Published online Aug 10, 2016. doi: 10.4253/wjge.v8.i15.541
Peer-review started: February 23, 2016
First decision: March 25, 2016
Revised: April 11, 2016
Accepted: June 1, 2016
Article in press: June 3, 2016
Published online: August 10, 2016
Processing time: 166 Days and 20.8 Hours
To describe the procedure, efficacy, and utility of single-incision laparoscopic-assisted stoma creation (SILStoma) for transverse colostomy. Using single-incision laparoscopic surgery, we developed a standardized technique for SILStoma. Twelve consecutive patients underwent SILStoma for transverse colostomy at Osaka Medical Center for Cancer and Cardiovascular Diseases from April 2013 to March 2016. A single, intended stoma site was created with a 2.5-3.5 cm skin incision for primary access to the intra-abdominal space, and it functioned as the main port through which multi-trocars were placed. Clinical and operative factors and postoperative outcomes were evaluated. Patient demographics, including age, gender, body mass index, and surgical indications for intestinal diversion were evaluated. SILStoma was performed in nine cases without the requirement of additional ports. In the remaining three cases, 1-2 additional 5-mm ports were required for mobilization of the transverse colon and safe dissection of abdominal adhesions. No cases required conversion to open surgery. In all cases, SILStoma was completed at the initial stoma site marked preoperatively. No intraoperative or postoperative complications greater than Grade II (the Clavien-Dindo classification) were reported in the complication survey. Surgical site infection at stoma sites was observed in four cases; however, surgical interventions were not required and all infections were cured completely. In all cases, the resumption of bowel movements was observed between postoperative days 1 and 2. SILStoma for transverse loop colostomy represents a feasible surgical procedure that allows the creation of a stoma at the preoperatively marked site without any additional large skin incisions.
Core tip: We described the procedure, efficacy, and utility of single-incision laparoscopic-assisted stoma creation (SILStoma) for transverse colostomy. Using single-incision laparoscopic surgery, we developed a standardized technique for SILStoma. Twelve consecutive patients underwent SILStoma for transverse colostomy. In all cases, SILStoma was completed at the initial stoma site marked preoperatively. No complications were reported in the complication survey. SILStoma for transverse loop colostomy represents a feasible surgical procedure allowing stoma creation at ideal stoma sites marked preoperatively. Reductions in the number of port sites and the avoidance of additional skin incisions may result in improved cosmetic outcomes and patient quality of life.
- Citation: Miyoshi N, Fujino S, Ohue M, Yasui M, Noura S, Wada Y, Kimura R, Sugimura K, Tomokuni A, Akita H, Kobayashi S, Takahashi H, Omori T, Fujiwara Y, Yano M. Standardized technique for single-incision laparoscopic-assisted stoma creation. World J Gastrointest Endosc 2016; 8(15): 541-545
- URL: https://www.wjgnet.com/1948-5190/full/v8/i15/541.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i15.541
In the last decade, laparoscopy has been effectively utilized for colorectal surgery in many institutions and is associated with decreased blood loss, shorter hospital stays, decreased postoperative pain, faster postoperative recovery, and improved quality of life[1-4]. Conventional multiport laparoscopic colorectal surgery, such as for colorectal cancer, is generally performed using 4-5 trocar: 1 trocar for a laparoscopist, 2 trocars for an operator, and 1-2 trocars for an assistant. To reduce patient stress (i.e., wound pain and cosmetic outcome), efforts have been made to decrease the number of port sites and shorten the length of skin incisions. Therefore, reduced port surgery (RPS), including single-incision laparoscopic surgery, has been developed for colorectal surgery[5-8].
In general, RPS utilizes an umbilical incision as the main port for multi-trocar (generally, 2-4 trocars) access to remove specimens and perform anastomosis at bowel ends during colorectal surgery. The skin incision length of the main port depends on the surgical procedure performed. Although shorter skin incisions and decreased numbers of port sites limit the work space for laparoscopic handling, they have been shown to reduce wound pain and improve cosmetic outcome.
Stoma creation for intestinal diversion is a common surgical procedure. Compared with ileostomy, the stoma site of colostomy is limited by the length and mobilization of the target section of the colon such as transverse colon. Utilizing single-incision laparoscopic surgery, we developed a standardized technique for single-incision laparoscopic-assisted stoma creation (SILStoma). Herein, we describe the procedure, technical details, efficacy, and utility of SILStoma for transverse colostomy.
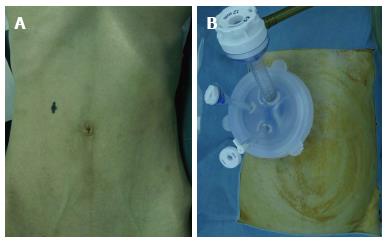
Twelve consecutive patients with bowel obstruction at a left-sided colon or rectum underwent SILStoma for transverse colostomy at Osaka Medical Center for Cancer and Cardiovascular Diseases from April 2013 to March 2016. A surgeon and an experienced enterostomal therapy nurse preoperatively marked an appropriate stoma site. A single, intended stoma site was created with a 2.5-3.5 cm skin incision for primary access to the intra-abdominal space, and it functioned as the main port through which multi-trocars were placed. SILStoma was performed as follows: An initial skin incision was made at the stoma site marked preoperatively and Lap-Protector (Hakko Co. Ltd., Nagano, Japan) and EZ Access (Hakko Co. Ltd., Nagano, Japan) were placed into the incision site. Three devices were introduced through the EZ Access and were adjusted to fit the Lap-Protector, including a flexible laparoscope (Olympus, Tokyo, Japan) and two operating forceps (Figure 1). An operator used two trocars and an assistant handled the laparoscope. In cases where the completion of the surgical procedure using a single port proved technically challenging, an additional port was introduced via the lateral abdomen.
The entire abdominal cavity was inspected laparoscopically. In the head-up tilt position with right side up, the transverse colon was detected and the target section of the intestinal tract was identified. Using forceps laparoscopically, dissection of greater omentum and mobilization were performed to construct a loop colostomy at the initial stoma site, and the mobilized transverse colon was extracted through the Lap-Protector, which was placed at the stoma site (Figure 2). Depending on the size of the transverse colon, the fascia was closed with Vicryl (size 1; Johnson and Johnson, New Brunswick, NJ, United States) to prevent stoma site hernia. The skin and intestine were sutured and fixed with vicryl.
Clinical and operative factors and postoperative outcomes were evaluated. Surgical complications were assessed according to the Clavien-Dindo classification system[9], in which all complications were graded from I to IV. The present study was approved by the institutional review board of Osaka Medical Center for Cancer and Cardiovascular Diseases.
Patient demographics, including age, gender, body mass index, and surgical indications for intestinal diversion are shown in Table 1. Previous history related to surgical interventions, such as previous abdominal surgeries, operation time, intraoperative bleeding, number of additional port sites, conversion to laparotomy, postoperative complications, and median days until stoma functioned were investigated (Table 2).
| Age (yr) | 61.5 (54-76) |
| Sex (male/female) | 5/7 |
| Body mass index | 21.85 (13.7-24.5) |
| Previous surgical history | 1 |
| Indications | |
| Unresectable obstructive descending colon cancer | 1 |
| Unresectable obstructive rectal cancer | 10 |
| Recurrence of uterine corpus cancer with rectal obstruction | 1 |
| Preoperative decompression of intestine | 7 |
| All continuous variables are expressed as medians (range) | |
| Operative duration (min) | 58.5 (28-140) |
| Blood loss (mL) | 0 (0-5) |
| Additional port (except single incision) | 0 (0-2) |
| Conversion to open | 0 |
| Complications (Grade ≥ II1) | 0 |
| Median days until stoma functioning | 1 (1-2) |
| All continuous variables are expressed as average and standard deviation | |
| Operative duration (min) | 76.9 ± 38.3 |
| Blood loss (mL) | 0.4 ± 1.4 |
| Additional port (except single incision) | 0 (0-2) |
| Conversion to open | 0 |
| Complications (Grade ≥ II1) | 0 |
SILStoma was performed in nine cases without the requirement of additional ports. In two cases, one additional port (5 mm at the left-side lateral abdomen) was required, and in another case, two additional ports (5 mm trocars at left- and right-side lateral abdomen) were required. In the remaining three cases, additional ports allowed mobilization of the transverse colon and the safe dissection of abdominal adhesions. No cases required conversion to open surgery. In all cases, SILStoma was completed at the initial stoma sites marked preoperatively with a success rate of 100%.
No intra- or postoperative complications greater than or equal to Grade II were reported in the postoperative complication survey. Surgical site infection at the stoma sites was observed in four cases; however, surgical interventions were not required and all infections were completely cured within 30 d after the operation.
In all cases, the resumption of bowel movements was observed between postoperative days 1 and 2. Postoperative diets were provided after confirmation of the resumption of bowel movements.
Laparoscopic surgery was introduced to improve patient quality of life by reducing wound length and pain, leading to quicker postoperative recovery. Results from several randomized studies have demonstrated the non-inferiority of laparoscopic surgery in terms of short-term oncological outcomes compared with conventional open surgery[1,10,11]. Laparoscopic surgery has been applied in the treatment of colorectal cancer, where radical resection is the overall goal of treatment to reduce disease recurrence and improve patient survival[1,10-12].
The introduction of RPS, including single-incision laparoscopic surgery, has been shown to improve cosmetic outcomes; however, reducing the number of port sites limits laparoscopic handling space. In recent years, a small number of reports have compared the clinicopathological factors and outcomes between single-incision laparoscopic surgery and conventional laparoscopic surgery for colectomy[13-15]. These studies reported no differences in operative duration, conversion rate to open surgery, number of lymph nodes harvested, length of hospital stay, postoperative complications, or mortality[13-15]. Among the 12 cases included in the present study, no intra- or postoperative complications greater than or equal to Grade II were reported. No cases required conversion to open surgery.
In the present study, we performed colostomy at the transverse colon because the obstructive effect such as colitis and edema at the sigmoid colon. The stoma site was a major concern as the surgical procedure was performed via a single port site; however, we were able to mobilize the transverse colon by laparoscopic surgery and create the stoma at the site initially marked preoperatively. Resultant stoma sites were those marked preoperatively in all cases, indicating the substantial benefit of this rational approach to stoma creation. Another concern was the reduction in the number of port sites that may have increased the technical difficulty of operative handling during the surgical procedure. In order to reduce the difficulty caused by the limited work space at the main port for multi-trocar access, we placed three trocars in the EZ Access device and make differences of the trocar length. In the first five cases, the surgical procedure took long time (supplementary table S1); however, the relatively short operation time observed in the succeeding cases indicates that SILStoma is no more time-consuming than comparable techniques, and indirectly demonstrated that technical challenges encountered during the surgical procedure may be less than anticipated. Although we included consecutive cases in the present study, we did not perform a comparison of open vs single-incision laparoscopic surgery using patient randomization. Therefore, selection bias may have been introduced to the results of the present study. There have been several previous studies of single-incision laparoscopic surgery for ileostomy and sigmoid colostomy, however small number of cases was evaluated for transverse colostomy[16-18]. Although further studies are required to fully determine the potential benefit of the presented technique, SILStoma did not impede stoma creation, indicating its utility in transverse loop colostomy.
SILStoma for transverse loop colostomy represents a feasible surgical procedure allowing stoma creation at ideal stoma sites marked preoperatively. Reductions in the number of port sites and the avoidance of additional skin incisions may result in improved cosmetic outcomes and patient quality of life.
The procedure, efficacy, and utility of single-incision laparoscopic-assisted stoma creation (SILStoma) for transverse colostomy.
A single, intended stoma site was created with a 2.5-3.5 cm skin incision for primary access to the intra-abdominal space, and it functioned as the main port through which multi-trocars were placed.
SILStoma was performed as follows: An initial skin incision was made at the stoma site marked preoperatively and Lap-Protector (Hakko Co. Ltd., Nagano, Japan) and EZ Access (Hakko Co. Ltd., Nagano, Japan) were placed into the incision site.
The skin and intestine were sutured and fixed with vicryl.
Laparoscopic surgery was introduced to improve patient quality of life by reducing wound length and pain, leading to quicker postoperative recovery. Results from several randomized studies have demonstrated the non-inferiority of laparoscopic surgery in terms of short-term oncological outcomes compared with conventional open surgery.
SILStoma for transverse loop colostomy represents a feasible surgical procedure allowing stoma creation at ideal stoma sites marked preoperatively. Reductions in the number of port sites and the avoidance of additional skin incisions may result in improved cosmetic outcomes and patient quality of life.
The paper is interesting, and well-presented and developed and consequently.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Garcia-Vallejo L, Hiraki M, Nakayama Y, Neri V S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G. Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA. 2002;287:321-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 540] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 2. | Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2606] [Cited by in RCA: 2518] [Article Influence: 119.9] [Reference Citation Analysis (0)] |
| 3. | Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25:3061-3068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1112] [Article Influence: 61.8] [Reference Citation Analysis (0)] |
| 4. | Yamamoto S, Inomata M, Katayama H, Mizusawa J, Etoh T, Konishi F, Sugihara K, Watanabe M, Moriya Y, Kitano S. Short-term surgical outcomes from a randomized controlled trial to evaluate laparoscopic and open D3 dissection for stage II/III colon cancer: Japan Clinical Oncology Group Study JCOG 0404. Ann Surg. 2014;260:23-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 270] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 5. | Makino T, Milsom JW, Lee SW. Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg. 2012;255:667-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Champagne BJ, Papaconstantinou HT, Parmar SS, Nagle DA, Young-Fadok TM, Lee EC, Delaney CP. Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg. 2012;255:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 147] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 7. | Yang TX, Chua TC. Single-incision laparoscopic colectomy versus conventional multiport laparoscopic colectomy: a meta-analysis of comparative studies. Int J Colorectal Dis. 2013;28:89-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Vestweber B, Galetin T, Lammerting K, Paul C, Giehl J, Straub E, Kaldowski B, Alfes A, Vestweber KH. Single-incision laparoscopic surgery: outcomes from 224 colonic resections performed at a single center using SILS. Surg Endosc. 2013;27:434-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6210] [Cited by in RCA: 8636] [Article Influence: 539.8] [Reference Citation Analysis (0)] |
| 10. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1681] [Article Influence: 84.1] [Reference Citation Analysis (0)] |
| 11. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [PubMed] [DOI] [Full Text] |
| 12. | Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Hellinger M, Flanagan R, Peters W, Nelson H. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655-662; discussion 662-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 802] [Article Influence: 44.6] [Reference Citation Analysis (0)] |
| 13. | Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, Oh ST. The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg. 2011;254:933-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 14. | Fujii S, Watanabe K, Ota M, Watanabe J, Ichikawa Y, Yamagishi S, Tatsumi K, Suwa H, Kunisaki C, Taguri M. Single-incision laparoscopic surgery using colon-lifting technique for colorectal cancer: a matched case-control comparison with standard multiport laparoscopic surgery in terms of short-term results and access instrument cost. Surg Endosc. 2012;26:1403-1411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Huscher CG, Mingoli A, Sgarzini G, Mereu A, Binda B, Brachini G, Trombetta S. Standard laparoscopic versus single-incision laparoscopic colectomy for cancer: early results of a randomized prospective study. Am J Surg. 2012;204:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 16. | Nguyen HM, Causey MW, Steele SR, Maykel JA. Single-port laparoscopic diverting sigmoid colostomy. Dis Colon Rectum. 2011;54:1585-1588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Zaghiyan KN, Murrell Z, Fleshner PR. Scarless single-incision laparoscopic loop ileostomy: a novel technique. Dis Colon Rectum. 2011;54:1542-1546. [PubMed] [DOI] [Full Text] |
| 18. | Hasegawa J, Hirota M, Kim HM, Mikata S, Shimizu J, Soma Y, Nezu R. Single-incision laparoscopic stoma creation: experience with 31 consecutive cases. Asian J Endosc Surg. 2013;6:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |