Published online Mar 15, 2021. doi: 10.4251/wjgo.v13.i3.157
Peer-review started: December 16, 2020
First decision: January 11, 2021
Revised: January 18, 2021
Accepted: February 4, 2021
Article in press: February 4, 2021
Published online: March 15, 2021
Processing time: 78 Days and 6.5 Hours
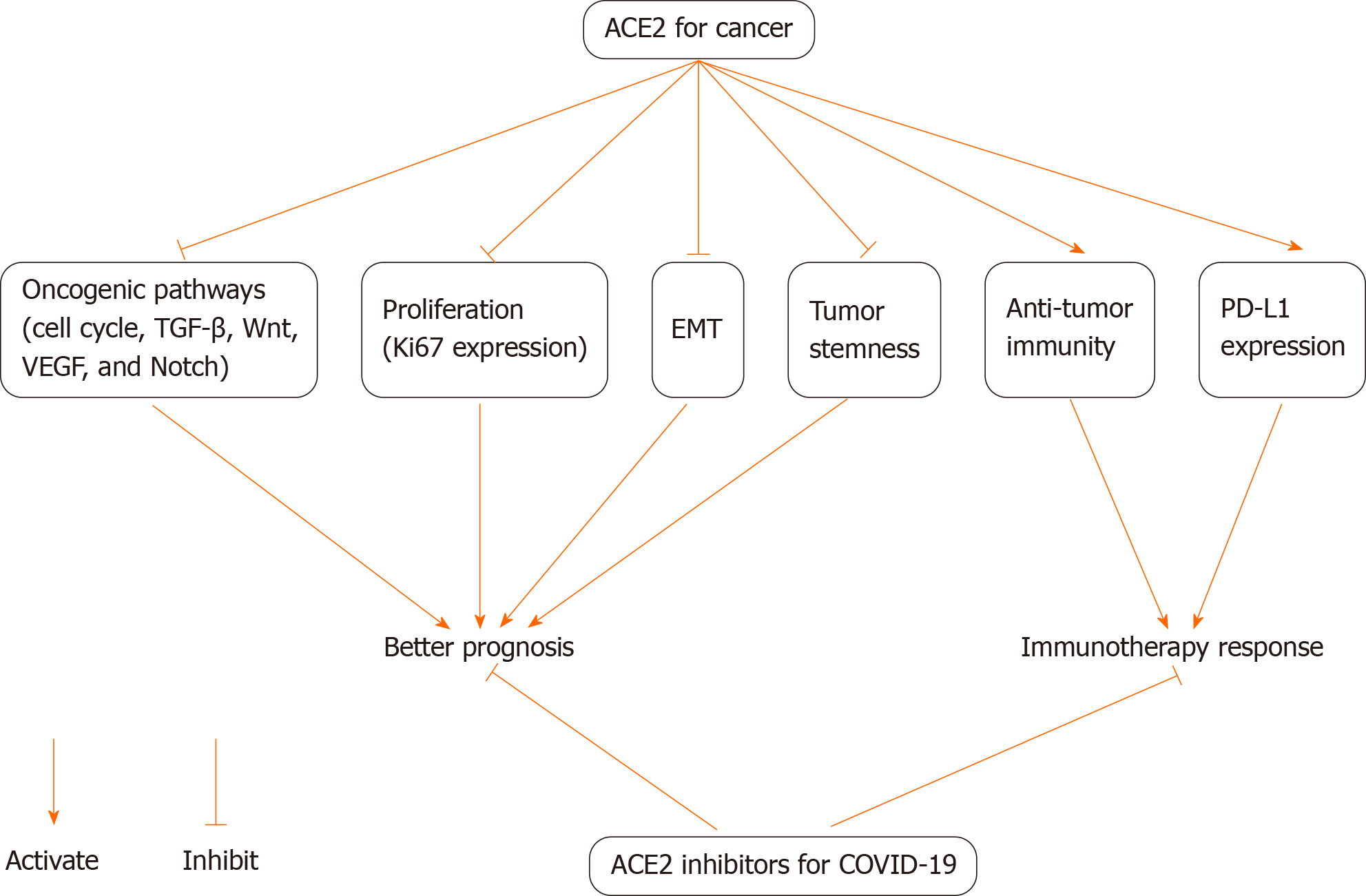
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in more than two million deaths. Underlying diseases, including cancer, are high-risk factors for severe COVID-19 outcomes. Angiotensin-converting enzyme 2 (ACE2), as a SARS-CoV-2 host cell receptor, plays a crucial role in SARS-CoV-2 invading human cells. ACE2 also has significant associations with cancer. Recent studies showed that ACE2 was inversely correlated with the activities of multiple oncogenic pathways and tumor progression phenotypes, and was positively correlated with antitumor immune response and survival prognosis in diverse cancers, suggesting a potential protective role of ACE2 in cancer progression. Positive expression of ACE2 is also correlated with programmed death-ligand 1 (PD-L1) in cancer. The positive associations of ACE2 expression with antitumor immune signatures and PD-L1 expression indicate that ACE2 expression is a positive predictor for the response to immune checkpoint inhibitors (ICIs). This was evidenced in multiple cancer cohorts treated with ICIs. Thus, ACE2 may build potential connections between COVID-19 and cancer and cancer immunotherapy. The potential connections suggest that ACE2 inhibitors may not be a good option for treating COVID-19 patients with cancer, particularly in cancer patients who are receiving immunotherapy. Furthermore, the relationships between ACE2, COVID-19, and cancer are worth confirming by more experimental and clinical data, considering that many cancer patients are at high risk for COVID-19.
Core Tip: Angiotensin-converting enzyme 2 (ACE2) is a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) host cell receptor and plays a crucial role in SARS-CoV-2 invading human cells to cause coronavirus disease 2019 (COVID-19). ACE2 also plays a role in preventing tumor progression and promoting cancer immunotherapy response. Thus, the use of ACE2 inhibitors to prevent and treat COVID-19 should be carried out cautiously in cancer patients.
- Citation: Wang XS. Angiotensin-converting enzyme 2 connects COVID-19 with cancer and cancer immunotherapy. World J Gastrointest Oncol 2021; 13(3): 157-160
- URL: https://www.wjgnet.com/1948-5204/full/v13/i3/157.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v13.i3.157
Infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused more than 113 million cases of coronavirus disease 2019 (COVID-19) and 2.5 million deaths as of February 25, 2021[1]. More seriously, a second wave of the COVID-19 pandemic has emerged and is expected to be more infectious and more deadly. Abundant evidence[2] has shown that many underlying diseases, including cancer, are risk factors for severe COVID-19 outcomes. Thus, specific measures to protect people with underlying diseases from SARS-CoV-2 infection or the development of severe COVID-19 are crucial for reducing COVID-19 deaths. Similar to cancer, COVID-19 may affect various human organs or tissues, including the lungs, kidneys, liver, brain, colon, stomach, and skin, in light of the fact that the SARS-CoV-2 host cell receptor angiotensin-converting enzyme 2 (ACE2) is expressed in a wide range of human tissues[3]. In fact, the essential role of ACE2 in SARS-CoV-2 invasion into human tissues is well recognized[4].
ACE2 also plays an important role in cancer. For example, Dai et al[5] showed that increased ACE2 expression was associated with a better survival prognosis in liver cancer. ACE2 exerts antitumor effects by inhibiting tumor angiogenesis[6]. Several recent studies explored the associations of ACE2 with antitumor immunity and immunotherapy response[7-9]. Yang et al[7] showed that the elevated expression of ACE2 was correlated with increased antitumor immune response in uterine corpus endometrial and renal papillary cell cancers. Bao et al[8] revealed strong associations between ACE2 expression and immune gene signatures in cancer. Our recent study[9] systematically explored the associations of ACE2 expression with antitumor immune signatures, tumor progression phenotypes, oncogenic signatures, and clinical features in 13 cancer cohorts. We found that the expression levels of ACE2 were inversely correlated with the levels of tumor proliferation, stemness, and epithelial-mesenchymal transition in diverse cancers. Moreover, ACE2 expression levels were inversely correlated with the activities of multiple oncogenic pathways in cancer, including the cell cycle, vascular endothelial growth factor, transforming growth factor-β, Wnt, and Notch signaling. In contrast, the expression levels of ACE2 correlated positively with diverse antitumor immune signatures in cancer, including antigen processing and presentation, T cell and B cell receptor signaling, nucleotide-binding and oligomerization domain-like receptor signaling, chemokine signaling, cytokine-cytokine receptor interaction, natural killer cell-mediated cytotoxicity, and Jak-STAT signaling. As a result, increased ACE2 expression was associated with a favorable survival prognosis in multiple cancer cohorts, including renal clear cell carcinoma, renal papillary cell carcinoma, lung adenocarcinoma, and ovarian carcinoma[9]. Interestingly, the expression levels of ACE2 were significantly lower in advanced than in non-advanced tumors in renal clear cell carcinoma. Overall, these data suggest a potential protective role of ACE2 in cancer development. Interestingly, positive expression of ACE2 was significantly correlated with the gene encoding programmed death-ligand 1 (PD-L1) in cancer. As both the inflamed immune microenvironment and high PD-L1 expression are positively associated with the response to immune checkpoint inhibitors (ICIs), ACE2 upregulation may indicate an increased immunotherapy response in cancer. Indeed, in four cancer cohorts involving three cancer types (melanoma, renal clear cell carcinoma, and bladder cancer), the cancers with higher ACE2 expression levels (> median) showed a higher rate of response to ICIs than the cancers with lower ACE2 expression levels (< median).
Emerging evidence suggests potential associations between COVID-19 and cancer and cancer immunotherapy through ACE2 (Figure 1). In light of the important roles of ACE2 in preventing tumor progression and promoting cancer immunotherapy response, ACE2 inhibitors may not be a good option for treating COVID-19 patients with cancer, particularly in cancer patients who are receiving immunotherapy. The protective role of ACE2 in cancer progression and the function of ACE2 in promoting cancer immunotherapy response need to be further confirmed by more experimental and clinical data.
I appreciate Mr. Feng QS from China Pharmaceutical University for editing the manuscript.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mostaf-Hedeab G S-Editor: Fan JR L-Editor: Webster JR P-Editor: Li JH
| 1. | Johns Hopkins University. COVID-19 Dashboard by the Center for System Science and Engineering (CSSE) at Johns Hopkins University (JHU) [Internet]. 2020. Available from: https://coronavirus.jhu.edu/map.html. |
| 2. | Li M, Zhang Z, Cao W, Liu Y, Du B, Chen C, Liu Q, Uddin MN, Jiang S, Chen C, Zhang Y, Wang X. Identifying novel factors associated with COVID-19 transmission and fatality using the machine learning approach. Sci Total Environ. 2020;764:142810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 59] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 3. | Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1028] [Cited by in RCA: 1068] [Article Influence: 213.6] [Reference Citation Analysis (0)] |
| 4. | Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020; 181: 271-280. e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11946] [Cited by in RCA: 14274] [Article Influence: 2854.8] [Reference Citation Analysis (0)] |
| 5. | Dai YJ, Hu F, Li H, Huang HY, Wang DW, Liang Y. A profiling analysis on the receptor ACE2 expression reveals the potential risk of different type of cancers vulnerable to SARS-CoV-2 infection. Ann Transl Med. 2020;8:481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 6. | Zhang Q, Lu S, Li T, Yu L, Zhang Y, Zeng H, Qian X, Bi J, Lin Y. ACE2 inhibits breast cancer angiogenesis via suppressing the VEGFa/VEGFR2/ERK pathway. J Exp Clin Cancer Res. 2019;38:173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 193] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 7. | Yang J, Li H, Hu S, Zhou Y. ACE2 correlated with immune infiltration serves as a prognostic biomarker in endometrial carcinoma and renal papillary cell carcinoma: implication for COVID-19. Aging (Albany NY). 2020;12:6518-6535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 8. | Bao R, Hernandez K, Huang L, Luke JJ. ACE2 and TMPRSS2 expression by clinical, HLA, immune, and microbial correlates across 34 human cancers and matched normal tissues: implications for SARS-CoV-2 COVID-19. J Immunother Cancer. 2020;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 9. | Zhang Z, Li L, Li M, Wang X. The SARS-CoV-2 host cell receptor ACE2 correlates positively with immunotherapy response and is a potential protective factor for cancer progression. Comput Struct Biotechnol J. 2020;18:2438-2444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |