Published online May 10, 2016. doi: 10.4253/wjge.v8.i9.391
Peer-review started: January 12, 2016
First decision: February 2, 2016
Revised: February 17, 2016
Accepted: March 7, 2016
Article in press: March 9, 2016
Published online: May 10, 2016
Processing time: 118 Days and 20.2 Hours
Splenic rupture is a rare complication of diagnostic and therapeutic gastrointestinal endoscopy procedures. Herein, we report for the first time a case of splenic rupture following therapeutic retrograde double-balloon enteroscopy, which occurred in an 85-year-old man who was treated for recurrent mid-intestinal bleeding that resulted from ileal angioectasia. This patient promptly underwent an operation and eventually recovered.
Core tip: Splenic rupture is a rare, devastating complication of colonoscopy. For the first time, we report a case of splenic rupture following therapeutic retrograde double-balloon enteroscopy.
- Citation: Girelli CM, Pometta R, Facciotto C, Mella R, Bernasconi G. First report of splenic rupture following deep enteroscopy. World J Gastrointest Endosc 2016; 8(9): 391-394
- URL: https://www.wjgnet.com/1948-5190/full/v8/i9/391.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i9.391
Splenic rupture is a rare complication of gastrointestinal endoscopy. Although very few cases of splenic injuries have been reported following endoscopic retrograde cholangio pancreatography[1,2], immediate or delayed splenic injury and rupture have mostly been reported following diagnostic and therapeutic colonoscopy. To the best of our knowledge, 102 of such cases have been reported in the English language literature[3]. Deep enteroscopy (DE) is a relatively new endoscopic technique involving approach of the small bowel from an oral (antegrade DE) or aboral (retrograde DE) route. In contrast to small bowel capsule endoscopy (SBCE), DE is invasive, requires sedation and allows for endoscopic interventions (i.e., biopsy, tattooing, hemostasis, or polypectomy). In accordance with the European Society of Gastrointestinal Endoscopy guidelines[4], in the clinical setting of recurrent, overt mid-gastrointestinal bleeding, we perform DE to better characterize and/or treat lesions identified by other less invasive means, such as SBCE and/or cross-sectional imaging. DE can be performed with the aid of an overtube; currently, three different instruments are used: A single-balloon enteroscope, a double-balloon enteroscope (DBE) and a spiral enteroscope. To date, no case of splenic rupture has been reported following DE. Herein, we present the first such case, which occurred after a therapeutic retrograde DBE (R-DBE).
An 85-year-old Caucasian man was admitted to hospital in March 2015 because of gastrointestinal bleeding (bright red blood in his stools) and anemia (hemoglobin level of 7.7 g/dL). In 1998, he underwent aortic valve replacement with a mechanical prosthesis, with subsequent long-life warfarin (target INR of 3-4.5). Previously, 5 mo before his current admission, he was admitted because of overt gastrointestinal hemorrhage. Although an upper endoscopy was normal, colonoscopy revealed sigmoid diverticula and active bleeding resulting from a Dieulafoy lesion of the right flexure, which was successfully clipped.
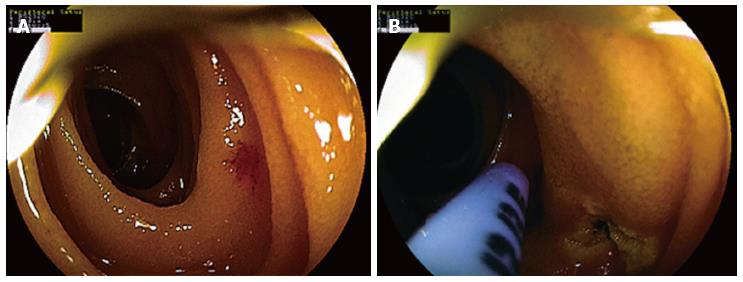
During this present instance of hospital admission, two units of packed red blood cells were administered. Urgent esophagogastroduodenoscopy and colonoscopy were performed without evidence of active bleeding. Therefore, the patient underwent SBCE (Pillcam SB3, Covidien, Ireland). At 3 h 30 min after capsule ingestion (81% of the small bowel transit time from the first duodenal image), the capsule showed active ileal oozing and bleeding from an otherwise normal mucosa (Figure 1). With the aim of stopping the bleeding, we performed an R-DBE (instrument: Fuji EN450T5; working length: 2000 mm, and distal end diameter: 9.4 mm) under conscious sedation (pethidine 50 mg, midazolam 5 mg, i.v.) up to 180 cm from the ileocecal valve, which we calculated using the May method[5] without experiencing any technical difficulty. A 5 mm, branched angioectasia (type 1b of the Yano-Yamamoto classification[6]) was identified that was 150 cm proximal to the ileocecal valve (Figure 2A), which we treated by argon plasma coagulation (low power, 10 Watt) and then tattooed (Figure 2B). No other lesion was identified. At the end of the procedure (total procedural time: 74 min), the patient was asymptomatic and his vital parameters were stable. Then, 12 h later, he reported a dull, ill-defined abdominal pain and a physical examination was unremarkable. However, laboratory tests showed a decrease of 2 g/dL in the hemoglobin concentration in the absence of overt hematochezia. An urgent contrast enhanced computerized tomography (CT) scan revealed a grade IV splenic injury with active bleeding (Figure 3), according to the American Association for the Surgery of Trauma classification[7]. Because of the high injury severity score, operative management was performed[8]. Hemoperitoneum and splenic capsular laceration was confirmed during surgery, and splenectomy and segmental ileal resection of the tattooed ileal region was carried out. The choice to make an ileal resection was dictated based on the high re-bleeding rate after endoscopic thermo-ablation of angioectasia[9]. The patient was discharged 14 d later in good health and was administered oral warfarin. Then, two months later, he returned to the hospital because of further gastrointestinal bleeding and anemia. Colonoscopy confirmed red blood in the colonic lumen, without any evidence of active bleeding; an upper endoscopy was normal. He was transfused and treated with somatostatin infusion. After confirming that the bleeding had stopped, he was discharged and prescribed subcutaneous long-acting octreotide (20 mg, monthly). No additional transfusions were required during the six-month follow-up period.
To date, no case of splenic rupture after DE has been reported in the English language literature. The rate of occurrence of splenic injury following colonoscopy is very low, but it may be underestimated because of a reluctance to report unfavorable outcomes[10]. In a population-based study, Cooper et al[11] reported 12 splenic injuries among 165527 procedures. However, the complication rate with any endoscopic procedure is generally low, so a large number of DE need to be performed to determine the complication rate of such a relatively new invasive procedure. It is conceivable that R-DBE, which is a more invasive and less frequently performed procedure than colonoscopy, may carry a higher risk of splenic injury.
In our unit, beginning in 2006, we have performed a mean of 22 DBE/year, mostly by an antegrade approach; however, a single operator (CMG) recently performed 15 consecutive therapeutic R-DBE procedures without any complications. Although a learning curve has not yet been established for R-DBE, Mehdizadeh et al[12] suggest a minimum of 20 procedures to learn to maintain ileal access through the ileocecal valve and reduce procedure times.
Splenic injury complicating gastrointestinal endoscopy may result from either direct trauma or excessive traction on the splenocolic ligament that occurs during the maneuvers required for instrument advancement. Several risk factors have been postulated and categorized as endoscopist-dependent (scope straightening, hooking the splenic flexure, alpha maneuver, and excessive hurry) or patient-dependent (female gender, smoking, anticoagulation, splenomegaly, pre-existing spleen disease, and adhesions)[13-15].
Interestingly, the most predictive diagnostic indicator of splenic injury was found to be an unexplained decrease in hemoglobin greater than 3 g/dL after endoscopy rather than procedural difficulties[3]. Deep sedation may be related to a delayed diagnosis of this complication[11]. Nearly all colonoscopic splenic injuries require surgical intervention, with a mortality rate of 5%[13]. With regard to DBE, two retrospective series of 40 and 41 patients older than 70 and 65 years, respectively, did not show a complication rate that was higher than that seen in younger patients[16,17]. In our present case, chronic oral anticoagulation, several colonoscopies performed before R-DBE, and mild splenomegaly (resulting from subclinical prosthesis-related mechanical hemolysis) likely contributed to the pathogenesis of this complication.
In conclusion, we have reported the first case of splenic rupture after therapeutic R-DBE. Careful clinical observation after such procedures is strongly advisable to promptly recognize and treat this rare but dreadful endoscopic complication.
An 85-year-old man on chronic warfarin underwent successful retrograde double-balloon enteroscopy for bleeding control of an ileal angioectasia, diagnosed on a previous capsule endoscopy. Twelve hours following the procedure, the patient complained abdominal pain.
Acute abdomen following deep enteroscopy (DE).
Intestinal perforation vs splenic injury.
Decrease of 2 g/dL of blood hemoglobin level.
Hemoperitoneum and grade IV splenic injury on contrast enhanced computerized tomography.
Splenic capsular laceration and rupture of the spleen.
Urgent splenectomy and ileal resection.
Splenic rupture is a rare devastating complication of gastrointestinal endoscopy. Immediate or delayed splenic injury and rupture have mostly been reported following diagnostic and therapeutic colonoscopy. This is the first reported case of splenic rupture following retrograde DE.
Vascular lesions of the small bowel are classified by the Yano-Yamamoto classification. Type 1a: Punctulate erythema with or without oozing; type 1b: Patchy erythema with or without oozing; type 2a: Punctulate erythema with pulsatile bleeding; type 2b: Pulsatile red protrusion without surrounding venous dilatation; type 3: Pulsatile red protrusion with surrounding venous dilatation; type 4: Other lesions not classified into any of the above categories.
Retrograde double-balloon enteroscopy can cause delayed splenic rupture. Careful clinical patient observation is recommended after this procedure. Abdominal pain along with hemoglobin decrease ≥ 2 g/dL following the procedure mandate urgent contrast enhanced abdominal computerized tomography.
The authors report a case of spleen injury after DE for the first time and underscore the importance of careful clinical observation for a patient, especially complaining of abdominal pain, after endoscopic examination in order to recognize and treat this potentially life-threatening complication as soon as possible. Thus, this report is very unique and instructive for many kinds of clinicians including endoscopists.
P- Reviewer: Akyuz F, Ogata H, Soria F, Tsujikawa T, Urbain D S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Zyromski NJ, Camp CM. Splenic injury: a rare complication of endoscopic retrograde cholangiopancreatography. Am Surg. 2004;70:737-739. [PubMed] |
| 2. | Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC Emerg Med. 2012;12:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 120] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 3. | Singla S, Keller D, Thirunavukarasu P, Tamandl D, Gupta S, Gaughan J, Dempsey D. Splenic injury during colonoscopy--a complication that warrants urgent attention. J Gastrointest Surg. 2012;16:1225-1234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Pennazio M, Spada C, Eliakim R, Keuchel M, May A, Mulder CJ, Rondonotti E, Adler SN, Albert J, Baltes P. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2015;47:352-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 560] [Article Influence: 56.0] [Reference Citation Analysis (1)] |
| 5. | May A, Nachbar L, Schneider M, Neumann M, Ell C. Push-and-pull enteroscopy using the double-balloon technique: method of assessing depth of insertion and training of the enteroscopy technique using the Erlangen Endo-Trainer. Endoscopy. 2005;37:66-70. [PubMed] |
| 6. | Yano T, Yamamoto H, Sunada K, Miyata T, Iwamoto M, Hayashi Y, Arashiro M, Sugano K. Endoscopic classification of vascular lesions of the small intestine (with videos). Gastrointest Endosc. 2008;67:169-172. [PubMed] |
| 7. | Moore EE, Shackford SR, Pachter HL, McAninch JW, Browner BD, Champion HR, Flint LM, Gennarelli TA, Malangoni MA, Ramenofsky ML. Organ injury scaling: spleen, liver, and kidney. J Trauma. 1989;29:1664-1666. [PubMed] |
| 8. | Siriratsivawong K, Zenati M, Watson GA, Harbrecht BG. Nonoperative management of blunt splenic trauma in the elderly: does age play a role. Am Surg. 2007;73:585-589; discussion 590. [PubMed] |
| 9. | May A, Friesing-Sosnik T, Manner H, Pohl J, Ell C. Long-term outcome after argon plasma coagulation of small-bowel lesions using double-balloon enteroscopy in patients with mid-gastrointestinal bleeding. Endoscopy. 2011;43:759-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 85] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 10. | Lawton R, Parker D. Barriers to incident reporting in a healthcare system. Qual Saf Health Care. 2002;11:15-18. [PubMed] |
| 11. | Cooper GS, Kou TD, Rex DK. Complications following colonoscopy with anesthesia assistance: a population-based analysis. JAMA Intern Med. 2013;173:551-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 190] [Article Influence: 15.8] [Reference Citation Analysis (1)] |
| 12. | Mehdizadeh S, Han NJ, Cheng DW, Chen GC, Lo SK. Success rate of retrograde double-balloon enteroscopy. Gastrointest Endosc. 2007;65:633-639. [PubMed] |
| 13. | Skipworth JR, Raptis DA, Rawal JS, Olde Damink S, Shankar A, Malago M, Imber C. Splenic injury following colonoscopy--an underdiagnosed, but soon to increase, phenomenon. Ann R Coll Surg Engl. 2009;91:W6-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Rao KV, Beri GD, Sterling MJ, Salen G. Splenic injury as a complication of colonoscopy: a case series. Am J Gastroenterol. 2009;104:1604-1605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Sidhu R, Sanders DS. Double-balloon enteroscopy in the elderly with obscure gastrointestinal bleeding: safety and feasibility. Eur J Gastroenterol Hepatol. 2013;25:1230-1234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Choi DH, Jeon SR, Kim JO, Kim HG, Lee TH, Lee WC, Kang BS, Cho JH, Jung Y, Kim WJ. Double-balloon enteroscopy in elderly patients: is it safe and useful. Intest Res. 2014;12:313-319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |