Published online Aug 16, 2017. doi: 10.4253/wjge.v9.i8.378
Peer-review started: February 2, 2017
First decision: February 20, 2017
Revised: March 30, 2017
Accepted: July 7, 2017
Article in press: July 10, 2017
Published online: August 16, 2017
Processing time: 200 Days and 7.4 Hours
The inspection of the liver is a valuable part of the upper endoscopic ultrasonography (EUS) studies, regardless of the primary indication for the examination. The detailed images of the liver segments provided by EUS allows the use of this technique in the study of parenchymal liver disease and even in the diagnosis and classification of focal liver lesions. EUS has also emerged as an important tool in understanding the complex collateral circulation in patients with portal hypertension and their clinical and prognostic value. Recently, EUS-guided portal vein catheterization has been performed for direct portal pressure measurement as an alternative method to evaluate portal hemodynamics. In this review, the authors summarize the available evidence regarding the application of EUS to patients with liver diseases and how we can apply it in our current clinical practice.
Core tip: This review summarizes the current status of the available evidence regarding the application of endoscopic ultrasonography (EUS) to patients with liver diseases, focusing on recent breakthroughs and its potential application on clinical practice. We highlight the emerging role of EUS in the study of parenchymal liver disease as well as in the diagnosis and classification of focal liver lesions. Finally, we emphasise the crucial role of EUS in the understanding of the complex collateral circulation in patients with portal hypertension.
- Citation: Magalhães J, Monteiro S, Xavier S, Leite S, de Castro FD, Cotter J. Endoscopic ultrasonography - emerging applications in hepatology. World J Gastrointest Endosc 2017; 9(8): 378-388
- URL: https://www.wjgnet.com/1948-5190/full/v9/i8/378.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i8.378
In the recent years, there has been remarkable improvement in hepatology, with new treatments for viral hepatitis, recommendations for the follow-up of cirrhotic patients and treatment of portal hypertension complications. These advances have brought an increased need for the assessment of liver function and liver histologic characterization.
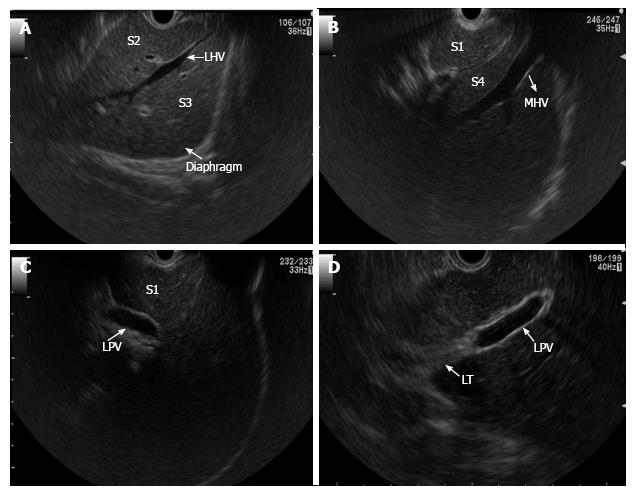
Endoscopic ultrasonography (EUS) has become an important tool, not only in the diagnosis of several gastrointestinal lesions, but also in performing various therapeutic manoeuvres[1]. Due to the close proximity of the transducer to the liver, from the transgastric and transduodenal routes, EUS allows a clear visualization of the liver anatomy and its vasculature providing accurate and detailed images[2,3] (Figure 1). As experience grows with this technique new indications for EUS continue to emerge, and endosonographers have made an effort to define a clinical role for EUS in liver diseases.
This review summarizes the available evidence regarding the application of EUS to patients with liver diseases and how it can be applied in a current clinical practice.
Although non-invasive tests, such as elastography or serologic markers for liver fibrosis, have been developed, the liver biopsy remains an important part of the liver disease evaluation and management[4].
Liver biopsy has been commonly performed by percutaneously image-guided. A transjugular fluoroscopy-guided approach is used when the percutaneous route is not safe, because of coagulopathy or ascites[5,6].
EUS-guidance represents an emerging method of liver biopsy. EUS provides images of both lobes of the liver, moreover biopsy needle can be safely directed into the liver under image guidance, and intervening vessels and organs can be avoided.
EUS-guided liver biopsy (EUS-LB) for studying parenchymal liver disease has largely been studied with the use of different needles. Since a tissue core biopsy with a preserved architecture is crucial to diagnosis and fully characterization of the hepatic diseases, needles specifically designed for core biopsy have been used. The ability to obtain specimens of liver tissue for histologic examination with a Tru-Cut biopsy needle dedicated for EUS-guided biopsy, the Quick-Core® needle (Cook® Medical), were demonstrated in some published studies[7,8]. In a study by DeWitt et al[8], 21 consecutive patients underwent liver biopsy by using a Quick-Core® needle. Liver biopsy specimens were able to provide diagnostic clinical information in only 15 of 21 patients (71%), the total specimen length was a median of 9 mm, with a median of 2 complete portal tracts. The technique was safe and feasible. However the samples were smaller than those traditionally considered adequate for histologic assessment.
The Tru-Cut biopsy needle failed to reach widespread use due to technical difficulties with its utilization. To overcome the main limitations of a Tru-Cut biopsy needle, the same manufacture developed a new needle, the ProCore® needle (Cook® Medical). Sey et al[9] compared the diagnostic yield of a 19-gauge ProCore® needle with a Quick-Core® needle. A total of 45 patients underwent liver biopsy by using the Quick-Core® and 30 patients the ProCore® needle. The ProCore® needle group required fewer passes (median 2 vs 3, P < 0.0001), produced a longer median specimen length (median 20 mm vs 9 mm, P < 0.0001) with more complete portal tracts (median 5 vs 2, P = 0.0003) and also allowed a histologic diagnosis more frequently (97% vs 73%).
Other studies have also been published demonstrating the adequacy of liver tissue sampling by a 19-gauge FNA needle. Stavropoulos et al[10] presented a study in which patients underwent a EUS-LB with a 19-gauge FNA needle. All patients underwent EUS with a 7.5-MHz linear echoendoscope (Olympus GF-UC140P-AL5; Olympus, Tokyo, Japan) as the initial procedure. Twenty-two patients underwent a EUS-LB of the left lobe of the liver, a median of 2 passes (range 1-3) yielded a median specimen length of 36.9 mm, with a median of 9 complete portal tracts and a diagnostic yield of 91%, without post-procedure complications. The authors concluded that EUS-LB by using a 19-gauge FNA needle was feasible, safe, with an excellent diagnostic yield and sample adequacy for histologic examination.
To evaluate the diagnostic yield of EUS-LB in a large patient cohort, Diehl et al[11] recently presented a prospective, multicentre study with 110 patients who underwent EUS-LB at eight centres. EUS examination was performed with a linear echoendoscope (GF-UC140P, Olympus America, Center Valley, PA, United States). The biopsy was performed using a 19-gauge FNA needle, with or without a stylet, 7-10 to-and-fro motions of the needle were made per pass (1-2 pass were made), using the fanning technique and almost all endoscopists preferred to use full suction for the needle aspiration. Adequate liver biopsy specimens for pathological diagnosis were obtained in 98% of patients, with a median specimen length of 38 mm, with median of 14 complete portal tracts. There were five patients whose tissue yield was less than 6 complete portal tracts with aggregate length less than 15 mm. Nevertheless it has been possible to obtain a histological diagnosis in samples from four patients. There was no statistical difference in the yield between bilobar, left lobe only, or right lobe only biopsies. There was, however, one complication, where self-limited bleeding (pericapsular hematoma) occurred in a patient with coagulopathy and thrombocytopenia (platelets, 64000; INR, 1.42), evaluated for abnormal transaminases.
In a recent study by Pineda et al[12] the EUS-LB was for the first time compared with the other methods of liver biopsy (percutaneous and transjugular). The EUS-LB was obtained in widely separated regions of the liver or one single region only using a 19-gauge FNA needle. There were 68 EUS-LB cases when both lobes were biopsied, the left lobe only in 34 cases and transduodenal liver biopsy only in 8 cases. A sample of 27 percutaneous liver biopsies and 38 transjugular liver biopsies were selected. EUS-LB of both liver regions produced significantly more tissue in terms of both total specimen length (40 mm vs 25 mm, P < 0.001) and complete portal tracts (17 vs 10, P < 0.001) compared to a percutaneous liver biopsy. EUS-LB produced significantly longer total specimen length than transjugular liver biopsy (40 mm vs 34 mm, P = 0.01) and similar complete portal triads (17 vs 15.5, P = 0.22). Those EUS-LB cases in which the left lobe only was sampled were not statistically different compared to percutaneous and transjugular liver biopsy.
Nowadays the EUS-LB could be considered a procedure with several advantages. The liver can be sampled under ultrasonographic visualization, which is important to avoid vessels and organs. The biopsy of both left and right lobes of the liver can overcome the concerns about sampling error, since a more accurate representation of liver histology can be provided. Another potential advantage is that the patient is sedated for the EUS procedure, making the experience less unconfortable.
All previous reports excluded patients with international normalized ratio (INR) > 1.5, thrombocytopenia (platelets < 50000/uL) and antiplatelet agents within 5 d of the procedure. Although the needle puncture occurs under ultrasonographic guidance, Glisson’s capsule is punctured, and bleeding remains a concern, thus the use of EUS for these patients is not recommended. The Table 1 summarizes the data from the main studies of EUS-LB.
| Ref. | Study design | Needle | Passes | Specimen length (median) | Complete portal tracts (median) | Histological diagnosis |
| DeWitt et al[8] | Prospective unicentre study n = 21 | Quick-Core1 | 1-4 | 9 mm | 2 | 71% |
| Diehl et al[11] | Prospective multicentre study n = 110 | 19G (FNA) Expect1 | 1-2 | 38 mm | 14 | 98% |
| Stavropoulos et al[10] | Prospective unicentre study n = 22 | 19G (FNA) Echotip2 | 1-3 | 36.9 mm | 9 | 91% |
| Sey et al[9] | Prospective unicentre study n = 75 | Quick-Core1 | 1-7 | 9 mm | 2 | 73% |
| ProCore 19G1 | 1-3 | 20 mm | 5 | 97% |
Focal liver lesions are frequently incidentally discovered during an imaging test, such as ultrasonography (US) or computed tomography (CT). Other times they are found in patients with risk factors for hepatic malignancy or even during a preoperative staging of extra-hepatic malignancies. Accurate characterization of these lesions remains an integral part of patients’ evaluation, as the extent of liver involvement may change clinical stage and management.
The inspection of the liver is a valuable part of the upper EUS studies, regardless of the primary indication for the examination. Recently, EUS and EUS-guided fine needle aspiration (EUS-FNA) has emerged as an important tool in the diagnosis and classification of liver lesions. Most of the liver segments can be visualized with the echoendoscope[3] and the proximity of the ultrasound probe to the liver parenchyma provides exceptional images of the liver parenchyma, which may have a key role in the detection, characterization and even in the definitive diagnosis of liver lesions.
Awad et al[13] evaluated the feasibility of EUS for the detection and diagnosis of liver lesions in 14 patients with known or suspected hepatocellular carcinoma (HCC) and metastatic liver lesions. Consecutive patients referred for EUS with suspected liver lesions were evaluated. EUS not only successfully identified all previously hepatic lesions described by CT scan, but also identified new or additional lesions in 4 patients (28%), all less than 0.5 cm in size. Nine patients underwent EUS-FNA of hepatic lesions, with a 22-gauge needle and two passes for each lesion, and all FNA yielded adequate specimens. The authors suggested that EUS is an adequate preoperative staging tool for liver lesions suspected to be HCC or metastatic lesions, as EUS can detect small hepatic lesions previously undetected by dynamic CT scans.
Singh et al[14] have conducted a prospective trial to compare the accuracy of EUS and EUS-FNA with other imaging modalities for the detection of primary liver tumors in subjects at high risk of HCC. Seventeen subjects were enrolled in the study. The EUS has detected more HCC lesions than US (8 vs 2, P = 0.06), CT (19 vs 8, P = 0.06) or magnetic resonance imaging (MRI) (14 vs 7, P = 0.25), although not statistically significant. Moreover, EUS has detected small HCC lesions that has been missed by CT and MRI, with the smallest lesion visualized by EUS and confirmed by FNA having 4 mm in size. Thus, EUS-FNA helped in the determination of the cytological nature of liver nodular lesions that were indeterminate on CT and MRI. A diagnostic algorithm has been proposed in which EUS could be used for high-risk patients with inconclusive CT, or poorly accessible lesions requiring tissue confirmation.
In a study by DeWitt et al[15], the sensitivity of EUS features and EUS-FNA for benign and malignant solid liver lesions was described. The EUS-FNA was performed on 77 different liver lesions, a total of 45 aspirates (58%) were diagnostic for malignancy (true positives), of these, 44 were metastatic and one was a HCC. In 25 patients (55%), the FNA provided both the primary diagnosis and upstaged the malignancy and in nine subjects (20%) the EUS-FNA made the initial diagnosis, upstaged the tumor, and prevented surgery. Three lesions previously classified as benign were lately, by intraoperative findings or percutaneous-FNA, reclassified as malignant (false negatives). The EUS features predictive of malignant hepatic lesions were the presence of regular outer margins (60% vs 27%, P = 0.02) and the detection of two or more lesions (38% vs 9%, P = 0.03). EUS-FNA was performed using a 22-gauge needle and no complications were reported. This study concluded that EUS is a safe and sensitive procedure that can have a significant impact on patient management. The Table 2 summarizes the reported data from the studies of EUS of Focal liver lesions.
| Ref./study design | Study population | Patient number/EUS-FNA | EUS diagnostic yield | EUS-FNA diagnostic yield |
| Awad et al[13] Prospective unicenter study | Suspected HCC or metastatic liver carcinoma | 14/9 | EUS identified all hepatic lesions (n = 14) previously reported by CT 4 new/additional lesions identified by EUS | All FNA passes yielded adequate specimens (malignant: n = 8; benign: n = 1) |
| Singh et al[14] Prospective unicenter study | High risk for HCC | 17/16 | The diagnostic accuracy of US, CT, MRI, and EUS/EUS-FNA were 38%, 69%, 92%, and 94% | Cytologic diagnosis of primary liver tumor was established in 8 cases (HCC = 7; cholangiocarcinoma = 1) |
| DeWitt et al[15] Retrospective unicenter study | Staging EUS examinations for known or suspected malignancy | 77/77 | EUS features predictive of malignant hepatic lesions were the presence of regular outer margins and the detection of two or more lesions | 45 aspirates were diagnostic for malignancy (metastasis: n = 44; HCC = 1) |
The diagnosis of portal vein thrombosis (PVT) secondary to HCC invasion is of paramount importance since it preclude a therapeutic approach[16]. Non-tumor PVT has usually a similar appearance to portal vein tumor thrombosis, the last could enhance with contrast or have Doppler sign, however sometimes this differentiation is difficult and the diagnosis remains doubtful until proven otherwise. Although percutaneous US-guided FNA of a PVT has been well documented[17], this technique presents some difficulties, especially in accessing thrombus in the centrally located main portal vein. The EUS-FNA could overcome some limitations of a percutaneous US-guided FNA, as it provides an excellent view of the liver hilum which facilitates the puncture of a PVT. Some case reports have been published which the EUS-FNA was used to diagnose HCC in patients with portal vein thrombosis[18-21]. In two cases the procedure was performed with a 25-gauge needle[18,19], while the other cases were performed with a 22-gauge needle[20,21] and all patient have tolerated the procedure well, without any immediate or delayed complications.
After a careful study and analysis of these articles we can easily conclude that the EUS and EUS-FNA may be helpful in the management of a subset of patients with a high suspicion for small liver lesions and to approach lesions that remain difficult to sample by percutaneous US-guided techniques. However some important issues remain unanswered[22,23], the risk of needle track spread of HCC from EUS-FNA remains undefined and the quality of the visualization of peripheral lesions, such as the areas under the dome of the diaphragm and the inferior-posterior portion of the right lobe of the liver.
Other potential concerns are related to the risks associated with EUS-FNA. In a large international survey[24], in which centres with large experience participated, the EUS-FNA of the liver lesions, in expert hands, proved to be a safe procedure. The complication rate was 4%, although this included one major complication (death) and several minor complications (bleeding, infection, abdominal pain). The dead occurred in a patient with a pancreatic mass. The patient was suspected to have an occluded biliary stent at the time of the EUS and a cholangitis resulted from the introduction of bacteria into an obstructed bile duct by the needle. For this reason it is recommended that antibiotics are administered prophylactically and biliary drainage is established rapidly if fine needle aspiration of the liver is to be performed in the setting of obstructive jaundice. Despite these results more information about the risks and complications in specific groups is necessary, especially in patients with a particular propensity for liver lesions, such as patients with cirrhosis or portal hypertension. Prospective studies comparing the accuracy and complication rate of the EUS-FNA and percutaneous FNA techniques for the diagnosis of liver tumors are also still needed.
The therapy of HCC guided by EUS has also been reported in some case reports. In 2011, Di Matteo et al[25] reported a case of a hepatocellular carcinoma located in the caudate lobe unsuitable for surgical resection, liver transplant and percutaneous treatment. The embolization failed and an EUS-guided neodymium:Yttrium-aluminium-garnet (Nd: YAG) laser ablation was performed. The ablation of hepatocellular carcinoma was effective without adverse events. Nakaji et al[26] reported another case of EUS-guided hepatocellular carcinoma treatment this time with ethanol injection. These two cases have shown the significant innovative options to treat lesions that are difficult to reach by conventional methods.
Gastroesophageal varices are the most important portosystemic collaterals that can be developed as a consequence of portal hypertension[27]. The venous anatomy of the lower esophagus and stomach in patients with portosystemic collaterals is complex. The dilated submucosal veins can be readily seen during an upper endoscopy. This superficial venous plexus is connected, through the perforating vessels, with the deep venous plexus, periesophageal and paraesophageal veins[28].
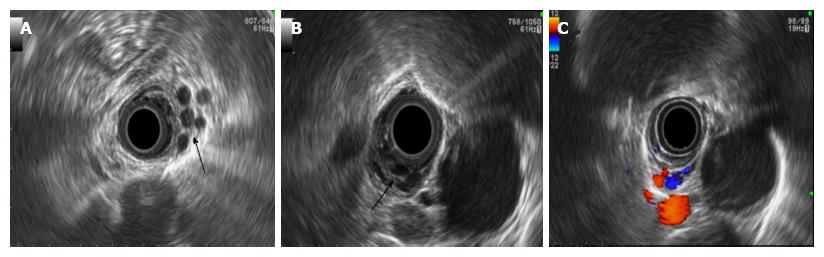
The endoscopic and ultrasound images provided by the EUS allows the visualization of the collateral vessels within and outside the esophageal wall[29-31] (Figure 2), and its role in the diagnosis and management of gastroesophageal varices is now well established.
In a study by Faigel et al[32] the presence and diameter of varices surrounding the esophagus and proximal stomach (paraesophageal and paragastric varices) were correlated with the presence and degree of liver disease and portal hypertension and represented a risk factor for variceal bleeding.
Since the previous reports about the role of collaterals in patients with portal hypertension and its clinical significance, some studies have analyzed the role of the EUS in the evaluation of the outcome of endoscopic therapeutics for esophageal varices, thereby allowing the selection of these patients for more intensive therapy or follow-up[33].
Endoscopic band ligation (EBL) has become the preferred method of treatment for esophageal varices, as it has proved to be as effective as injection sclerotherapy with fewer serious adverse events[34], however the risks of recurrence and rebleeding still remain a concern.
Recently, Masalaite et al[35] have assessed the role of the EUS in predicting the recurrence of esophageal varices following EBL. The study has shown that the presence of severe or multiple periesophageal collateral veins were independent prognostic factors for variceal recurrence. Similar results have been previously reported[36-38].
The effects of sclerotherapy and EBL on esophageal varices are considered to be different, which might be explained by different results of each technique in the ablation of collateral veins.
Lo et al[39] conducted a study to access the correlation between paraesophageal varices and esophageal variceal recurrence/rebleeding in patients who underwent sclerotherapy and EBL. Patients with more severe paraesophageal varices have presented a significantly higher rate of variceal recurrence and rebleeding. The prevalence of paraesophageal varices was 86% in the EBL group compared to 51% in the sclerotherapy group (P = 0.002).
In a study by de Paulo et al[40], the EUS was used to guide sclerotherapy for esophageal varices and although no significant benefit was found in the EUS-guided sclerotherapy in relation to the mean number of sessions necessary for eradication, the presence of collateral vessels, associated with bleeding recurrence, was less frequent in the EUS-guided group.
A possible explanation for these results could be appointed as the sclerotherapy causes fibrosis and obliteration of the perforating veins, while during EBL collateral vessels, in deeper layers, could remain untouched.
In order to identify factors that contributed to recurrence of varices and bleeding after endoscopic treatment some authors have also used color Doppler EUS. The association of Doppler to ultrasound images obtained by EUS allows both the visualization of varices and its collaterals and the understanding of the hemodynamics of the portal venous system and even the effects of endoscopic and pharmacological therapeutics for esophageal varices[41]. In a study by Hino et al[42] the color Doppler EUS was used to study the hemodynamics changes and morphology pattern of the left gastric vein (the main feeder vessel of esophageal varices). The hepatofugal flow velocity in the left gastric vein was studied in 31 patients with high risk esophageal varices. This study has demonstrated that patients showing anterior branch dominant pattern of left gastric vein and high hepatofugal flow velocity may present a high risk of an early recurrence of esophageal varices. Posteriorly, these results were validated by the same authors in a larger study of 68 patients[43].
The Table 3 summarizes the reports about the role of EUS in the evaluation of the outcome of endoscopic therapeutics for esophageal varices.
| Ref. | Study design | Endoscopic findings | EUS findings |
| Masalaite et al[35] | Prospective The role of EUS in predicting the recurrence/rebleeding of esophageal varices: EBL (n = 40) | Recurrence of esophageal varices: 19 (47.5%) within 12 mo of EBL | EUS independent prognostic factors for variceal recurrence: Severe esophageal collaterals (OR= 24.39) multiple esophageal collaterals (OR = 24.39) |
| Lo et al[39] | Prospective The role of EUS in predicting the recurrence of esophageal varices: ES (n = 35) vs EBL (n = 44) | Recurrence of esophageal varices: 43% ES vs 70% EBL | Paraesophageal varices: 51% ES vs 86% EBL |
| de Paulo et al[40] | Prospective The role of EUS-guided ES: ES (n = 25) vs EUS-guided ES (n = 25) of esophageal collateral vessels | Mean number of sessions until eradication: 4.3 ES group vs 4.1 for the EUS-ES Recurrence of esophageal varices: 16.7% ES vs 8.3% EUS-ES | Esophageal collaterals at the end of the sclerotherapy program: 8 patients in ES vs 0 patients in EUS-ES |
Currently, there are no specific recommendations for the EUS in the diagnosis or treatment management of patients with esophageal varices. However, the previously reported studies report information that may be important for the selection of optimal treatment for esophageal varices. The identification of collateral veins after endoscopic treatment would allow us to identify patients who are at higher risk of variceal recurrence and rebleeding and to select those who require a closer follow-up and even a more aggressive endoscopic approach.
Gastric varices occur in approximately 17% of patients with portal hypertension[44]. The endoscopic diagnosis of high risk for bleeding of gastric varices is not always easy to assess, and sometimes they are mistaken for large gastric folds or submucosal tumors. The magnetic resonance and CT allow the visualization of the entire portal venous system, however the accuracy of these techniques in distinguishing between submucosal gastric varices and perigastric collateral veins remains limited[41].
The EUS equipped with Doppler can significantly improve the detection of gastric varices and the understanding of the feeding vein, according to each type and the evaluation of vascular blood flow, which could be important in defining the therapeutic strategy[45,46]. With EUS-Color Doppler, Iwase et al[47] visualized small gastric varices that were difficult to detect by endoscopic observation, and were able to identify the feeding vein for each type of gastric varices. In a recent study by Imamura et al[48] the gastric varices diameter, which was independent from endoscopic view, Child-Pugh classification and the presence of hepatocellular carcinoma, have been correlated with flow volume measured by the EUS.
Sato et al[49] have also studied the role of the EUS-Color Doppler in the diagnosis and prediction of bleeding risk of gastric varices. The EUS-Color Doppler has allowed a clear sonographic visualization of the gastric varices and the evaluation of its morphology. In addition, the authors have showed that a smaller thickness of the gastric wall was a significant predictor of a high bleeding risk.
The presence of isolated gastric varices without esophageal varices can also be observed in patients with non-cirrhotic portal hypertension, which can occur in patients with splenic vein obstruction (left-sided portal hypertension). The role of the EUS color Doppler in patients with isolated gastric varices related to splenic vein occlusion has also been studied by Sato et al[50]. In this study the authors have provide specific findings that may be regarded as hallmarks of gastric varices due to splenic vein occlusion, namely a flow clearly depicted a round fundal region at the centre, with varices expanding to the curvatura major of the gastric body.
Endoscopic procedures, mainly the injection of tissue adhesives, such as cyanoacrylate (CYA), have become the therapy of choice for the treatment of gastric varices[51], although it is known to be associated with risk of clinical adverse events[52]. An innovative endoscopic option for the management of gastric varices includes the EUS-guided therapy.
The EUS can not only provide a clear image of the varix lumen, but also of the main feeding vein, and thus guiding the treatment directly to the perforating feeder vessel, which may theoretically minimize the amount of CYA needed to achieve the obliteration of gastric varices.
In a small study conducted by Romero-Castro et al[53] the EUS was used to guide the CYA injection in gastric varices. The EUS-guided CYA injection at the entrance of the perforating veins was successful in eradicating gastric varices in all the 5 patients treated, without recurrent bleeding or other subsequent complications. The authors have reported that the most difficult and time-consuming issue was the identification of the perforating vein of gastric varices and rule out what would be the outflowing vein. To be sure that the targeted vessel was the perforator, they carefully displayed the vascular anatomy by EUS and checked by fluoroscopy that the CYA-lipiodol mixture would not go downstream if an outflowing vein was mistakenly punctured.
Despite the reported success of the EUS-guided CYA injection, the concerns about the risks of embolization still remain. In a study by Binmoeller et al[54], coils, that are currently used for intravascular embolization treatments, were delivered into the varix under the EUS-guidance and previous to CYA injection, in order to reduce or eliminate the risk of glue embolization. The procedure was successful in all patients (thirty patients) with immediate hemostasis achieved in patients with active gastric varices bleeding (two patients). There was no damage to the echoendoscope, related to glue injections and non-procedure-related complications
In a multicentre study by Romero-Castro et al[55], EUS-guided coil application vs cyanoacrylate for the embolization of feeding gastric varices was studied. Thirty patients, 11 patients in the coil group and 19 patients in cyanoacrylate group, were included. Both techniques were effective in the gastric variceal obliteration. However coil application required fewer endoscopies and tended to have fewer adverse events.
An advantage of the EUS-guided treatment is the lack of dependency on direct varix visualization. In a case study reported by Tang et al[56] the point of rebleeding of a fundal gastric varices, which was persistently obscured due to ongoing bleeding and blood clots, was identified by the EUS, followed by CYA injection and real-time Doppler confirmation of vascular signal loss in gastric varices.
Transesophageal EUS-guided coil or CYA injection of gastric varices is feasible and deserves further studies to determine whether these approaches can improve safety and efficiency over standard endoscopic injection of CYA alone. Although the EUS-guided gastric variceal therapy offers many potential advantages, a review by Fujii-Lau et al[46] lists several pitfalls that should be considered before applying the technique, such as the risk of damage the echoendoscope if glue lodged within the channel, the smaller aspiration channel, compared to a therapeutic endoscope, which could be important in cases of active bleeding, the limited retroflexion of the echoendoscope making the approximation to the fundal mucosa difficult, the importance of a fluoroscopy guidance to monitor for the immediate embolization and the complexity of the entire procedure making it time-consuming.
Portal hypertension is a common adverse event of liver cirrhosis as this syndrome develops in the majority of patients with cirrhosis being responsible for severe complications such as gastrointestinal variceal bleeding, ascites, hepatorenal syndrome and hepatic encephalopathy[57]. The hepatic venous pressure gradient, an acceptable indirect measurement of portal pressure, predicts the development of complications of portal hypertension[58], whilst its use has also been proposed in the evaluation of the efficacy of pharmacological therapeutics in patients with portal hypertension[59]. Hepatic venous pressure gradient is traditionally measured by a transjugular approach, an invasive procedure, with radiation and intravenous contrast exposure and not readily available in all centres. The EUS-Guided portal vein catheterization for direct portal pressure measurement has been reported in some studies.
The possibility of direct EUS-guided portal vein catheterization using a 25-gauge needle and accurate pressure measurement has been demonstrated in animal models. In a study by Huang et al[60] a novel EUS-guided system using a 25-gauge FNA needle (Cook® Medical, Winston-Salem, NC, United States), and a compact manometer with non-compressible tubing (Cook® Medical, Bloomington, Ind, United States) has been used to directly measure portal pressure gradient and to evaluate its performance and clinical feasibility. Under the EUS guidance a 25-gauge FNA needle with attached manometer has been used to puncture (transgastric-transhepatic approach) and to measure pressures in the portal vein, right hepatic vein, inferior vena cava, and aorta in 3 animal models and the results were correlated with the standard transjugular approach. There has been an excellent correlation between the two methods and no adverse events have been reported. Recently, the same group[61] has presented the first human pilot study of the EUS-guided portal pressure gradient measurement (EUS-PPGM) in patients with liver disease. The procedure has been performed with a linear echoendoscope and the same equipment previously described. Twenty-eight patients underwent EUS-PPGM, 15 of 28 (57.1%) had evidence of portal hypertension based on portal pressure gradient of which 10 of 15 (66.7%) had clinical significant portal hypertension. There has been an excellent association between portal pressure gradient and clinical evidence of cirrhosis, presence of varices, portal hypertensive gastropathy and thrombocytopenia. There have not been technical failures or reported intraprocedural or post-procedural adverse events. This was the first study demonstrating that the EUS-PPGM can be safe and accurate in humans, even in the context of suspected cirrhosis.
The EUS-guided measurements of portal pressure gradient provide an alternative method to evaluate portal hemodynamics. More studies are still needed, mainly in cirrhotic patients with impaired hemostasis, and therefore there is a possibility to use this new method to evaluate the effect of pharmacological therapy on portal hypertension.
There is evidence to suggest that the EUS alone or with FNA represent a significant advance in the evaluation and treatment of liver diseases and its complications. The EUS is able to provide an early detection and the biopsy of small focal liver lesions that are either not visualized by other imaging modalities or visualized during routine staging procedures of gastrointestinal malignancies. Thus, the EUS is another potential method for a guided liver biopsy for study parenchymal liver disease.
The EUS proves to be really helpful in managing portal hypertension being used to stratify patients who are at risk of recurrence and rebleeding of gastroesophageal varices and providing support for more aggressive therapy with frequent endoscopic treatments including direct treatment to the perforating veins. Concerning gastric varices, it can be used to guide cyanoacrylate injection in an effort to achieve total occlusion of the varices and decrease the recurrence rate and complications.
More recently, the EUS has been described as a method for guiding interventions such as portal vein catheterization for direct portal pressure measurement. However most of the studies in this field are performed in animal models, and safety date in humans, mainly cirrhotic patients, are still lacking.
The diagnostic and therapeutic role of EUS in hepatology is emerging and the available evidence suggests that the EUS has the potential to be a valuable alternative imaging modality in the study of liver diseases and its complications. Several methods are still under development and need to be validated, but the authors expect that in the near future applications of the EUS in hepatology will become an integral part of the evaluation of patients with liver diseases.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Portugal
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cui J, Kim GH, Sato T S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Luthra AK, Evans JA. Review of current and evolving clinical indications for endoscopic ultrasound. World J Gastrointest Endosc. 2016;8:157-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Rameshbabu CS, Wani ZA, Rai P, Abdulqader A, Garg S, Sharma M. Standard imaging techniques for assessment of portal venous system and its tributaries by linear endoscopic ultrasound: a pictorial essay. Endosc Ultrasound. 2013;2:16-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 3. | Bhatia V, Hijioka S, Hara K, Mizuno N, Imaoka H, Yamao K. Endoscopic ultrasound description of liver segmentation and anatomy. Dig Endosc. 2014;26:482-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | European Association for Study of Liver; Asociacion Latinoamericana para el Estudio del Higado. EASL-ALEH Clinical Practice Guidelines: Non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63:237-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1177] [Cited by in RCA: 1332] [Article Influence: 133.2] [Reference Citation Analysis (0)] |
| 5. | Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD; American Association for the Study of Liver Diseases. Liver biopsy. Hepatology. 2009;49:1017-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1449] [Cited by in RCA: 1581] [Article Influence: 98.8] [Reference Citation Analysis (1)] |
| 6. | Shiha G, Ibrahim A, Helmy A, Sarin SK, Omata M, Kumar A, Bernstien D, Maruyama H, Saraswat V, Chawla Y. Asian-Pacific Association for the Study of the Liver (APASL) consensus guidelines on invasive and non-invasive assessment of hepatic fibrosis: a 2016 update. Hepatol Int. 2017;11:1-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 170] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 7. | Gleeson FC, Clayton AC, Zhang L, Clain JE, Gores GJ, Rajan E, Smyrk TC, Topazian MD, Wang KK, Wiersema MJ. Adequacy of endoscopic ultrasound core needle biopsy specimen of nonmalignant hepatic parenchymal disease. Clin Gastroenterol Hepatol. 2008;6:1437-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Dewitt J, McGreevy K, Cummings O, Sherman S, Leblanc JK, McHenry L, Al-Haddad M, Chalasani N. Initial experience with EUS-guided Tru-cut biopsy of benign liver disease. Gastrointest Endosc. 2009;69:535-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 9. | Sey MS, Al-Haddad M, Imperiale TF, McGreevy K, Lin J, DeWitt JM. EUS-guided liver biopsy for parenchymal disease: a comparison of diagnostic yield between two core biopsy needles. Gastrointest Endosc. 2016;83:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 10. | Stavropoulos SN, Im GY, Jlayer Z, Harris MD, Pitea TC, Turi GK, Malet PF, Friedel DM, Grendell JH. High yield of same-session EUS-guided liver biopsy by 19-gauge FNA needle in patients undergoing EUS to exclude biliary obstruction. Gastrointest Endosc. 2012;75:310-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 11. | Diehl DL, Johal AS, Khara HS, Stavropoulos SN, Al-Haddad M, Ramesh J, Varadarajulu S, Aslanian H, Gordon SR, Shieh FK. Endoscopic ultrasound-guided liver biopsy: a multicenter experience. Endosc Int Open. 2015;3:E210-E215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 12. | Pineda JJ, Diehl DL, Miao CL, Johal AS, Khara HS, Bhanushali A, Chen EZ. EUS-guided liver biopsy provides diagnostic samples comparable with those via the percutaneous or transjugular route. Gastrointest Endosc. 2016;83:360-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 94] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 13. | Awad SS, Fagan S, Abudayyeh S, Karim N, Berger DH, Ayub K. Preoperative evaluation of hepatic lesions for the staging of hepatocellular and metastatic liver carcinoma using endoscopic ultrasonography. Am J Surg. 2002;184:601-604; discussion 604-605. [PubMed] |
| 14. | Singh P, Erickson RA, Mukhopadhyay P, Gopal S, Kiss A, Khan A, Ulf Westblom T. EUS for detection of the hepatocellular carcinoma: results of a prospective study. Gastrointest Endosc. 2007;66:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | DeWitt J, LeBlanc J, McHenry L, Ciaccia D, Imperiale T, Chappo J, Cramer H, McGreevy K, Chriswell M, Sherman S. Endoscopic ultrasound-guided fine needle aspiration cytology of solid liver lesions: a large single-center experience. Am J Gastroenterol. 2003;98:1976-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Bruix J, Reig M, Sherman M. Evidence-Based Diagnosis, Staging, and Treatment of Patients With Hepatocellular Carcinoma. Gastroenterology. 2016;150:835-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1024] [Cited by in RCA: 1276] [Article Influence: 141.8] [Reference Citation Analysis (2)] |
| 17. | Tarantino L, Francica G, Sordelli I, Esposito F, Giorgio A, Sorrentino P, de Stefano G, Di Sarno A, Ferraioli G, Sperlongano P. Diagnosis of benign and malignant portal vein thrombosis in cirrhotic patients with hepatocellular carcinoma: color Doppler US, contrast-enhanced US, and fine-needle biopsy. Abdom Imaging. 2006;31:537-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 116] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 18. | Michael H, Lenza C, Gupta M, Katz DS. Endoscopic Ultrasound -guided Fine-Needle Aspiration of a Portal Vein Thrombus to Aid in the Diagnosis and Staging of Hepatocellular Carcinoma. Gastroenterol Hepatol (N Y). 2011;7:124-129. [PubMed] |
| 19. | Lai R, Stephens V, Bardales R. Diagnosis and staging of hepatocellular carcinoma by EUS-FNA of a portal vein thrombus. Gastrointest Endosc. 2004;59:574-577. [PubMed] |
| 20. | Moreno M, Gimeno-García AZ, Corriente MM, Nicolás-Pérez D, Brito-García A, García-Castro C, Quintero E. EUS-FNA of a portal vein thrombosis in a patient with a hidden hepatocellular carcinoma: confirmation technique after contrast-enhanced ultrasound. Endoscopy. 2014;46 Suppl 1 UCTN:E590-E591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Storch I, Gomez C, Contreras F, Schiff E, Ribeiro A. Hepatocellular carcinoma (HCC) with portal vein invasion, masquerading as pancreatic mass, diagnosed by endoscopic ultrasound-guided fine needle aspiration (EUS-FNA). Dig Dis Sci. 2007;52:789-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Thuluvath PJ. EUS-guided FNA could be another important tool for the early diagnosis of hepatocellular carcinoma. Gastrointest Endosc. 2007;66:274-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Maheshwari A, Kantsevoy S, Jagannath S, Thuluvath PJ. Endoscopic ultrasound and fine-needle aspiration for the diagnosis of hepatocellular carcinoma. Clin Liver Dis. 2010;14:325-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | tenBerge J, Hoffman BJ, Hawes RH, Van Enckevort C, Giovannini M, Erickson RA, Catalano MF, Fogel R, Mallery S, Faigel DO. EUS-guided fine needle aspiration of the liver: indications, yield, and safety based on an international survey of 167 cases. Gastrointest Endosc. 2002;55:859-862. [PubMed] |
| 25. | Di Matteo F, Grasso R, Pacella CM, Martino M, Pandolfi M, Rea R, Luppi G, Silvestri S, Zardi E, Costamagna G. EUS-guided Nd:YAG laser ablation of a hepatocellular carcinoma in the caudate lobe. Gastrointest Endosc. 2011;73:632-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 26. | Nakaji S, Hirata N, Iwaki K, Shiratori T, Kobayashi M, Inase M. Endoscopic ultrasound (EUS)-guided ethanol injection for hepatocellular carcinoma difficult to treat with percutaneous local treatment. Endoscopy. 2012;44 Suppl 2 UCTN:E380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1441] [Article Influence: 180.1] [Reference Citation Analysis (3)] |
| 28. | El-Saadany M, Jalil S, Irisawa A, Shibukawa G, Ohira H, Bhutani MS. EUS for portal hypertension: a comprehensive and critical appraisal of clinical and experimental indications. Endoscopy. 2008;40:690-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Choudhuri G, Dhiman RK, Agarwal DK. Endosonographic evaluation of the venous anatomy around the gastro-esophageal junction in patients with portal hypertension. Hepatogastroenterology. 1996;43:1250-1255. [PubMed] |
| 30. | Irisawa A, Shibukawa G, Obara K, Saito A, Takagi T, Shishido H, Odajima H, Abe M, Sugino T, Suzuki T. Collateral vessels around the esophageal wall in patients with portal hypertension: comparison of EUS imaging and microscopic findings at autopsy. Gastrointest Endosc. 2002;56:249-253. [PubMed] |
| 31. | Caletti G, Brocchi E, Baraldini M, Ferrari A, Gibilaro M, Barbara L. Assessment of portal hypertension by endoscopic ultrasonography. Gastrointest Endosc. 1990;36:S21-S27. [PubMed] |
| 32. | Faigel DO, Rosen HR, Sasaki A, Flora K, Benner K. EUS in cirrhotic patients with and without prior variceal hemorrhage in comparison with noncirrhotic control subjects. Gastrointest Endosc. 2000;52:455-462. [PubMed] |
| 33. | Masalaite L, Valantinas J, Stanaitis J. The role of collateral veins detected by endosonography in predicting the recurrence of esophageal varices after endoscopic treatment: a systematic review. Hepatol Int. 2014;8:339-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1229] [Cited by in RCA: 1210] [Article Influence: 67.2] [Reference Citation Analysis (0)] |
| 35. | Masalaite L, Valantinas J, Stanaitis J. Endoscopic ultrasound findings predict the recurrence of esophageal varices after endoscopic band ligation: a prospective cohort study. Scand J Gastroenterol. 2015;50:1322-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 36. | Leung VK, Sung JJ, Ahuja AT, Tumala IE, Lee YT, Lau JY, Chung SC. Large paraesophageal varices on endosonography predict recurrence of esophageal varices and rebleeding. Gastroenterology. 1997;112:1811-1816. [PubMed] |
| 37. | Kume K, Yamasaki M, Watanabe T, Yoshikawa I, Otsuki M, Harada M. Mild collateral varices and a fundic plexus without perforating veins on EUS predict endoscopic non-recurrence of esophageal varices after EVL. Hepatogastroenterology. 2011;58:798-801. [PubMed] |
| 38. | Konishi Y, Nakamura T, Kida H, Seno H, Okazaki K, Chiba T. Catheter US probe EUS evaluation of gastric cardia and perigastric vascular structures to predict esophageal variceal recurrence. Gastrointest Endosc. 2002;55:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 39. | Lo GH, Lai KH, Cheng JS, Huang RL, Wang SJ, Chiang HT. Prevalence of paraesophageal varices and gastric varices in patients achieving variceal obliteration by banding ligation and by injection sclerotherapy. Gastrointest Endosc. 1999;49:428-436. [PubMed] |
| 40. | de Paulo GA, Ardengh JC, Nakao FS, Ferrari AP. Treatment of esophageal varices: a randomized controlled trial comparing endoscopic sclerotherapy and EUS-guided sclerotherapy of esophageal collateral veins. Gastrointest Endosc. 2006;63:396-402; quiz 463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 41. | Sato T, Yamazaki K. Endoscopic color Doppler ultrasonography for esophagogastric varices. Diagn Ther Endosc. 2012;2012:859213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Hino S, Kakutani H, Ikeda K, Yasue H, Kitamura Y, Sumiyama K, Uchiyama Y, Kuramochi A, Matsuda K, Arakawa H. Hemodynamic analysis of esophageal varices using color Doppler endoscopic ultrasonography to predict recurrence after endoscopic treatment. Endoscopy. 2001;33:869-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 43. | Kuramochi A, Imazu H, Kakutani H, Uchiyama Y, Hino S, Urashima M. Color Doppler endoscopic ultrasonography in identifying groups at a high-risk of recurrence of esophageal varices after endoscopic treatment. J Gastroenterol. 2007;42:219-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 44. | Garcia-Pagán JC, Barrufet M, Cardenas A, Escorsell A. Management of gastric varices. Clin Gastroenterol Hepatol. 2014;12:919-928.e1; quiz e51-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 103] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 45. | Boustière C, Dumas O, Jouffre C, Letard JC, Patouillard B, Etaix JP, Barthélémy C, Audigier JC. Endoscopic ultrasonography classification of gastric varices in patients with cirrhosis. Comparison with endoscopic findings. J Hepatol. 1993;19:268-272. [PubMed] |
| 46. | Fujii-Lau LL, Law R, Wong Kee Song LM, Levy MJ. Novel techniques for gastric variceal obliteration. Dig Endosc. 2015;27:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 47. | Iwase H, Suga S, Morise K, Kuroiwa A, Yamaguchi T, Horiuchi Y. Color Doppler endoscopic ultrasonography for the evaluation of gastric varices and endoscopic obliteration with cyanoacrylate glue. Gastrointest Endosc. 1995;41:150-154. [PubMed] |
| 48. | Imamura H, Irisawa A, Shibukawa G, Takagi T, Hikichi T, Obara K, Ohira H. Echo-endoscopic analysis of variceal hemodynamics in patient with isolated gastric varices. Endosc Ultrasound. 2014;3:238-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 49. | Sato T, Yamazaki K, Toyota J, Karino Y, Ohmura T, Akaike J. Observation of gastric variceal flow characteristics by endoscopic ultrasonography using color Doppler. Am J Gastroenterol. 2008;103:575-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 50. | Sato T, Yamazaki K, Kimura M, Toyota J, Karino Y. Endoscopic Color Doppler Ultrasonographic Evaluation of Gastric Varices Secondary to Left-Sided Portal Hypertension. Diagnostics (Basel). 2014;4:94-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 51. | Koch D. Update in the management of gastric varices. Curr Opin Gastroenterol. 2016;32:166-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 52. | Cheng LF, Wang ZQ, Li CZ, Lin W, Yeo AE, Jin B. Low incidence of complications from endoscopic gastric variceal obturation with butyl cyanoacrylate. Clin Gastroenterol Hepatol. 2010;8:760-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 124] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 53. | Romero-Castro R, Pellicer-Bautista FJ, Jimenez-Saenz M, Marcos-Sanchez F, Caunedo-Alvarez A, Ortiz-Moyano C, Gomez-Parra M, Herrerias-Gutierrez JM. EUS-guided injection of cyanoacrylate in perforating feeding veins in gastric varices: results in 5 cases. Gastrointest Endosc. 2007;66:402-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 127] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 54. | Binmoeller KF, Weilert F, Shah JN, Kim J. EUS-guided transesophageal treatment of gastric fundal varices with combined coiling and cyanoacrylate glue injection (with videos). Gastrointest Endosc. 2011;74:1019-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 169] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 55. | Romero-Castro R, Ellrichmann M, Ortiz-Moyano C, Subtil-Inigo JC, Junquera-Florez F, Gornals JB, Repiso-Ortega A, Vila-Costas J, Marcos-Sanchez F, Muñoz-Navas M. EUS-guided coil versus cyanoacrylate therapy for the treatment of gastric varices: a multicenter study (with videos). Gastrointest Endosc. 2013;78:711-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 158] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 56. | Tang RS, Teoh AY, Lau JY. EUS-guided cyanoacrylate injection for treatment of endoscopically obscured bleeding gastric varices. Gastrointest Endosc. 2016;83:1032-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 57. | Bosch J, García-Pagán JC. Complications of cirrhosis. I. Portal hypertension. J Hepatol. 2000;32:141-156. [PubMed] |
| 58. | La Mura V, Nicolini A, Tosetti G, Primignani M. Cirrhosis and portal hypertension: The importance of risk stratification, the role of hepatic venous pressure gradient measurement. World J Hepatol. 2015;7:688-695. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 59. | Addley J, Tham TC, Cash WJ. Use of portal pressure studies in the management of variceal haemorrhage. World J Gastrointest Endosc. 2012;4:281-289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 60. | Huang JY, Samarasena JB, Tsujino T, Chang KJ. EUS-guided portal pressure gradient measurement with a novel 25-gauge needle device versus standard transjugular approach: a comparison animal study. Gastrointest Endosc. 2016;84:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 65] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 61. | Huang JY, Samarasena JB, Tsujino T, Lee J, Hu KQ, McLaren CE, Chen WP, Chang KJ. EUS-guided portal pressure gradient measurement with a simple novel device: a human pilot study. Gastrointest Endosc. 2017;85:996-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 130] [Article Influence: 16.3] [Reference Citation Analysis (0)] |