Published online May 15, 2021. doi: 10.4251/wjgo.v13.i5.440
Peer-review started: December 8, 2020
First decision: March 8, 2021
Revised: March 21, 2021
Accepted: April 23, 2021
Article in press: April 23, 2021
Published online: May 15, 2021
Processing time: 149 Days and 11.7 Hours
The coronavirus disease 2019 (COVID-19) pandemic has made it more challenging for patients to undergo yttrium-90 (Y-90) radioembolization (RE). Same day Y-90 RE provides an opportunity to minimize logistical challenges and infection risk associated with COVID-19, thus improving patient access.
To describe the use of same day Y-90 RE with routine single photon emission computed tomography/computed tomography (SPECT/CT) in order to optimize therapy.
All patients were selected for Y-90 RE through a multidisciplinary tumor board, and were screened and tested for COVID-19 infection per institutional protocol. A same day procedure was developed, consisting of angiography, imaging, and Y-90 resin particle delivery. Routine SPECT/CT after technetium-99m macroaggregated albumin (Tc-99m MAA) administration was performed for assessment of arterial supply, personalized dosimetry, and extrahepatic activity. Post-treatment Y-90 bremsstrahlung SPECT/CT was performed for confirmation of particle delivery, by utilization of energy windowing to limit signal from previously administered Tc-99m MAA particles.
A total of 14 patients underwent same day Y-90 RE between March and June 2020. Mean lung shunt fraction was 6.13% (range 3.5%-13.1%). Y-90 RE was performed for a single lesion in 7 patients, while the remaining 7 patients had treatment of multifocal lesions. The largest lesion measured 8.3 cm. All patients tolerated the procedure well and were discharged the same day.
Same day Y-90 RE with resin-based microspheres is feasible, and provides an opportunity to mitigate infection risk and logistical challenges associated with the COVID-19 pandemic and beyond. We recommend consideration of SPECT/CT, especially among patients with complex malignancies, for the potential to improve outcomes and eligibility of patients to undergo same day Y-90 RE.
Core Tip: Same day yttrium-90 (Y-90) radioembolization with resin-based microspheres is feasible, and provides an opportunity to mitigate infection risk and logistical challenges associated with the coronavirus disease 2019 pandemic and beyond. We recommend consideration of single photon emission computed tomography/computed tomography, especially among patients with complex malignancies, for the potential to improve outcomes and eligibility of patients to undergo same day Y-90 RE.
- Citation: Elsayed M, Loya M, Galt J, Schuster DM, Bercu ZL, Newsome J, Brandon D, Benenati S, Behbahani K, Duszak R, Sethi I, Kokabi N. Same day yttrium-90 radioembolization with single photon emission computed tomography/computed tomography: An opportunity to improve care during the COVID-19 pandemic and beyond. World J Gastrointest Oncol 2021; 13(5): 440-452
- URL: https://www.wjgnet.com/1948-5204/full/v13/i5/440.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v13.i5.440
Yttrium-90 (Y-90) radioembolization (RE) is an increasingly accepted minimally invasive procedure in which radioactive particles are injected into hepatic arteries feeding tumor[1,2]. In carefully selected patients with unresectable malignancy, Y-90 RE improves survival compared to conventional treatments[3-6].
Despite the favorable safety profile and clinical benefits of Y-90 RE, a disadvantage of this procedure compared to other locoregional therapies is that it is typically performed as a staged procedure requiring at least two visits. Prior to definitive Y-90 RE, an initial procedure is required in which angiographic mapping is performed to evaluate arterial anatomy and administer the radiotracer Technetium-99m macroaggregated albumin (Tc-99m MAA), which is used to determine lung shunt fraction (LSF)[1]. This procedure is also used to calculate the activity to be delivered to tumor and the presence of extrahepatic uptake. After this initial procedure, in most practices there is typically a 1-3 week waiting period for the delivery of Y-90 glass or resin-based microspheres.
Recent publications have indicated that Y-90 RE can be safely performed during a single day, rather than as two separate procedures spaced over multiple days or weeks[7-9]. During this same day procedure, pre-treatment mesenteric angiography, LSF evaluation, and Y-90 RE is performed during the same visit[7,10]. By performing Y-90 RE during that same day, this therapy becomes even more competitive with other locoregional therapies that do not require multiple procedures[7]. This is especially beneficial for patients with travel hardships, difficult vascular access, contrast allergies, and those who require monitored anesthesia care[7]. In addition, a same day procedure is likely to result in cost savings and fewer procedural complications[7].
Since the outbreak of the severe acute respiratory syndrome coronavirus (SARS-CoV-2) global pandemic, it has been increasingly important to minimize patient visits while maintaining a high level of care. Safety for oncology patients is paramount, as COVID-19 infection among these patients is associated with high mortality[11-13]. Given the increased safety and logistical challenges of protecting patients in the time of the SARS-CoV-2 pandemic, same day Y-90 planning and therapy for eligible patients becomes an increasingly attractive care model.
Existing literature suggests that same day Y-90 RE should be more strongly considered among patients with small, solitary, and peripheral tumors[7,9]. The reasoning for this is that LSF tends to be low in these patients, making it simple to calculate a tumor dose which exceeds threshold activity[14]. This enables a shorter and less complex procedure, since planar scintigraphy without single photon emission computed tomography/computed tomography (SPECT/CT) can be performed after Tc-99m MAA administration. A study by Gabr et al[15] even proposed eliminating Tc-99m MAA scans entirely in patients with United Network for Organ Sharing stage T1/T2 hepatocellular carcinoma (HCC) without prior transjugular intrahepatic portosystemic shunt (TIPS), since hepatopulmonary shunting is low and dose can be easily calibrated for segmental injections[15]. Conversely, more complex malignancies such as in patients with larger tumors, multiple lesions, prior TIPS placement, and other lesions at high risk for hepatopulmonary shunting may necessitate personalized dosimetry for good treatment response after Y-90 RE[16,17]. SPECT/CT analysis also enables detailed assessment of arterial supply and extrahepatic uptake[18]. In addition, post-treatment bremsstrahlung SPECT/CT imaging is useful for confirmation of adequate Y-90 dose delivery[19-24].
SPECT/CT for personalized dosimetry has been increasingly validated as a tool to improve outcomes in select patients. This is due to the ability to augment administered dose and deliver sufficient threshold activity to the tumor, which is correlated with increased pathological necrosis[25]. A study by Garin et al[17] demonstrates that personalized dosimetry with SPECT/CT improves overall survival without increasing liver toxicity among patients with HCC and portal vein thrombosis. A randomized multicenter trial examining personalized dosimetry among patients with advanced HCC (including at least one measurable lesion 7 cm or larger) also demonstrated greater rates of complete or partial response as well as improved survival. These findings reinforce the need for routine SPECT/CT in select populations[26].
To date, no series has described the use of same-day Y-90 in conjunction with the routine use of SPECT/CT. This report outlines our early experience with same day resin-based Y-90 RE during the COVID-19 pandemic, including the use of SPECT/CT after administration of Tc-99m MAA and Y-90 particles. We provide recommendations with regards to procedural technique and imaging in order to maximize the eligibility for patients to undergo Y-90 RE during a single day planning and treatment session.
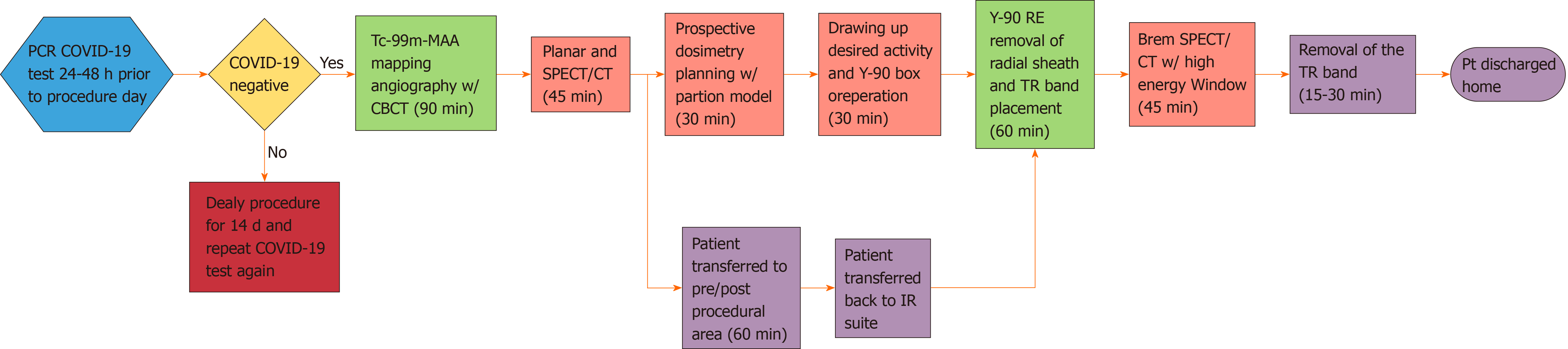
This series has been approved by the local Institutional Review Board, and the need for written informed consent was waived. All patients were referred to interventional radiology for Y-90 RE through multidisciplinary tumor boards. Exclusion criteria at the authors’ institution consisted of a tumor burden of greater than 75% of the whole liver, serum albumin < 2.5 g/dL, serum bilirubin > 2 mg/dL, and aspartate aminotransferase and alanine aminotransferase > 5 times the upper limit of normal. Patients who underwent same-day angiography and LSF evaluation were also required to have vascular anatomy amenable to catheter-directed therapy and LSF low enough that would permit administration of desired activity of Y-90 microspheres without exceeding lung dose limit of less than 30 Gray (Gy) per session and 50 Gy per lifetime. LSF and vascular anatomy were determined during the mapping portion of the same day procedure. All eligible patients were screened for COVID-19 symptoms and high risk exposures per institutional protocol. As part of this protocol, all patients were tested for COVID-19 using nasal swab polymerase chain reaction (PCR) analysis 24-48 h before the procedure day. The typical work flow of a same day procedure is depicted in Figure 1.
All patients selected for Y-90 RE underwent visceral angiography and administration of Tc-99m MAA into the hepatic artery vasculature for evaluation of hepatopulmonary shunting. Access was obtained via the radial artery in all patients, as described in prior literature[27]. Prior to Tc-99m MAA administration, angiography was performed for procedural planning, and embolization was considered for branch vessels thought to be at high risk for non-target embolization. Cone beam CT was utilized in all cases to ensure perfusion of the targeted tumor(s). If the entire tumor(s) were not perfused from the microcatheter location, either the microcatheter position was adjusted and the process was repeated or Tc-99m MAA was injected in a split dose to ensure the entire treatment lobe or segment was covered. During contrast injection from the selected vessel, careful attention was placed on the presence of reflux into nearby non-target branches. If there was excessive reflux that could not be resolved by repositioning the microcatheter, a Sniper balloon occlusion microcatheter (Embolx, Sunnyvale, CA, United States) was utilized to deliver Y-90 particles while preventing non-target embolization.
After administration of Tc-99m MAA, the 5 French (Fr) base catheter and coaxial microcatheter were disposed of in a radioactive waste bin. Vascular access was maintained by securing the 5 Fr radial sheath (Terumo Medical Corporation, Somerset, NJ, United States) with multiple Tegaderm dressings (3M, St. Paul, MN, United States). All patients went to nuclear medicine for Tc-99m MAA planar scintigraphy for evaluation of LSF. Anterior and posterior acquisitions of the chest and upper abdomen were acquired with a gamma camera using a low energy high-resolution parallel collimator, as described in prior literature[28]. Region of interest boxes were manually drawn over the liver and lung fields. Using the region of interest boxes, LSF was obtained by calculating the geometric mean of the counts.
After planar scintigraphy, Tc-99m MAA SPECT/CT images were obtained evaluate the tumor anatomy, assess the presence of extrahepatic activity, and perform personalized dosimetry. All patients were treated with resin-based Y-90 microspheres (Sirtex Medical Ltd, Woburn, MA). The partition dosimetry model was used in all patients[29]. In solitary tumors or tumors confined to a single segment (segmentec
The decision to order which calibration of resin microsphere using the Sirtex FLEXDosimetry program was made based on the targeted tumor(s) size and the volume of the liver to be treated approximately 2 wk before the day of planning/ therapy (https://www.sirtex.com/us/clinicians/flexdose-delivery-program/). For tumors in which segmentectomy or bi-segmentectomy was anticipated, a 3-d pre-calibrated activity was ordered. For lobar treatments with tumors > 8cm, 1-d pre-calibrated activity was ordered. For every other scenario, 2-d pre-calibrated activity was used. The rationale behind the calibration was based on the volume of the targeted the tumor(s) and the desire to have adequate coverage of the target with microspheres. In general, we opted to use resin calibrations which had greater activity per particle (“hotter”) for small tumors, which would allow adequate delivery of dose with a relatively small amount of particles. Resin calibrations with lower activity per particle (“colder”) for larger tumors were used to allow the delivery of more particles and adequate coverage of tumor.
After imaging, all patients returned to the peri-procedural area. Once Y-90 dosimetry planning was completed, patients returned to the interventional radiology suite for subselective catheterization of the hepatic artery via the pre-existing radial access and Y-90 RE was performed. The desired activity was administered via microcatheter from the same location where Tc-99m MAA was injected. After administration, access was removed and hemostasis was achieved using a hemostatic compression band as described in prior literature[30].
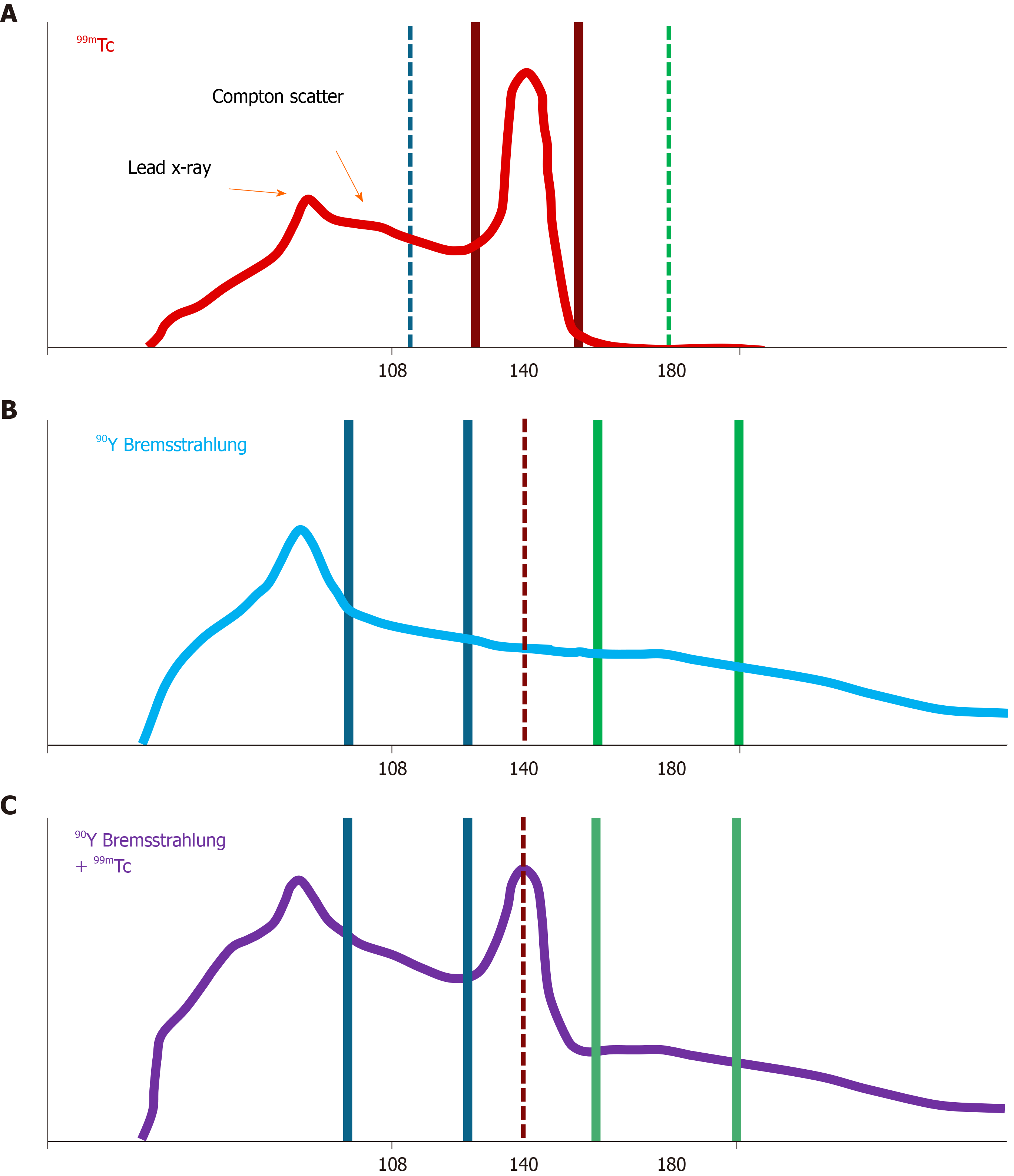
After Y-90 RE, bremsstrahlung SPECT/CT imaging was performed in order to confirm sufficient coverage of tumor. This was performed by using a high energy window of activity in order avoid including activity originating from the previously administered Tc-99m MAA. The spectral analysis of Tc-99m MAA and Y-90 as well as the reasoning behind using the high energy window during the bremsstrahlung SPECT/CT is summarized in Figures 2 and 3. Patients were discharged on the same day following embolization. Follow up imaging with CT or MRI 4-6 wk after therapy as well as a telemedicine appointment with the interventional oncology clinic was arranged.
There was a total of 15 patients initially selected for a single session Y-90 RE between April and June 2020. All patients were asymptomatic and tested negative for COVID-19 via PCR testing. Y-90 RE was not performed in a single patient due to an occluded celiac artery which could not be traversed on angiography, leaving 14 patients who underwent single session treatment. Additionally, superior mesenteric artery collaterals to the hepatic arteries were extremely tortuous and could not be safely cannulated with a microcatheter for delivery of Y-90 microspheres. Among the treated patients, 5 patients had HCC, while the remaining 9 patients had metastatic malignancies (Table 1). Age range of treated patients was 44-83 years. There were 9 female patients while the remaining 5 were male. All patients had an Eastern Cooperative Oncology Group status of 0. All patients with HCC had Model for End-Stage Liver Disease scores ranging from 6-11. One patient with HCC had a Child-Pugh score of A8, while the remaining had a Child-Pugh score of A5.
| Patient | Sex | Age | Diagnosis | ECOG status | MELD score | Child-Pugh Score | Number of lesions treated | Largest treated tumor size (cm) | LSF (%) | Access | Dose (mCI) | Extrahepatic activity | Embolized non-target vessel |
| 1 | F | 65 | HCC | 0 | 11 | A5 | 1 | 6.1 × 5.1 × 5.7 | 3.75 | Radial | 33.8 | No | NA |
| 2 | F | 65 | HCC | 0 | 10 | A5 | 1 | 2.8 × 2.3 × 2.3 | 4.46 | Radial | 59.8 | No | NA |
| 3 | F | 44 | Breast | 0 | NA | NA | 1 | 3.0 × 2.2 × 2.3 | 3.50 | Radial | 40.1 | No | NA |
| 4 | M | 60 | Colon | 0 | NA | NA | 3 | 4.7 × 3.9 × 4.1 | 5.69 | Radial | 40.48 | No | NA |
| 5 | F | 65 | Ovarian | 0 | NA | NA | 1 | 5.0 × 3.7 × 4.8 | 7.48 | Radial | 45.8 | No | NA |
| 6 | F | 72 | HCC | 0 | 6 | A5 | 1 | 2.0 × 2.3 × 2.5 | 6.61 | Radial | 75.01 | No | NA |
| 7 | M | 69 | HCC | 0 | 10 | A5 | 1 | 8.3 × 8.0 × 9.0 | 13.1 | Radial | 82.58 | No | NA |
| 8 | F | 83 | Colon | 0 | 7 | NA | 2 | 1.4 × 1.1 × 1.3 | 3.84 | Radial | 35.82 | No | NA |
| 9 | F | 38 | Breast | 0 | NA | NA | 1 | 3.2 × 3.2 × 3.5 | 3.70 | Radial | 53.48 | No | NA |
| 10 | F | 68 | Colon | 0 | NA | NA | 5+ | 1.9 × 1.8 × 1.9 | 3.59 | Radial | 45.38 | No | GDA |
| 11 | F | 68 | Neuroendocrine | 0 | NA | NA | 2 | 7.8 × 5.5 × 6.4 | 8.10 | Radial | 47.81 | No | Right gastric |
| 12 | M | 63 | HCC | 0 | 11 | A8 | 2 | 3.1 × 2.8 × 2.5 | 9.93 | Radial | 52.16 | No | NA |
| 13 | M | 58 | Colon | 0 | NA | NA | 2 | 2.0 × 1.8 × 2.3 | 3.57 | Radial | 32.93 | No | NA |
| 14 | M | 71 | Uveal melanoma | 0 | NA | NA | 2 | 5.4 × 5.0 × 5.2 | 8.49 | Radial | 59.85 | No | NA |
Planning and therapy were performed for multifocal lesions in 7 patients, while the remaining 7 patients had planning and therapy for a single lesion. Prophylactic embolization of non-target vessels was performed in two patients (gastroduodenal artery and right gastric artery). Mean LSF was 6.13% (range 3.5%-13.1%). No patient required dose adjustment based on LSF, as all projected lung doses were < 20 Gy. The largest treated lesion measured up to 8.3 cm. No extra-hepatic activity was noted on SPECT/CT scans.
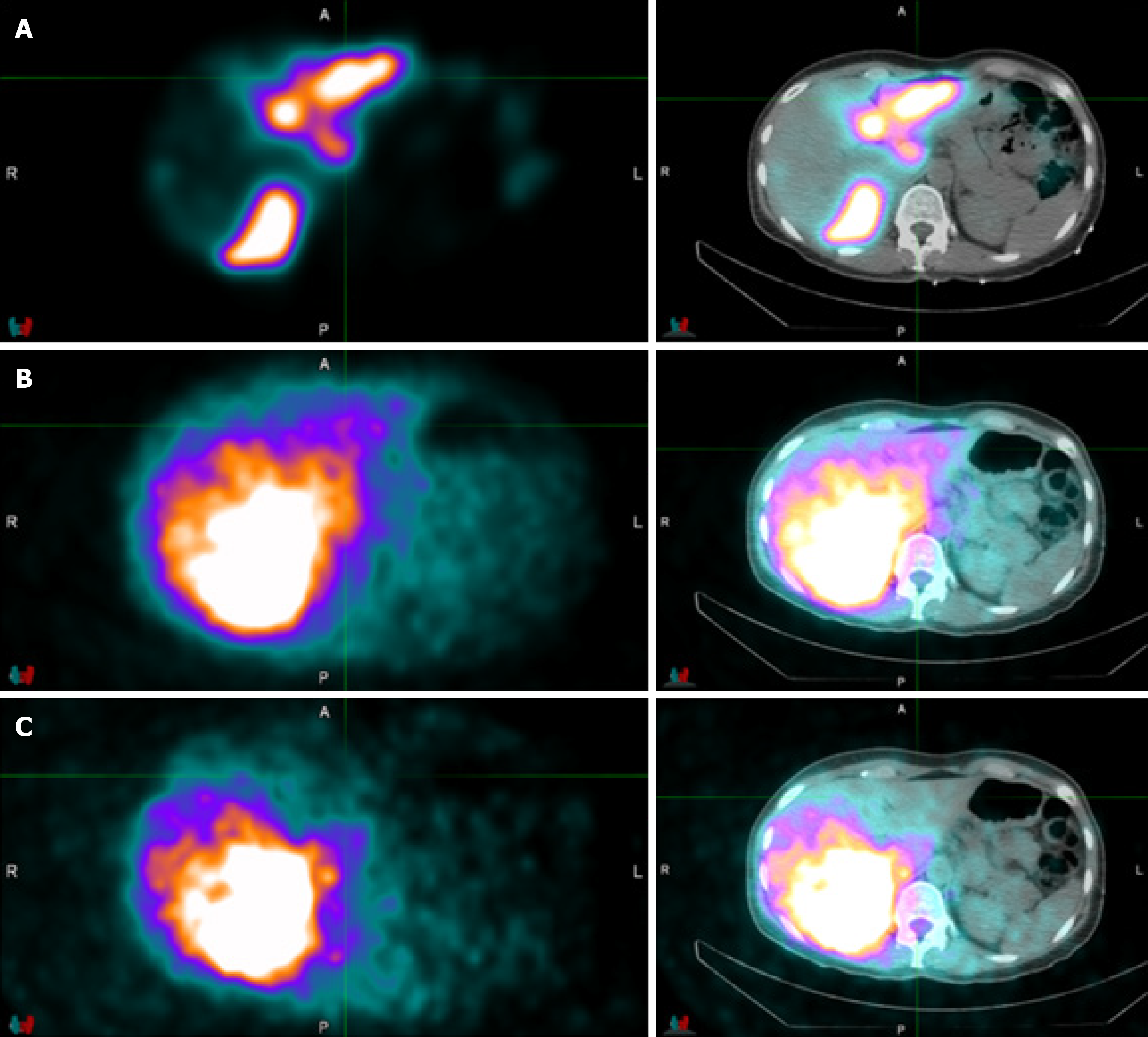
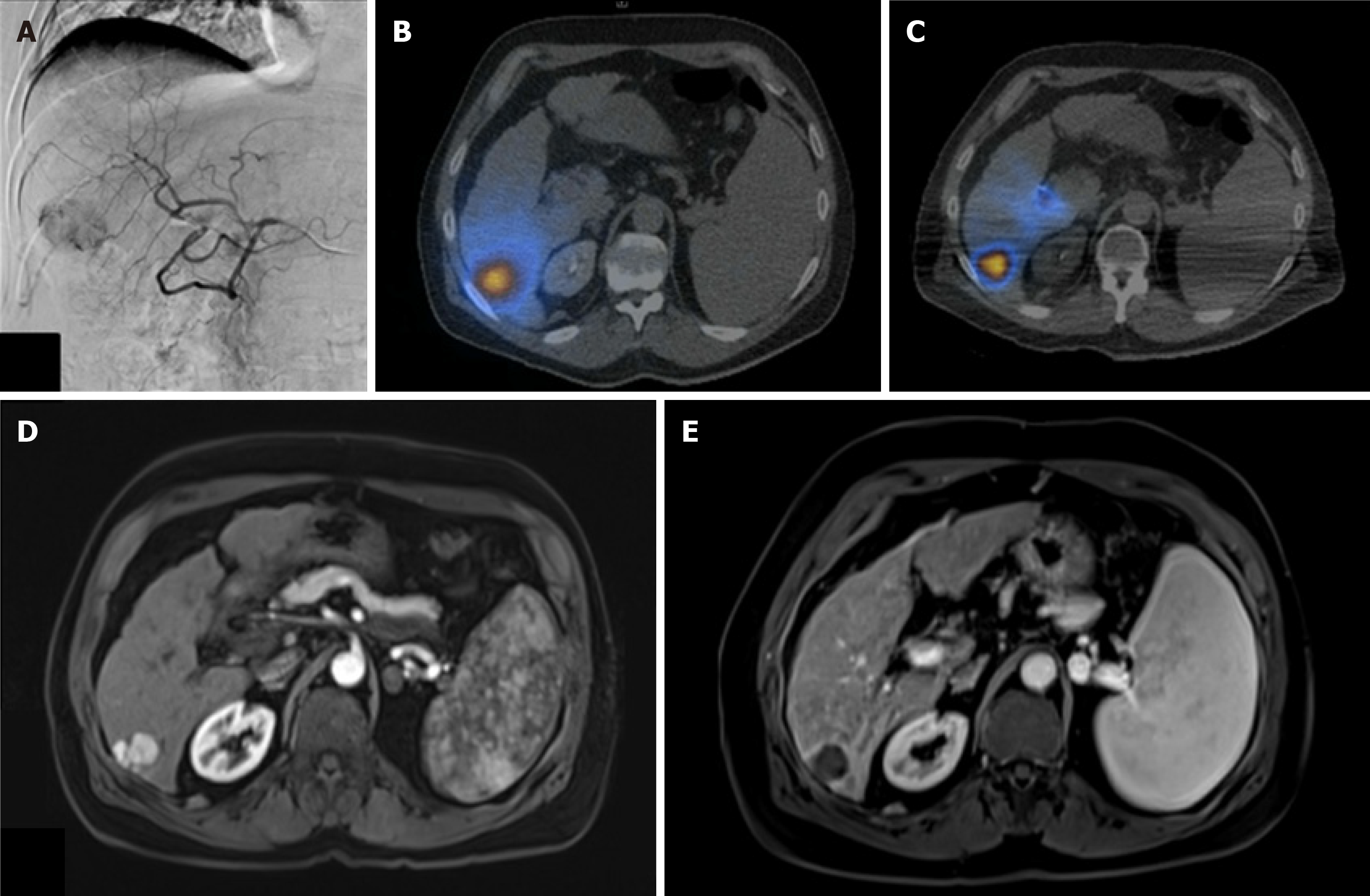
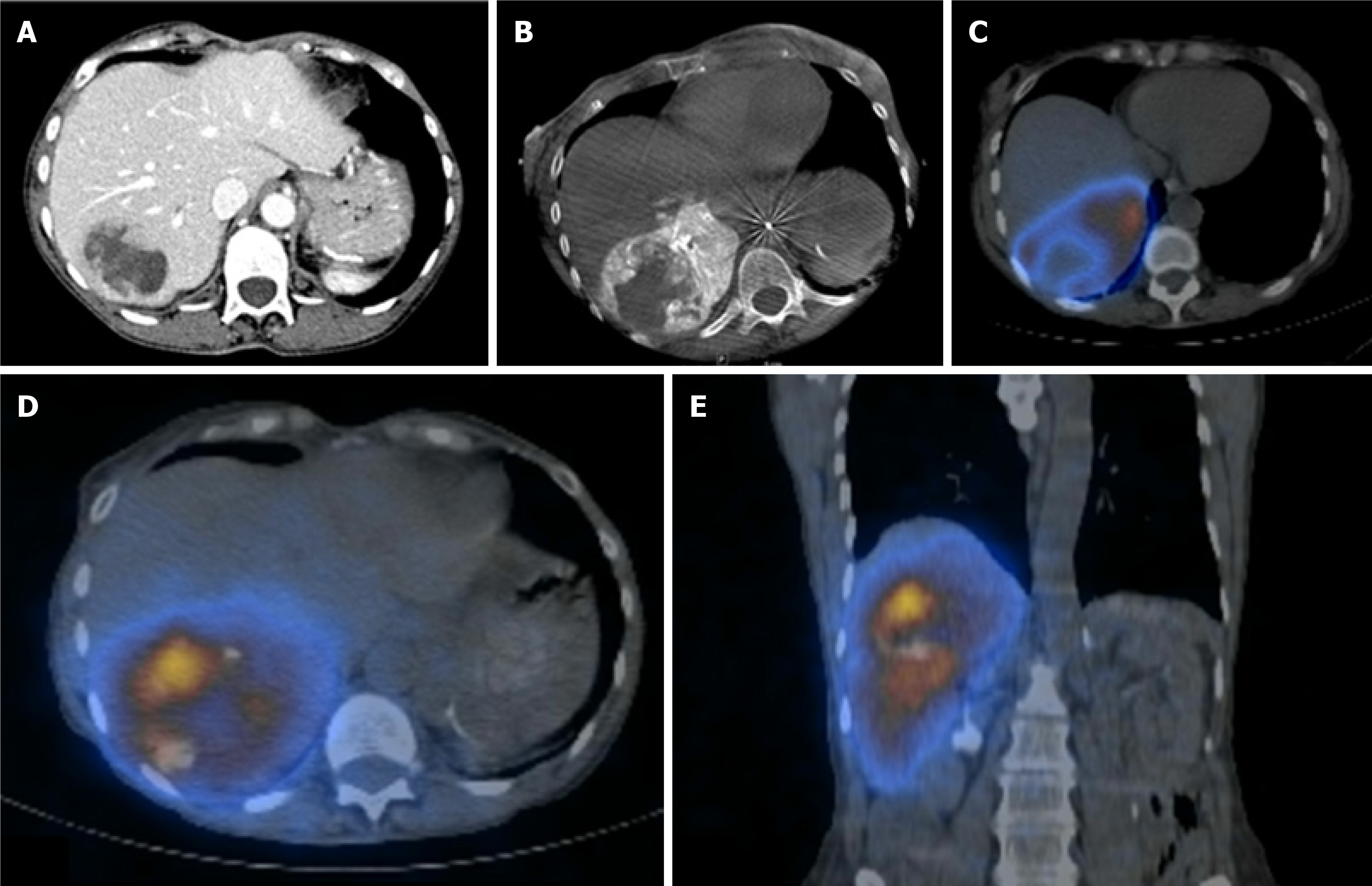
The time between Tc-99m MAA administration and Y-90 delivery was approximately 90-120 min. After Y-90 particle delivery, all patients underwent bremsstrahlung SPECT/CT imaging demonstrating adequate delivery of particles into tumor. Figure 3 depicts the differences in bremsstrahlung SPECT/CT obtained after administration of Tc-99m MAA and subsequently with Y-90 when using medium energy vs high energy windows. All patients tolerated the procedure well and were discharged home. Case examples are described in Figure 4 (segment 6 HCC treated with radiation segmentectomy) and Figure 5 (ovarian cancer treated with a posterior right lobe infusion).
The COVID-19 global pandemic has led to unprecedented challenges for oncology patients, their physicians, and other caregivers. Decreased screening, diagnosis, and treatment of cancer patients are anticipated to result in significant excess deaths[31]. Delays in care may also result in progression of malignancy which can preclude patients from certain treatments. This has resulted in a critical analysis of how to best care for oncology patients.
According to the American Society of Clinical Oncology, the overarching duty of a clinician during this pandemic is to maximize health outcomes while equitably allocating resources[32]. This is corroborated by the Society of Interventional Radiology, which recommends that treatments are prioritized according to the risk of future morbidity[33]. The interventional radiologist thus has competing obligations of providing effective and timely oncologic treatments while minimizing the risk of COVID-19 infection in patients and associated healthcare workers. Such challenges have resulted in re-examination by interventional radiology groups of how to treat patients with hepatic malignancies. For example, Garin et al[34] suggest that transarterial chemoembolization can be considered in lieu of Y-90 RE for certain patients, so that a staged procedure can be avoided.
Rather than opting for other systemic or locoregional therapies, we developed a care pathway to preserve patient access to Y-90 RE. This single day service offers a profound opportunity to provide effective therapy while minimizing complications related to COVID-19 infection by reducing visits to healthcare facilities. Prior series have already established that same day Y-90 RE can be safely performed in certain patients[7-10]. In the majority of cases within these series, the only imaging performed for dose calculation was planar scintigraphy, which allows for a short time interval between mapping and delivery. However, planar scintigraphy does not provide necessary information for more personalized dosimetry, which can maximize therapeutic effect while minimizing adverse events in certain patients[16,17,26].
Our series demonstrates the feasibility of offering same day Y-90 RE with routine Tc-99m MAA SPECT/CT as well as post-treatment bremsstrahlung SPECT/CT. Although this care pathway requires more time for acquisition of SPECT/CT images, it has the benefit of allowing more personalized dose calculation, detailed assessment of extra-hepatic activity, and confirmation of dose delivery. Additionally, with the advent of FLEXDosimetry products by Sirtex Medical, as discussed above, practically any type of Y-90 RE strategy can be performed including radiation segmentectomy of a small solitary tumor to lobar treatment of multifocal liver tumors. This approach is particularly attractive in less busy interventional oncology practices that may not have a large supply of glass microsphere vials of different activity readily available during the same day Y-90 RE.
Overall, the studied care pathway can increase the scope of patients who can be treated with same day Y-90 RE, including patients who have tumors with complex arterial supply and multifocal disease. In addition, the use of personalized dosimetric analysis likely results in better patient outcomes[26,35]. As previously mentioned, a randomized trial of patients with HCC by Garin et al[26] found that personalized dosimetry with SPECT/CT resulted in improved response rates and overall survival in patients with advanced HCC. As proposed in recent literature, a potential strategy may be the use of only planar scintigraphy (or even no LSF fraction evaluation) in patients with small peripheral tumors, and the use of SPECT/CT in patients with more complex malignancies who are likely to benefit from personalized dosimetry[16]. More research is necessary to elucidate an optimal treatment algorithm for same day therapy. Ultimately, we believe that more widespread adoption of same day Y-90 with resin microsphere and use SPECT/CT among patients with advanced malignancies will meaningfully optimize care for patients eligible for Y-90 during the COVID-19 pandemic and beyond.
Same day Y-90 RE with resin-based microspheres is feasible and provides an opportunity to mitigate infection risk and logistical challenges associated with the COVID-19 pandemic. We recommend consideration of SPECT/CT, especially among patients with complex malignancies, to improve outcomes and eligibility of patients to undergo same day Y-90 RE.
Yttrium-90 (Y-90) radioembolization (RE) is an intra-arterial targeted liver therapy for patients with hepatic malignancies. Recent publications demonstrate that Y-90 RE can be performed as a single combined procedure, rather than a staged procedures performed over multiple days.
Given the coronavirus disease 2019 (COVID-19) pandemic, there has been an increased need to mitigate infection risk and logistical challenges. By reducing the number of in-person visits, same day Y-90 RE provides an opportunity to improve patient care for oncology patients during the COVID-19 and beyond. However, existing literature describing same day Y-90 RE predominantly report the use of planar scintigraphy without single photon emission computed tomography/computed tomography (SPECT/CT), which may limit the ability to optimize therapy for patients with more advanced malignancies. This retrospective analysis describes the use of pre- and post-treatment SPECT/CT with personalized dosimetry during the COVID-19 pandemic.
Describe the use of same day Y-90 RE with routine SPECT/CT.
A same day procedure was developed, consisting of angiography, imaging, and Y-90 resin particle delivery. Routine SPECT/CT after Tc-99m MAA administration was performed for assessment of arterial supply, personalized dosimetry, and extrahepatic activity. Post-treatment Y-90 bremsstrahlung SPECT/CT was performed for confirmation of particle delivery, by utilization of energy windowing to limit signal from previously administered Tc-99m MAA particles.
A total of 14 patients underwent same day Y-90 RE with SPECT/CT. Mean lung shunt fraction was 6.13% (range 3.5%-13.1%). Y-90 RE was performed for a single lesion in 7 patients, while the remaining 7 patients had treatment of multifocal lesions. All patients tolerated the procedure well and were discharged the same day.
Same day Y-90 RE with resin-based microspheres is feasible, and provides an opportunity to mitigate infection risk and logistical challenges associated with the COVID-19 pandemic. Consideration of routine SPECT/CT is recommended, especially among patients with complex malignancies, for the potential to improve outcomes and eligibility of patients to undergo same day Y-90 RE.
Further studies of long-term patient outcomes and cost-benefit analyses would be useful to validate the utility of same day Y-90 with SPECT/CT.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and Hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Costache RS, Manrai M S-Editor: Liu M L-Editor: A P-Editor: Li JH
| 1. | Kruskal JB, Kung JW. The 2015 RadioGraphics Monograph Issue: Quality, Safety, and Noninterpretive Skills. Radiographics. 2015;35:1627-1629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Salem R, Lewandowski RJ, Sato KT, Atassi B, Ryu RK, Ibrahim S, Nemcek AA Jr, Omary RA, Madoff DC, Murthy R. Technical aspects of radioembolization with 90Y microspheres. Tech Vasc Interv Radiol. 2007;10:12-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 106] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Salem R, Lewandowski RJ, Mulcahy MF, Riaz A, Ryu RK, Ibrahim S, Atassi B, Baker T, Gates V, Miller FH, Sato KT, Wang E, Gupta R, Benson AB, Newman SB, Omary RA, Abecassis M, Kulik L. Radioembolization for hepatocellular carcinoma using Yttrium-90 microspheres: a comprehensive report of long-term outcomes. Gastroenterology. 2010;138:52-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 738] [Cited by in RCA: 781] [Article Influence: 52.1] [Reference Citation Analysis (0)] |
| 4. | Llovet JM, Real MI, Montaña X, Planas R, Coll S, Aponte J, Ayuso C, Sala M, Muchart J, Solà R, Rodés J, Bruix J; Barcelona Liver Cancer Group. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359:1734-1739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2502] [Cited by in RCA: 2611] [Article Influence: 113.5] [Reference Citation Analysis (0)] |
| 5. | Wang DS, Louie JD, Sze DY. Intra-arterial therapies for metastatic colorectal cancer. Semin Intervent Radiol. 2013;30:12-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Cianni R, Urigo C, Notarianni E, Saltarelli A, Salvatori R, Pasqualini V, Dornbusch T, Cortesi E. Selective internal radiation therapy with SIR-spheres for the treatment of unresectable colorectal hepatic metastases. Cardiovasc Intervent Radiol. 2009;32:1179-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Gabr A, Kallini JR, Gates VL, Hickey R, Kulik L, Desai K, Thornburg B, Marshall K, Salzig K, Williams M, Del Castillo C, Ganger D, Hohlastos E, Baker T, Lewandowski RJ, Salem R. Same-day 90Y radioembolization: implementing a new treatment paradigm. Eur J Nucl Med Mol Imaging. 2016;43:2353-2359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Li MD, Chu KF, DePietro A, Wu V, Wehrenberg-Klee E, Zurkiya O, Liu RW, Ganguli S. Same-Day Yttrium-90 Radioembolization: Feasibility with Resin Microspheres. J Vasc Interv Radiol. 2019;30:314-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Calvo A, Tabone M, Carbonatto P, Richetta E, Pellerito R. Radioembolization in a Single Session Using 90-Yttrium Resin Microspheres. J Vasc Interv Radiol. 2019;30:1648-1649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Gabr A, Ali R, Al Asadi A, Mora R, Mouli S, Riaz A, Salem R, Lewandowski RJ. Technical Aspects and Practical Approach Toward Same-Day Y90 Radioembolization in the Management of Hepatocellular Carcinoma. Tech Vasc Interv Radiol. 2019;22:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, Shete S, Hsu CY, Desai A, de Lima Lopes G Jr, Grivas P, Painter CA, Peters S, Thompson MA, Bakouny Z, Batist G, Bekaii-Saab T, Bilen MA, Bouganim N, Larroya MB, Castellano D, Del Prete SA, Doroshow DB, Egan PC, Elkrief A, Farmakiotis D, Flora D, Galsky MD, Glover MJ, Griffiths EA, Gulati AP, Gupta S, Hafez N, Halfdanarson TR, Hawley JE, Hsu E, Kasi A, Khaki AR, Lemmon CA, Lewis C, Logan B, Masters T, McKay RR, Mesa RA, Morgans AK, Mulcahy MF, Panagiotou OA, Peddi P, Pennell NA, Reynolds K, Rosen LR, Rosovsky R, Salazar M, Schmidt A, Shah SA, Shaya JA, Steinharter J, Stockerl-Goldstein KE, Subbiah S, Vinh DC, Wehbe FH, Weissmann LB, Wu JT, Wulff-Burchfield E, Xie Z, Yeh A, Yu PP, Zhou AY, Zubiri L, Mishra S, Lyman GH, Rini BI, Warner JL; COVID-19 and Cancer Consortium. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395:1907-1918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1195] [Cited by in RCA: 1282] [Article Influence: 256.4] [Reference Citation Analysis (0)] |
| 12. | Miyashita H, Mikami T, Chopra N, Yamada T, Chernyavsky S, Rizk D, Cruz C. Do patients with cancer have a poorer prognosis of COVID-19? Ann Oncol. 2020;31:1088-1089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 257] [Cited by in RCA: 302] [Article Influence: 60.4] [Reference Citation Analysis (0)] |
| 13. | Mehta V, Goel S, Kabarriti R, Cole D, Goldfinger M, Acuna-Villaorduna A, Pradhan K, Thota R, Reissman S, Sparano JA, Gartrell BA, Smith RV, Ohri N, Garg M, Racine AD, Kalnicki S, Perez-Soler R, Halmos B, Verma A. Case Fatality Rate of Cancer Patients with COVID-19 in a New York Hospital System. Cancer Discov. 2020;10:935-941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 493] [Cited by in RCA: 577] [Article Influence: 115.4] [Reference Citation Analysis (0)] |
| 14. | Gaba RC, Zivin SP, Dikopf MS, Parvinian A, Casadaban LC, Lu Y, Bui JT. Characteristics of primary and secondary hepatic malignancies associated with hepatopulmonary shunting. Radiology. 2014;271:602-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Gabr A, Ranganathan S, Mouli SK, Riaz A, Gates VL, Kulik L, Ganger D, Maddur H, Moore C, Hohlastos E, Katariya N, Caicedo JC, Kalyan A, Lewandowski RJ, Salem R. Streamlining radioembolization in UNOS T1/T2 hepatocellular carcinoma by eliminating lung shunt estimation. J Hepatol. 2020;72:1151-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 16. | Edeline J, Garin E. Streamlining TARE or personalizing SIRT? J Hepatol. 2020;72:1046-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Garin E, Rolland Y, Edeline J, Icard N, Lenoir L, Laffont S, Mesbah H, Breton M, Sulpice L, Boudjema K, Rohou T, Raoul JL, Clement B, Boucher E. Personalized dosimetry with intensification using 90Y-loaded glass microsphere radioembolization induces prolonged overall survival in hepatocellular carcinoma patients with portal vein thrombosis. J Nucl Med. 2015;56:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 114] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 18. | Lenoir L, Edeline J, Rolland Y, Pracht M, Raoul JL, Ardisson V, Bourguet P, Clément B, Boucher E, Garin E. Usefulness and pitfalls of MAA SPECT/CT in identifying digestive extrahepatic uptake when planning liver radioembolization. Eur J Nucl Med Mol Imaging. 2012;39:872-880. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Kim YC, Kim YH, Um SH, Seo YS, Park EK, Oh SY, Han YM, Choe JG. Usefulness of Bremsstrahlung Images after Intra-arterial Y-90 Resin Microphere Radioembolization for Hepatic Tumors. Nucl Med Mol Imaging. 2011;45:59-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Garin E, Lenoir L, Rolland Y, Edeline J, Mesbah H, Laffont S, Porée P, Clément B, Raoul JL, Boucher E. Dosimetry based on 99mTc-macroaggregated albumin SPECT/CT accurately predicts tumor response and survival in hepatocellular carcinoma patients treated with 90Y-loaded glass microspheres: preliminary results. J Nucl Med. 2012;53:255-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 213] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 21. | Garin E, Rolland Y, Edeline J. 90Y-Loaded Microsphere SIRT of HCC Patients With Portal Vein Thrombosis: High Clinical Impact of 99mTc-MAA SPECT/CT-Based Dosimetry. Semin Nucl Med. 2019;49:218-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Allimant C, Kafrouni M, Delicque J, Ilonca D, Cassinotto C, Assenat E, Ursic-Bedoya J, Pageaux GP, Mariano-Goulart D, Aho S, Guiu B. Tumor Targeting and Three-Dimensional Voxel-Based Dosimetry to Predict Tumor Response, Toxicity, and Survival after Yttrium-90 Resin Microsphere Radioembolization in Hepatocellular Carcinoma. J Vasc Interv Radiol 2018; 29: 1662-1670. e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 23. | Hermann AL, Dieudonné A, Maxime R, Manuel S, Helena P, Gilles C, Laurent C, Rachida L, Vilgrain V. Role of 99mTc-Macroaggregated Albumin SPECT/CT based dosimetry in predicting survival and tumor response of patients with locally advanced and inoperable hepatocellular carcinoma (HCC) treated by selective intra-arterial radiation therapy (SIRT) with yttrium-90 resin microspheres, a cohort from SARAH study. J Hepatol. 2018;68:S13. [DOI] [Full Text] |
| 24. | Kokabi N, Galt JR, Xing M, Camacho JC, Barron BJ, Schuster DM, Kim HS. A simple method for estimating dose delivered to hepatocellular carcinoma after yttrium-90 glass-based radioembolization therapy: preliminary results of a proof of concept study. J Vasc Interv Radiol. 2014;25:277-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Vouche M, Habib A, Ward TJ, Kim E, Kulik L, Ganger D, Mulcahy M, Baker T, Abecassis M, Sato KT, Caicedo JC, Fryer J, Hickey R, Hohlastos E, Lewandowski RJ, Salem R. Unresectable solitary hepatocellular carcinoma not amenable to radiofrequency ablation: multicenter radiology-pathology correlation and survival of radiation segmentectomy. Hepatology. 2014;60:192-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 233] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 26. | Garin E, Tzelikas L, Guiu B, Chalaye J, Edeline J, Baere TD, Tacher V, Robert C, Assenat E, Terroir-Cassou-Mounat M, Regnault H, Palard X, Laffont S, Campillo-Gimenez B, Rolland Y. Major impact of personalized dosimetry using 90Y loaded glass microspheres SIRT in HCC: Final overall survival analysis of a multicenter randomized phase II study (DOSISPHERE-01). J Clin Oncol. 2020;38:516-516. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Fischman AM, Swinburne NC, Patel RS. A Technical Guide Describing the Use of Transradial Access Technique for Endovascular Interventions. Tech Vasc Interv Radiol. 2015;18:58-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 28. | Kao YH, Tan EH, Ng CE, Goh SW. Clinical implications of the body surface area method versus partition model dosimetry for yttrium-90 radioembolization using resin microspheres: a technical review. Ann Nucl Med. 2011;25:455-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 29. | Pardo F, Sangro B, Lee RC, Manas D, Jeyarajah R, Donckier V, Maleux G, Pinna AD, Bester L, Morris DL, Iannitti D, Chow PK, Stubbs R, Gow PJ, Masi G, Fisher KT, Lau WY, Kouladouros K, Katsanos G, Ercolani G, Rotellar F, Bilbao JI, Schoen M. The Post-SIR-Spheres Surgery Study (P4S): Retrospective Analysis of Safety Following Hepatic Resection or Transplantation in Patients Previously Treated with Selective Internal Radiation Therapy with Yttrium-90 Resin Microspheres. Ann Surg Oncol. 2017;24:2465-2473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 30. | Sharpless NE. COVID-19 and cancer. Science. 2020;368:1290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 298] [Article Influence: 59.6] [Reference Citation Analysis (0)] |
| 31. | Marron JM, Joffe S, Jagsi R, Spence RA, Hlubocky FJ. Ethics and Resource Scarcity: ASCO Recommendations for the Oncology Community During the COVID-19 Pandemic. J Clin Oncol. 2020;38:2201-2205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 100] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 32. | Society of Interventional Radiology. COVID-19 case classification. 2020 Apr 8 [cited 21 June 2020] [Internet]. Available from: www.sirweb.org/practice-resources/toolkits/covid-19-toolkit/covid-19-case-classification. |
| 33. | Denys A, Guiu B, Chevallier P, Digklia A, de Kerviler E, de Baere T. Interventional oncology at the time of COVID-19 pandemic: Problems and solutions. Diagn Interv Imaging. 2020;101:347-353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 34. | Garin E, Rolland Y, Lenoir L, Pracht M, Mesbah H, Porée P, Laffont S, Clement B, Raoul JL, Boucher E. Utility of Quantitative Tc-MAA SPECT/CT for yttrium-Labelled Microsphere Treatment Planning: Calculating Vascularized Hepatic Volume and Dosimetric Approach. Int J Mol Imaging. 2011;2011:398051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |