Published online Mar 16, 2017. doi: 10.4253/wjge.v9.i3.145
Peer-review started: November 15, 2016
First decision: December 1, 2016
Revised: December 13, 2016
Accepted: January 11, 2017
Article in press: January 14, 2017
Published online: March 16, 2017
Processing time: 121 Days and 23.3 Hours
A 63-year-old man presented at our hospital with right upper abdomen pain and fever for 4 d. The patient’s magnetic resonance cholangiopancreatography revealed dilated common bile duct and choledocholithiasis. In his past history, he received proximal gastrectomy and modified double tracks anastomosis. Endoscopic retrograde cholangiopancretography in modified double tracks anastomosis, especially accompanied with anastomotic stenosis, has been rarely reported. In the present case, the duodenoscope was successfully introduced over the guidewire and the stone taken out using a basket. The patient had good palliation of his symptoms after removal of the stone.
Core tip: It has been quite difficult to carry out conventional endoscopic retrograde cholangiopancretography (ERCP) for pancreatobiliary diseases in patients with modified double tracks anastomosis after proximal gastrectomy. Thus, this procedure posed a great challenge to the endoscopist. After confirming the long limb, we chose to go back to the cabined anastomosis and switched the gastroscope for the duodenoscope. For safety, the endoscope that went into the residual stomach across the gastrojejunal anastomosis was introduced by guidewire. Finally, we successfully carried out the ERCP and removed the stone.
- Citation: Wang XS, Wang F, Li QP, Miao L, Zhang XH. Endoscopic retrograde cholangiopancretography in modified double tracks anastomosis with anastomotic stenosis. World J Gastrointest Endosc 2017; 9(3): 145-148
- URL: https://www.wjgnet.com/1948-5190/full/v9/i3/145.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i3.145
Endoscopic retrograde cholangiopancretography (ERCP) has been widely applied to pancreatobiliary diseases in recent years. The success rate is 90%-95%[1]. However, it is quite difficult to carry out conventional ERCP for pancreatobiliary diseases in patients with surgically altered gastrointestinal anatomy[2]. Patients with altered anatomy, such as those with a Billroth II gastrojejunostomy or a biliodigestive anastomosis with Roux-en-Y reconstruction, pose serious challenges to the endoscopist when access to the biliary system is required.
With the development of endoscopy, the technology of ERCP has improved greatly. Many modified methods of ERCP, including double-balloon enteroscope (DBE), single-balloon enteroscope (SBE) and spiral enteroscope (SE), have been applied in the clinic. However, deep endoscopic options, including DBE, SBE, SE and any of those modalities, were used mainly according to the preference of the endoscopist. This case with modified double tracks anastomosis after proximal gastrectomy, especially accompanied with anastomotic stenosis, is rarely encountered; thus, it poses a great challenge to the endoscopist. We finally successfully carried out the ERCP and removed the stone in such a challenging case.
A 63-year-old man presented at our hospital with right abdomen pain and fever for 4 d. He had radiating pain in his lower back, fever to 38 °C, nausea without vomiting, icteric sclera, and yellow urine. On admission, his general appearance was acute ill looking and there was tenderness on the right upper quadrant of the abdomen. Cardiac and respiratory examination was unremarkable. Laboratory findings were as follows: white blood cell, 8.600/mm3 (normal, 4-10/mm3); neutrophil percentage, 84.9% (normal, 50%-70%); total bilirubin, 21 g/L (normal, 1-10 g/L); direct bilirubin, 12 g/L (normal, 1-4 g/L); aspartate aminotransferase, 54 U/L (normal, 0-37 U/L); alanine aminotransferase, 151 U/L (normal, 0-40 U/L); serum amylase, 779.2 U/L (normal, 40-110 U/L). Magnetic resonance cholangiopancreatography revealed dilated common bile duct and choledocholithiasis.
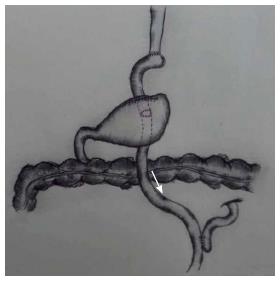
The patient’s medical history included receipt of proximal gastrectomy due to high grade intraepithelial neoplasia of gastric cardia in 2015. The small intestine was consequently rearranged into a Y-configuration, where one jejunal isoperistaltic limb was anastomosed to the distal esophagus and the other limb connected to the excluded stomach was reattached distally in an end-to-side fashion. Besides, the posterior wall of the gastric remnant had been made into a gastrojejunal anastomosis below the esophagojejunal anastomosis (Figure 1). As a result, there were two ways for food emptying between the esophagus and intestinal anastomosis, with the first including the distal esophagus, partial jejunum, remnant stomach and duodenum, and the second (called the “long limb”) including only the distal esophagus and partial jejunum. In addition, the patient had undergone cholecystectomy for gallbladder stones by laparoscopy 1 wk prior to presentation.
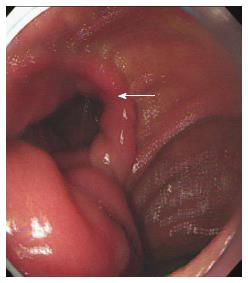
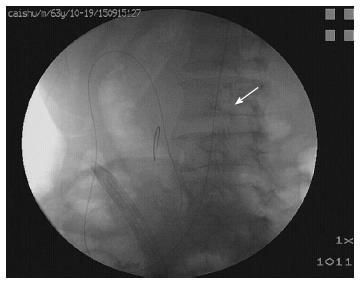
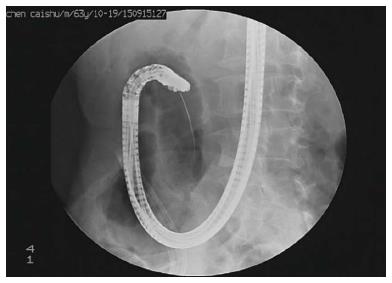
The patient was diagnosed with choledocholith, post-cholecystectomy and postoperative gastric cancer. ERCP was performed with a cap-assisted forward viewing endoscope (Olympus, Center Valley, PA, United States). When the endoscope passed the distal esophagus some distance, we found an anastomosis, but it was hard to pass the gastroscope (Figure 2). We continued the original way for some distance, until we found another anastomosis. We confirmed that this was the long limb and the stenosed anastomosis is the gastrojejunal anastomosis. Then, we chose to go back to the cabined anastomosis and switched the gastroscope for the duodenoscope (Olympus). For safety, the endoscope that went into the residual stomach across the gastrojejunal anastomosis was introduced by guidewire (JagwireTM, 0.035 in × 450 cm; Boston Scientific, Marlborough, MA, United States) (Figure 3). Then, we successfully arrived at the major papilla (Figure 4) and achieved a cholangiogram (Figure 5). At last, we removed the stone (diameter, 1.1 cm × 1.4 cm) using a stone-removal basket (Boston Scientific) and placed a nasobiliary stent of pig tail type (Boston Scientific) for drainage. Two days later, the patient’s symptoms were alleviated and he left the hospital to rehabilitation several days later.
ERCP is the first choice for the clinical diagnosis and treatment of biliary and pancreatic diseases currently. However, conventional ERCP in patients with surgically altered gastrointestinal anatomy is far more challenging because of the complicated angulation, the inability of the endoscope to reach the blind end (due to the long bowel passage) and the difficulty in identifying the afferent limb[3]. Considering the technical challenges in reaching the papilla and performing therapy in patients with surgically altered gastrointestinal anatomy, modified methods of ERCP were developed. A recent review, including over 945 procedures using DBE, SBE or SE with altered anatomy, found success rates of reaching the papilla were 80% in Roux-en-Y gastric bypass (RYGB) and 96% in Billroth II procedures; the rates of desired therapies performed were 70% in RYGB and 90% in Billroth II procedures. Moreover, the overall rate of complications of DBE, SBE and SE in patients is only 3.4%[4]. These methods have greatly helped endoscopists complete the operations.
Modified double tracks anastomosis have been used in the surgery of gastric cardia to improve the nutrition and reflux symptoms[5]. It is difficult to study, however, because the overall number of cases is still relatively low. Cases associated with anastomotic stenosis have been rarely reported, especially. The treatment options for the case presented herein included surgical operation, laparoscopic treatment and ERCP. Surgical operation and laparoscopy may impose an excessive burden on a debilitated patient, resulting in slower rehabilitation and bringing about more complications. In addition, a recent study has demonstrated that ERCP is effective in diagnosing and treating choledocholithiasis[6]. Our patient’s general situation was not good because he had undergone surgery for cholecystectomy to address gallbladder stones by laparoscopy 1 wk prior. Duodenoscopic treatment was, therefore, a better choice.
In the endoscopic treatment of the present case, the view of choosing the narrow anastomosis when we had affirmed the long limb was prudential. The way for passing the long limb to the major papilla was too long and had high risk of perforation[7]. However, we would have to try to get to the point of major papilla across the long limb if the anastomosis was too narrow to pass the duodenoscope.
Having reached the gastrojejunal anastomosis, we still faced some difficulties. Firstly, identification of the afferent limb to residual stomach in gastrojejunal anastomosis was very difficult, as it was secluded and an endoscopist could easily miss it. So, we were cautious to slowly move forward and observe the surrounding tissues carefully to find the gastrojejunal anastomosis. The second challenge was that proximal gastrectomy might result in post-surgical adhesion. Special care needed to be taken, and endoscopists should use discretion in withdrawal because of the high risk of bleeding and perforation. Last, but not least, the gastrojejunal anastomosis is relatively narrow and presents high risks of bleeding and perforation as well as post-surgical adhesion; so, we minimized the operative manipulation of the anastomosis. As such, we decided to directly replace the gastroscope with the duodenoscope. The endoscope was introduced by a guidewire through the anastomotic stenosis. Finally, we overcame the above challenges and successfully removed the stone.
Although a few cases of modified ERCP techniques in surgically altered gastrointestinal anatomy have been reported, this report of ERCP in proximal gastrectomy and modified double tracks anastomosis with anastomotic stenosis is rather rare. From this case, we learned that endoscopic treatment is feasible for this type of clinical situation. If a similar case is discovered, the above case report may be helpful to solve common challenges.
A 63-year-old man presented with right upper abdomen pain and fever that persisted for 4 d before he sought evaluation at the Second Affiliated Hospital of Nanjing Medical University.
The patient had undergone proximal gastrectomy with modified double tracks anastomosis due to high grade intraepithelial neoplasia of gastric cardia. After admission to the hospital, magnetic resonance cholangiopancreatography revealed dilated common bile duct and choledocholithiasis.
White blood cell, 8.600/mm3 (normal, 4-10/mm3); neutrophil percentage, 84.9% (normal, 50%-70%); total bilirubin, 21 g/L (normal, 1-10 g/L); direct bilirubin, 12 g/L (normal, 1-4 g/L); aspartate aminotransferase, 54 U/L (normal, 0-37 U/L); alanine aminotransferase, 151 U/L (normal, 0-40 U/L); serum amylase, 779.2 U/L (normal, 40-110 U/L).
Magnetic resonance cholangiopancreatography revealed dilated common bile duct and choledocholithiasis.
The duodenoscope was introduced over a guidewire and the stone was removed using a basket. The patient had good palliation of his symptoms several days later.
There is no related report about endoscopic retrograde cholangiopancretography in the modified double tracks anastomosis with anastomotic stenosis.
This report emphasizes the importance of understanding surgically altered gastrointestinal anatomy before surgery. Endoscopic treatment is feasible to this case.
This is an interesting case report and eventually needs to be published.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Mohamed AA, Imagawa A, Tovey FI S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc. 2005;61:112-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 224] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 2. | Shimatani M, Takaoka M, Matsushita M, Okazaki K. Endoscopic approaches for pancreatobiliary diseases in patients with altered gastrointestinal anatomy. Dig Endosc. 2014;26 Suppl 1:70-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Shimatani M, Takaoka M, Tokuhara M, Miyoshi H, Ikeura T, Okazaki K. Review of diagnostic and therapeutic endoscopic retrograde cholangiopancreatography using several endoscopic methods in patients with surgically altered gastrointestinal anatomy. World J Gastrointest Endosc. 2015;7:617-627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Skinner M, Popa D, Neumann H, Wilcox CM, Mönkemüller K. ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 2014;46:560-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 152] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 5. | Yabusaki H, Nashimoto A, Matsuki A. Evaluation of jejunal pouch interposition after proximal gastrectomy for early gastric cancer in the upper third of the stomach. Hepatogastroenterology. 2012;59:2032-2036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Lynn AP, Chong G, Thomson A. Endoscopic retrograde cholangiopancreatography in the treatment of intraoperatively demonstrated choledocholithiasis. Ann R Coll Surg Engl. 2014;96:45-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Prachayakul V, Aswakul P. Endoscopic retrograde cholangiopancreatography-related perforation: Management and prevention. World J Clin Cases. 2014;2:522-527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (2)] |