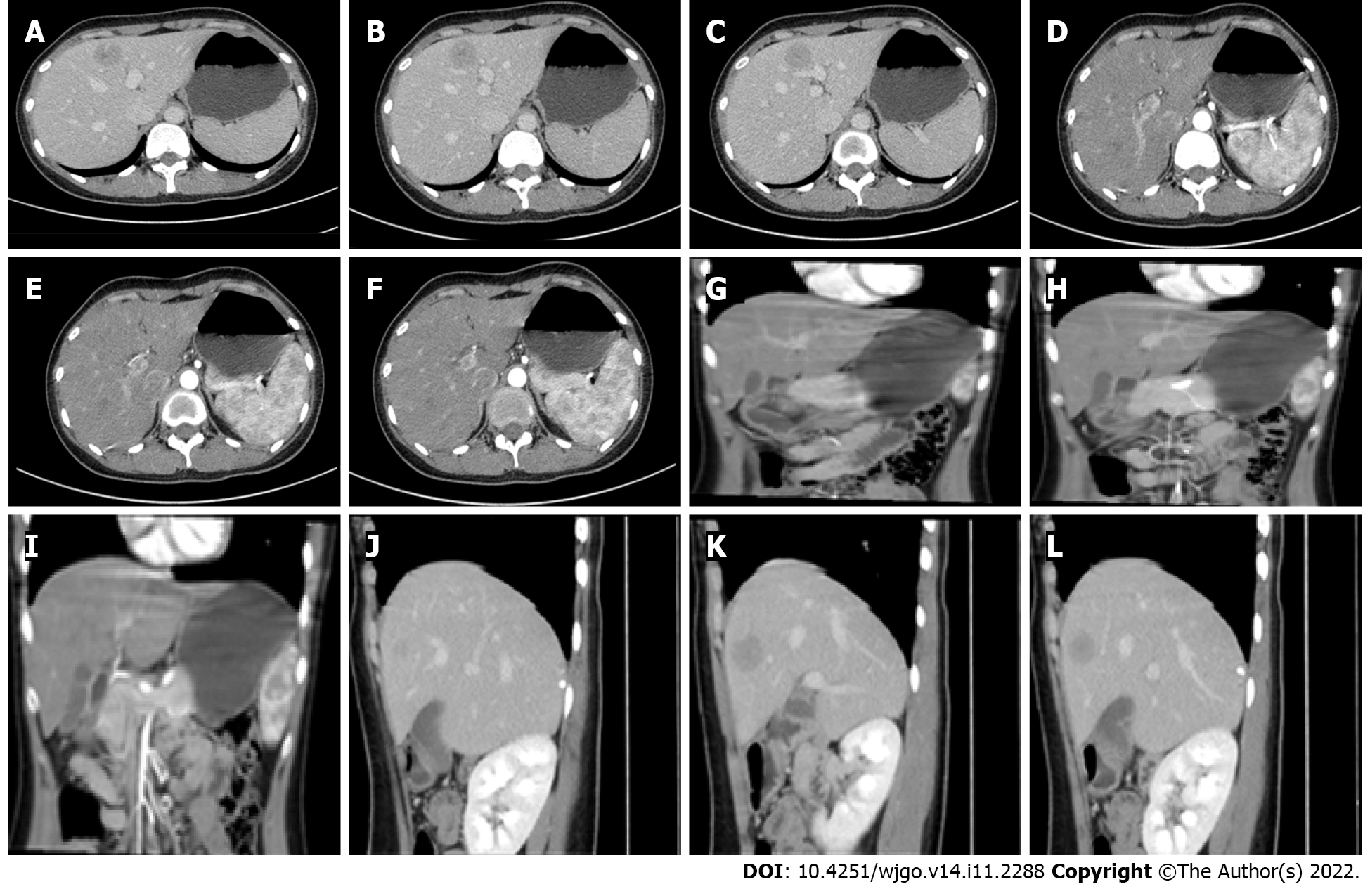
Ultrasonography revealed a 3-cm diameter mass in the left hepatic lobe (Figure 1), necessitating the performance of abdominal contrast-enhanced computed tomography (CT). CT showed asymmetrical tumor enhancement during the arterial phase; however, the enhancement declined during the portal venous phase, and the tumor had a pseudo-capsule appearance (Figure 2).
We initially diagnosed the disease as hepatocellular carcinoma (HCC) based on the findings from clinical, laboratory, and imaging assessments.
After discussion with the radiologist, early hepatocellular carcinoma was highly suspected according to the imaging signs and clinical manifestations. There was no other adjuvant treatment for the patient according to the preoperative comprehensive evaluation. Therefore, the patient underwent laparoscopic left hepatectomy.
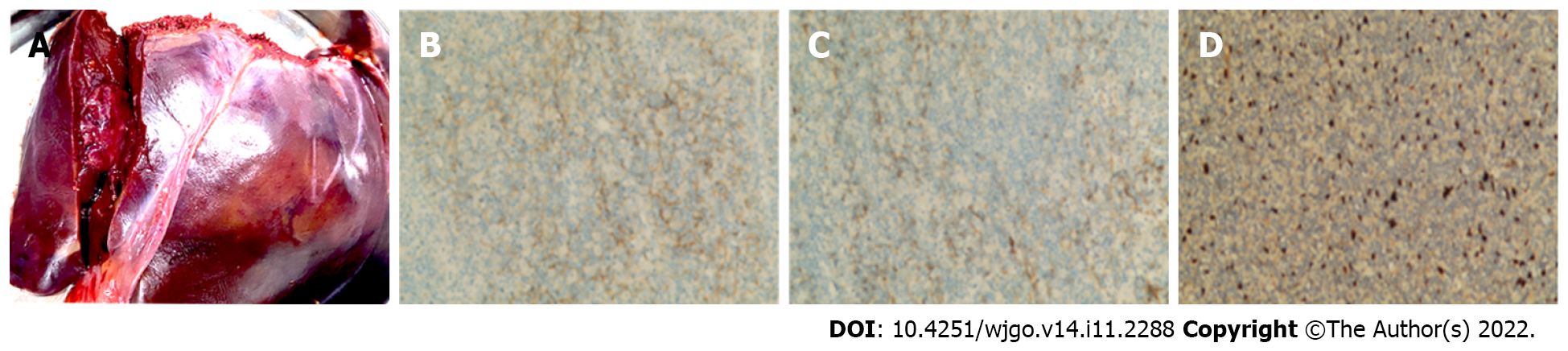
Postoperative pathological analysis showed a large number of medium to small lymphocytes distributed in the liver space-occupying lesion area, and an unequal number of spindle or epithelial cells, and histiocyte-like cells, were distributed alternately. Further, hepatic lobule structure was found in the surrounding liver tissue, some small lymphocytes had infiltrated the portal area, and a few small cells were found in the hepatic sinuses.
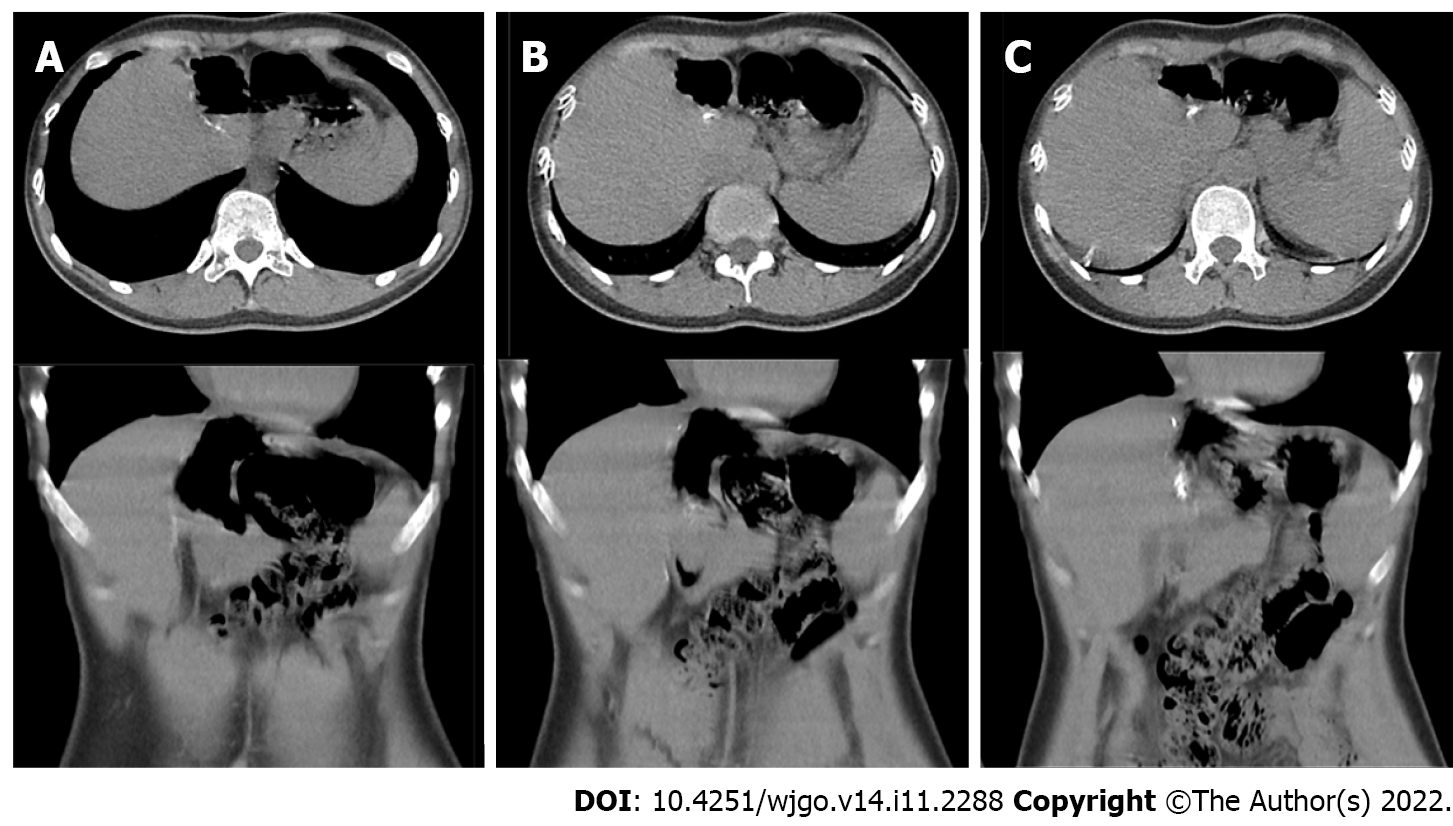
Immunohistochemical staining showed that the tumor specimen was positive for CD2, CD3, CD5, CD7, CD8, and TIA-1 in all lymphocytes. A portion of the tissue specimen was CD4 positive. Furthermore, positive expressions of CD21, CD35, Ki-67 (30%), and SMA were observed in a portion of the specimen with spindle-epithelioid tumor cells. In situ hybridization test was only positive for EBV-encoded RNA in spindle-epithelioid tumor cells (Figure 3). Based on these pathological findings, the patient was diagnosed with IPT-like FDCS. During the 6-mo postoperative follow-up period, the patient had no signs of recurrence or metastasis (Figure 4).
Although IPT-like FDCS is a special type of FDCS, it exhibits characteristic features comparable to those of conventional FDCS[4]. More than 60 cases of IPT-like FDCS have been reported in English literature, mainly located in the liver (more than 20 cases)[5-8] and spleen (more than 30 cases)[9-12], and to a lesser extent in the colon (6 cases)[13-15], lungs (1 case)[16], and pancreas (1 case)[17]. The tumor mainly occurs in middle-aged and elderly people, with a female-to-male ratio of 2.2:1, and a median age of 56.5 years[18].
To date, all reported patients with IPT-like FDCS in the liver presented with fever, jaundice, abdominal pain, and/or anemia as the initial clinical manifestations. In addition, other case reports highlighted paraneoplastic arthritis as an initial clinical manifestation[19,20]. However, the patient in the present case did not experience any clinical manifestations prior to the hospital visit, which shows the peculiarity of the disease in clinical practice. In our case, contrast-enhanced CT showed an asymmetrical tumor enhancement and decline during the arterial and portal venous phases, respectively, with a pseudo-capsule appearance of the tumor; these findings corroborated with those of previous studies[21].
Because the imaging manifestations of IPT-like FDCS of the liver are nonspecific, CT usually shows low-density nodule enhancement, which is characterized by non-uniform enhancement in the arterial phase and resolution in the delayed phase. Some highly differentiated HCCs can also show resolution in the delayed phase; therefore, hepatic inflammatory pseudotumor (HIPT)-like FDCS should also be differentiated from HCC with internal necrosis via imaging findings. HCC with internal necrosis often has peripheral structural invasion, accompanied by cirrhosis and portal hypertension, and may have tumor thrombus formation. HCC is the most common malignant tumor of the liver. The patient had chronic viral hepatitis, AFP elevation, and imaging findings suggestive of HCC. These signs are consistent with the general clinical manifestations of HCC. Therefore, we should pay attention to the possibility of this disease in addition to the huge mixed echo mass in the liver. If IPT-like FDCS is suspected, it is important to perform routine puncture biopsy. Puncture biopsy is a feasible preoperative diagnostic method for IPT-like FDCS, but many false negative cases have been encountered due to the smaller amount of obtained puncture tissue. Its definitive diagnosis mainly relies on immunohistochemical and in situ hybridization analyses of surgically obtained tumor specimens.
Apart from HCC, pathological analyses should be performed to distinguish HIPT-like FDCS from other diseases such as HIPT and primary liver lymphoma because the symptoms and imaging findings of HIPT are nonspecific. The histopathological characteristics of HIPT include the presence of inflammatory lesions consisting of diffused and dense hyalinized collagenosis with inflammatory cells, compact foamy histiocyte proliferation, as well as lymphocyte and plasma cell infiltration[22]. In primary liver lymphoma, clinical features are nonspecific as well, and histological analyses demonstrate infiltrations limited to the liver. Among the types of lymphoma, diffuse large B-cell lymphoma is the most common type noted[23,24]. HIPT-like FDCS shows a contrasting lymphocyte infiltration pattern compared with that of FDCS, immunohistochemical analyses show positive expression of one of the FDCS markers (CD21, CD35, CD23, or CNA42) in tumor cells, and in situ hybridization testing is positive for EBV-encoded RNA in spindle-epithelioid tumor cells. Clinicians can better diagnose HIPT-like FDCS via pathological examinations of surgically resected tissue specimens.
In summary, HIPT-like FDCS displays combined characteristics of chronic inflammation and malignant tumors on imaging. The final diagnosis is dependent on pathology, which shows that the tumor cells express CD21, CD23, CD35, SMA, and other markers, or do not express these antigens, but are EBER positive. HCC, HIPT, and primary liver lymphoma should be considered in the differential diagnosis.
In the treatment of HIPT-like FDCS, complete resection of tumor is the best treatment, but there is still dispute about whether conventional radiotherapy and chemotherapy are needed after surgery. Chemotherapy and/or radiotherapy can be used for patients with recurrence or surgery that cannot be cured[25-27]. The review found that the incidence of HIPT-like FDCS is very low, as are the recurrence and metastasis rate and mortality rate of previously reported liver cases; 4 cases recurred or metastasized, the recurrence rate was 11.8%, and the mortality rate was 2.9%. The remaining cases survived well[2]. In the present case, HIPT-like FDCS was found to be an indolent malignant tumor with no sign of relapse or metastasis noted during the follow-up.
HIPT-like FDCS is extremely difficult to distinguish from HCC due to their similar clinical features. In addition, surgical resection may provide better long-term outcomes in patients with indolent malignant HIPT-like FDCSs.
The authors thank Clinical Medical School, Guizhou Medical University, and the Hepatobiliary Department, Affiliated Hospital of Guizhou Medical University.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lin J, China; Sahin TT, Turkey S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Pileri SA, Grogan TM, Harris NL, Banks P, Campo E, Chan JK, Favera RD, Delsol G, De Wolf-Peeters C, Falini B, Gascoyne RD, Gaulard P, Gatter KC, Isaacson PG, Jaffe ES, Kluin P, Knowles DM, Mason DY, Mori S, Müller-Hermelink HK, Piris MA, Ralfkiaer E, Stein H, Su IJ, Warnke RA, Weiss LM. Tumours of histiocytes and accessory dendritic cells: an immunohistochemical approach to classification from the International Lymphoma Study Group based on 61 cases. Histopathology. 2002;41:1-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 491] [Cited by in RCA: 450] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 2. | Ge R, Liu C, Yin X, Chen J, Zhou X, Huang C, Yu W, Shen X. Clinicopathologic characteristics of inflammatory pseudotumor-like follicular dendritic cell sarcoma. Int J Clin Exp Pathol. 2014;7:2421-2429. [PubMed] |
| 3. | Cheuk W, Chan JK, Shek TW, Chang JH, Tsou MH, Yuen NW, Ng WF, Chan AC, Prat J. Inflammatory pseudotumor-like follicular dendritic cell tumor: a distinctive low-grade malignant intra-abdominal neoplasm with consistent Epstein-Barr virus association. Am J Surg Pathol. 2001;25:721-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 219] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 4. | Cazzola M. Introduction to a review series: the 2016 revision of the WHO classification of tumors of hematopoietic and lymphoid tissues. Blood. 2016;127:2361-2364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 5. | Aparicio Serrano A, Castro Rodríguez J, Gallego Jiménez E, Barrera Baena P. Inflammatory pseudotumor-like follicular dendritic cell sarcoma of the liver. Rev Esp Enferm Dig. 2021;113:378-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Lu SS, Wang Z, Zhao S, Liu WP. [Hepatic inflammatory pseudotumor-like follicular dendritic cell sarcoma with paravertebral metastasis and recurrence: report of a case]. Zhonghua Bing Li Xue Za Zhi. 2021;50:958-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Pascariu AD, Neagu AI, Neagu AV, Băjenaru A, Bețianu CI. Hepatic inflammatory pseudotumor-like follicular dendritic cell tumor: a case report. J Med Case Rep. 2021;15:410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (2)] |
| 8. | Jin K, Li MN, Li S, Li J, Chen N. [Hepatic inflammatory pseudotumor-like follicular dendritic cell sarcoma]. Zhonghua Gan Zang Bing Za Zhi. 2020;28:172-174. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Hang JF, Wang LC, Lai CR. Cytological features of inflammatory pseudotumor-like follicular dendritic cell sarcoma of spleen: A case report. Diagn Cytopathol. 2017;45:230-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Kwon H. Inflammatory pseudotumor-like follicular dendritic cell tumor of the spleen. Turk J Gastroenterol. 2018;29:128-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Li X, Shi Z, You R, Li Y, Cao D, Lin R, Huang X. Inflammatory Pseudotumor-Like Follicular Dendritic Cell Sarcoma of the Spleen: Computed Tomography Imaging Characteristics in 5 Patients. J Comput Assist Tomogr. 2018;42:399-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Gong QX, Fan QH, Zhou ZS, Zhang ZH, Yu MN, Wang Z, Wang C, Zhang WM. [Inflammatory pseudotumor-like follicular dendritic cell tumor of spleen]. Zhonghua Bing Li Xue Za Zhi. 2008;37:40-44. [PubMed] |
| 13. | Kazemimood R, Saei Hamedani F, Sharif A, Gaitonde S, Wiley E, Giulianotti PC, Groth JV. A Rare Case of Epstein-Barr Virus Negative Inflammatory Pseudotumor-like Follicular Dendritic Cell Sarcoma Presenting as a Solitary Colonic Mass in a 53-Year-Old Woman; Case Report and Review of Literature. Appl Immunohistochem Mol Morphol. 2017;25:e30-e33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Pan ST, Cheng CY, Lee NS, Liang PI, Chuang SS. Follicular Dendritic Cell Sarcoma of the Inflammatory Pseudotumor-like Variant Presenting as a Colonic Polyp. Korean J Pathol. 2014;48:140-145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Shi QY, Zheng Z, Wu HY, Chen JY, Fan XS. [Colonic inflammatory pseudotumor-like follicular dendritic cell sarcoma: report of a case]. Zhonghua Bing Li Xue Za Zhi. 2022;51:138-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | He H, Xue Q, Tan F, Yang L, Wang X, Gao Y, Mao Y, Mu J, Wang D, Zhao J, Zhao L, Gao S. A rare case of primary pulmonary inflammatory pseudotumor-like follicular dendritic cell sarcoma successfully treated by lobectomy. Ann Transl Med. 2021;9:77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 17. | Mograbi M, Stump MS, Luyimbazi DT, Shakhatreh MH, Grider DJ. Pancreatic Inflammatory Pseudotumor-Like Follicular Dendritic Cell Tumor. Case Rep Pathol. 2019;2019:2648123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Kiryu S, Takeuchi K, Shibahara J, Uozaki H, Fukayama M, Tanaka H, Maeda E, Akahane M, Ohtomo K. Epstein-Barr virus-positive inflammatory pseudotumour and inflammatory pseudotumour-like follicular dendritic cell tumour. Br J Radiol. 2009;82:e67-e71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Martins PN, Reddy S, Martins AB, Facciuto M. Follicular dendritic cell sarcoma of the liver: unusual presentation of a rare tumor and literature review. Hepatobiliary Pancreat Dis Int. 2011;10:443-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Levi Sandri GB, Colasanti M, Vennarecci G, Ettorre GM. Paraneoplastic arthritis as first symptom of a liver inflammatory pseudotumor-like follicular dendritic cell sarcoma. Liver Int. 2016;36:1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Xu L, Ge R, Gao S. Imaging features and radiologic-pathologic correlations of inflammatory pseudotumor-like follicular dendritic cell sarcoma. BMC Med Imaging. 2021;21:52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Horiuchi R, Uchida T, Kojima T, Shikata T. Inflammatory pseudotumor of the liver. Clinicopathologic study and review of the literature. Cancer. 1990;65:1583-1590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 23. | Lizarralde E, Martínez P, Ibañez T, Gutiérrez A. Primary hepatic lymphoma and primary biliary cirrhosis. Am J Gastroenterol. 2000;95:562-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Delshad SD, Ahdoot JJ, Portocarrero DJ. Primary hepatic lymphoma. Clin Gastroenterol Hepatol. 2010;8:e49-e50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Zhang BX, Chen ZH, Liu Y, Zeng YJ, Li YC. Inflammatory pseudotumor-like follicular dendritic cell sarcoma: A brief report of two cases. World J Gastrointest Oncol. 2019;11:1231-1239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 26. | Choe JY, Go H, Jeon YK, Yun JY, Kim YA, Kim HJ, Huh J, Lee H, Shin DH, Kim JE. Inflammatory pseudotumor-like follicular dendritic cell sarcoma of the spleen: a report of six cases with increased IgG4-positive plasma cells. Pathol Int. 2013;63:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 27. | Zhao M, Du X, OuYang B, Li M, Yang H. Inflammatory pseudotumor-like follicular dendritic cell sarcoma mimicking a colonic polyp. J Gastrointest Surg. 2021;25:2429-2430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |