Published online Jun 25, 2016. doi: 10.4253/wjge.v8.i12.444
Peer-review started: February 14, 2016
First decision: March 23, 20116
Revised: April 20, 2016
Accepted: May 17, 2016
Article in press: May 27, 2016
Published online: June 25, 2016
Processing time: 138 Days and 18 Hours
Nowadays, the trend is to perform surgeries with “scarless” incisions. In light of this, the single-port laparoscopic surgery (SPLS) technique is rapidly becoming widespread due to its lack of invasiveness and its cosmetic advantages, as the only entry point is usually hidden in the umbilicus. The interest in “scarless” liver resections did not grow as rapidly as the interest in other scarless surgeries. Hepatopancreatobiliary surgeons are reluctant to operate a malignant lesion through a narrow incision with limited exposure. There are concerns over adverse oncological outcomes for single-port laparoscopic liver resections (SPL-LR) for hepatocellular carcinoma or metastatic colorectal cancer. In addition, getting familiar with using the operating instruments through a narrow incision with limited exposure is very challenging. In this article, we reviewed the published literature to describe history, indications, contraindications, ideal patients for new beginners, technical difficulty, advantages, disadvantages, oncological concern and the future of SPL-LR.
Core tip: This manuscript highlights the indications, contraindications, technical difficulties, advantages and disadvantages of the single-incisionlaparoscopic (SIL) liver surgery. The authors wanted to share their experience of SIL liver surgery by this review and to create a referrence review for new beginners.
- Citation: Karabicak I, Karabulut K. Single port laparoscopic liver surgery: A minireview. World J Gastrointest Endosc 2016; 8(12): 444-450
- URL: https://www.wjgnet.com/1948-5190/full/v8/i12/444.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i12.444
Laparoscopic liver resection is performed on benign and malignant liver tumors. Preliminary oncological results of liver resection have demonstrated that laparoscopic techniques are as effective as open procedures in a select group of patients[1-4]. Laparoscopic liver surgery has been shown to be superior to open surgery in terms of intraoperative blood loss, pain control, duration of hospital stay, resumption of oral intake, and complication rates[5-8].
Laparoscopic metastasectomy and left lateral sectionectomy are widely performed and accepted as the gold standard treatment for liver tumors in many hepatobiliary centers[9]. Major hepatectomies, such as left and right hepatectomies or extended left and right hepatectomies, are performed laparoscopically by experienced hepatobiliary surgeons[1,3,6,7,10].
Nowadays, the trend is to perform surgeries with “scarless” incisions. In light of this, the single-port laparoscopic surgery (SPLS) technique is rapidly becoming widespread due to its lack of invasiveness and its cosmetic advantages, as the only entry point is usually hidden in the umbilicus[11-13].
As advances in laparoscopic liver resections have been slower than laparoscopic resections of other organs, the interest in “scarless” liver resections did not grow as rapidly as the interest in other scarless surgeries. Moreover, single-port laparoscopic liver resection (SPL-LR) has a significant learning curve, which can make surgeons reluctant to perform it[14-18].
The most difficult part of this technique is getting familiar with using the operating instruments through a narrow incision with limited exposure[12,14,18,19]. Surgeons with experience in both open and laparoscopic liver surgery are best suited to perform this challenging procedure[14-18].
Those who intend to start performing SPL-LR have to be very selective in choosing first patients during the learning curve so as to not fail. A surgeon should combine his/her experience in both laparoscopic liver resection and SPLS for other organs such as gallbladder when performing the SPL-LR, especially during the initial stages of the learning curve[14-19].
SPL-LR is a newly emerging technique, and it is still limited in practice. The development of special instruments to facilitate this technique have made liver resection feasible and safe, but surgeons have been slow in applying this technique[14-16].
The first report of SPL-LR, published by Aldrighetti et al[19] in 2010, was a left lateral sectionectomy for a single colorectal metastasis. After the publication of this, many case reports and a few short series about SPL-LR and two case-matched analysis of traditional laparoscopic liver resection and SPL-LR were published[14-18,20-27]. Table 1 shows baseline characteristics of small case series about SPL-LR. We published the first SPL pericystectomy for liver hydatid disease[26].
| Ref. | Type of article | Year | Country | No. of patients by diagnosis | Type of Surgery | Child-Pugh classification of HCC patients | |||||
| Benign Lesion | HCC | Metastatic tumor | Right hepatectomy | Left hepatectomy | LLLS | Nonanatomic resection or segmentectomy | |||||
| Shetty et al[14] | Case series | 2011 | South Korea | - | 23 | - | 1 | 1 | 4 | 17 | No data |
| Pan et al[18] | Case series | 2012 | China | 3 | 4 | 1 | 3 | 5 | A (4) | ||
| Aikawa et al[21] | Case series | 2012 | Japan | 2 | 5 | 1 | - | - | - | 8 | A (3) B (1) C (1) |
| Hu et al[22] | Prospective, randomized, controlled study | 2014 | China | 18 | - | - | - | - | 14 | - | No data |
| Wu et al[24] | Case series | 2014 | China | 13 | 2 | 2 | - | 1 | 8 | 8 | No data |
| Aldrighetti et al[25] | Case-matched analysis | 2012 | Italy | 5 | 6 | 2 | - | - | 13 | - | No data |
| Karabicak et al[27] | Case series | 2016 | Turkey | 3 | 2 | 4 | - | - | 2 | 7 | A (1) B (1) |
Patient selection is of paramount importance for SPLS. The aim of SPLS is to reduce the operative trauma and to make the smallest possible incision (2.5 to 5 cm) that will allow the extraction of the resected specimen (Figure 1). Tumors that require a big incision to remove the resected specimen are against the SPLS mentality[17,19,20,28]. It is mandatory to select the appropriate patient for this procedure, based on the size, malignancy potential and the location of the tumor[15,29].
SPL-LR has been performed for many different benign and malignant lesions such as liver adenoma, focal nodular hyperplasia, hemangioma, hydatid cyst, giant simple cyst, intrahepatic biliary stones, cystadenoma, metastatic liver lesions and hepatocellular carcinoma (HCC)[14,17,19,20,24,26,27,30].
The ideal lesions for SPL-LR are peripherally located superficial tumors[17,21] . Wu et al[24] recommend SPL-LR for patients with benign liver tumors that are less than 10 cm in diameter and located in segments II and III. Hu et al[22] recommends localized benign left lateral liver disease as a suitable candidate for SPL-LR, because laparoscopic left lateral sectionectomy (LLLS) is technically less demanding. They also mention that the resection specimen of benign liver diseases can be fragmented and retrieved without requiring the addition or extension of a trocar incision (Figure 2).
In our experience with the hydatid cyst, the cyst can at times be large enough to totally replace the left lateral section. In cases where the cyst can be totally removed by left lateral sectionectomy, we prefer to use SPL-LR. Once the SPL left lateral sectionectomy performed, the cyst is placed into the retrieval bag and then, the cyst content can be aspirated through the incision while it is in the bag; this enables the collapsed cyst wall to be easily pulled out from the small incision without having to enlarge it.
Malignant tumors bigger than 5 cm are not suitable for SPLS, as the incision required to extract the specimen itself would defeat the purpose of such a procedure[14-18]. Ideally, malignant liver lesions that are suitable for SPL-LR are less than 5 cm in diameter and located in the left lateral sector; alternatively, they are smaller than 2.5 cm in diameter and located at the surface in segments IV, V or VI[24].
Beginner surgeons have to be very cautious while choosing the ideal patients for SPLS. Surgical candidates have to be carefully selected to optimize the benefits of this technique[14-18,24]. One should never forget that, during the learning curve, it is difficult to obtain the angles necessary for parenchymal transection with instruments parallel to each other[12,14,31]. That is why obese patients, patients who require big lesions or lesions located deep in the parenchyma, or cirrhotic patients are not good candidates to start with[14,24,31].
Gkegkes et al[32] advise to start SPL-LR with the peripherally located lesions. The surgeon can then move on to anatomical resections and, finally, proceed to major hepatectomies before he/she can gain sufficient experience with SPL-LR. Wu et al[24] recommend starting with the lesion in the left lateral section or anterior and inferior liver segments (IV anterior, V and VI), since minimal mobilization of the liver is necessary in these locations.
Geller et al[31] recommend the ideal patient to be a thin, young female with a 3-4 cm hepatic adenoma, where cosmesis is of prime concern. Aikawa et al[21] and Aldrighetti et al[25] recommend that new surgeons start with the liver tumors located in the left lateral section, away from the hilum or anterior right hepatic segment.
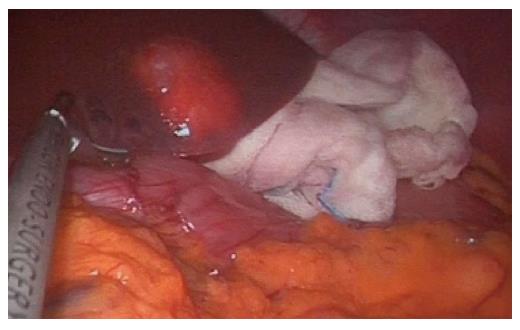
We recommend that during the learning curve, beginners of this technique start with the peripherally located benign lesions to decrease the failure rate (Figure 3). The first few patients should not be cirrhotic patients, as the new surgeon can cause harm and jeopardize the patient’s oncological safety.
We preferred to start performing SPL-LR on patients with peripherally located liver hydatid cysts since it is one of the most common benign liver tumors. Laparoscopic pericystectomy is the ideal surgical treatment for such a location[26].
Laparoscopic liver surgery has already been shown to decrease intraoperative bleeding and postoperative general complications, such as ascites and wound infection, without worsening the oncological outcome in well-selected cirrhotic patients[33-35].
The decrease in abdominal wall trauma in SPLS could be especially useful for cirrhotic patients. SPL-LR has been performed in well-selected cirrhotic patients with a medically and oncologically good outcome[14,21,23]. A peripherally located small HCC is appropriate for SPL-LR, since the surgery can be performed without prolonging the operation time or increasing bleeding so as to avoid deterioration after the surgery[14,16,23].
One has to be cautious with trans-umbilical incisions for the single port, as it can cause severe bleeding due to large umbilical veins. Gaujoux et al[17] recommends making incisions through the rectus abdominis muscle or in the supraumbilical position to avoid bleeding from large umbilical veins.
The first single-port device created for SPLS is the SILS port system (Covidien, Mansfield, MA), which has three access channel, and which is suitable for a 2.5 cm incision. Nowadays, there are many different types of port devices suitable for 2.5 to 5 cm incisions with three or four access channel, each having advantages over the others[18,21,32]. The ideal port has to have flexible access parts to reduce the overlapping of the instruments[14,32]. The size of the port has to be chosen according to the size of the liver to be resected. The port size should not be smaller than the malignant tumor since, eventually, the incision will need to be enlarged[20,21].
SPLS has some technical problems that are peculiar to operating through a single-port[12,14,32]. The main problems of this technique are instrument crowding, the absence of triangulation, the parallel field of view, and a two/three instrument restriction depending on the port choice[12-14,19,22,24,27,31,35].
Having all the instruments and the camera inserted parallel to each other within the single port causes restricted range of movement and conflict between the surgeon and the camera holder, both intracorporeally and extracorporeally[12,16,26,32,36] (Figure 4). The absence of triangulation makes laparoscopic manipulation more complicated and troublesome[22,25,31]. The “sword-fighting” is unavoidable, but this adversity can be decreased by cross-handling the instruments, using single ports with a large outer cap or self-retaining sleeves, and using curved and articulating instruments and flexible scopes[12,16,17,22,37,38].
Another apparent difficulty with SPL-LR is bleeding, which is the most common reason for conversion to traditional laparoscopy or open surgery[32,36]. Experience and careful patient selection are the mainstays of preventing this complication[14,22,25]. Prevention of major bleeding during parenchymal resection is an important step in SPL-LR, since the instruments are limited and the room is too narrow for manipulations[13,22,31,38]. Weiss et al[39] showed reduced bleeding during single-incision laparoscopic minor liver resection with inline radiofrequency pre-coagulation (Habib 4X).
If acute massive bleeding occurs, it is very difficult to stop parenchymal bleeding by SPLS. Shetty et al[14] reported that suture ligation is too time-consuming to control bleeding during SPL-LR due to inadequate instrument angles and extremely uncomfortable needle-handling. Unless the bleeding cannot be treated, conversion to laparoscopy or laparotomy is required[13,22,24,38].
Selection of the umbilicus for the single-port placement allows hiding the incision while achieving the resection. The transumbilical route is not appropriate for all patients, since the distances between the umbilicus and the liver vary from case to case. The entry of the port should be selected based on the patient’s body type and the location of the lesion[14,18,22] (Figure 5).
The development of new single ports, articulating special instruments and laparoscopic surgery experience facilitate this technique. In experienced hands, the SPL anatomical liver resection has become feasible and safe in carefully selected patients[14-17,22,25].
Lesions limited to the left lateral sector of the liver are the most appropriate for this technique. SPL left lateral sectionectomy has been the main type of resection for such lesions[22,25,37]. In this situation, the instruments are already aligned to the intended liver parenchyma transection plane, which helps to avoid “dueling swords” between the surgeon and the camera holder. Also, suspensory ligaments aid in surgical site exposure[17,22,25,40].
SPLS has been performed for different types of resections such as living donor liver harvesting, right hepatectomy, extended left lobectomy, left hepatectomy, left lateral sectionectomy, proximal left hemihepatectomy-segmentectomy, pericystectomy, wedge resection, liver cyst deroofing, biliary exploration, and pericystectomy for hydatid cyst[14,17,18,24,26,41-43].
There are concerns over adverse oncological outcomes for SPL-LR for HCC or metastatic colorectal cancer. Few publications about SPL-LR for malignant lesions are available; a majority of them are case reports, and a few of them are short case series. The role of SPL-LR for malignancy is reported for small HCCs and solitary liver metastasis[15,17,21]. Shetty et al[14] showed that, in the hands of experienced hepatobiliary and laparoscopic surgeons, SPL-LR is oncologically as safe as conventional laparoscopy in a variety of well-selected cases.
Strict oncological principles should not be compromised simply to achieve a SPL-LR. Free resection margins have to be achieved with the “no touch” technique[9,16,28,44]. Shetty et al[14] recommend making 5 cm incisions for SPL-LR in patients with malignant lesions, as this would make surgical handling relatively easy. By making a 5-cm incision, the necessity of the unfamiliar articulating instruments for the resection of the malignant tumor decreases. A 5-cm incision is usually large enough to deliver the specimen while maintaining its contours[14].
The advantages of SPL-LR usually include a hidden incision, minimization of abdominal trauma, less postoperative pain, quicker recovery, earlier resumption of normal activities, and shorter hospital stays compared to conventional surgeries[14-16,24,30]. Small case-control series comparing the SPL limited liver resection and the LLLS showed similarities in operating times, blood loss, length of stay and intra- and post-operative complications[25,30].
SPL-LR may be especially appealing in cirrhotic patients with HCC as it reduces the risk of complications such as ascites and wound infections, which can deteriorate the patient’s condition after a conventional liver resection[14,23].
Tayar et al[15] mentioned that after laparoscopic wedge resections of a liver tumor, one of the trocar incisions is usually enlarged for the specimen removal. They emphasize that this is an advantage of SPLS since, at the end of the surgery, the single-port incision will be used to extract the specimen. Therefore, the surgery can be completed without the need for an additional three or four ports.
An alternative to SPL liver surgery is multiport laparoscopic liver resection. Whenever necessary, one can easily convert single-port to standard laparoscopy if one encounters difficulty during the liver parenchyma resection[17,22,31].
SPL liver surgery has some very well-known disadvantages when compared with conventional laparoscopic surgery. The articulating specific surgical instruments may be necessary during deep parenchymal resection, which may not be easily available in all institutions, thus increasing the cost of the operation[15,21,22,32].
Colorectal cancer solitary small liver metastasis is an indication for SPL-LR. Performing this technique in a patient with a history of previous surgery may not always be possible because of the severe intra-abdominal adhesions (Figure 6). The presence of severe adhesions can diminish the number of patients suitable for this technique, even if the tumor is small and peripherally located. For such patients, conventional laparoscopy is the preferred technique. After making the umbilical incision for the single port, we usually make blunt and sharp dissections under direct visualization to create enough space for the port and the instruments.
SPL liver surgery has a significant learning curve that initially increases the operation time, the conversion rate and complications[14-18,21,22,25,31]. Aikawa et al[21] shortened the SPL-LR time by using multi-functional devices such as division, hemostasis, irrigation and suction.
The location and size of the malignant lesion is crucial. Malignant lesions bigger than 5 cm are considered to be a contraindication for this technique[14,18,24,45]. Anatomic resection of tumors located deep in the liver or in the posterior right lobe are not suitable for this technique, either[18,24,35].
Moreover, patient-related restrictions can diminish the application of SPL-LR. Longer single-port instruments may be necessary in obese or tall patients. Extremely obese patients may not be suitable for SPLS, because the depth of the subcutaneous fatty tissue may not allow the placement of the single port. Single-port site hernia has been reported to be higher in obese patients[15].
More blood loss can occur in cirrhotic patients during SPL-LR than during laparoscopic liver resections or major hepatic resections, especially during the learning curve[14,18,31]. In our experience, articulating tissue sealer shortens the operation time, decreases blood loss and reduces the size of unnecessarily removed liver tissue, particularly in cirrhotic patients.
SPL-LR is a new and emerging technique. Initially, surgeons were reluctant to perform this technique due to concerns about the oncological safety in malignant liver lesions[16,22,24,36]. However, the development of special instruments and ports have facilitated this technique and made it a feasible, effective and safe alternative to conventional laparoscopy for the treatment of peripherally located benign or malignant liver lesions in cautiously selected patients[14-18,22,24-26,45].
SPL-LR should be performed by surgeons with expertise in both liver and advanced laparoscopic surgery in centers where laparoscopic liver resection is routinely performed[14,22-26].
There are a limited number of studies comparing single-port and conventional laparoscopic liver resections, each with a very small sample size owing to strict patient-selection criteria due to safety concerns. Additional indications and contraindications of single-incision laparoscopic liver resections need to be stated in the light of large randomized studies[22,25,32]. Larger, particularly randomised studies are especially necessary to determine whether SPL-LR is safe and feasible for massive hepatic resections and resections of bigger malignant tumors[14-18,25,45].
Studies comparing the oncological outcome and complication rates between SPL-LR and conventional laparoscopy, and between SPL-LR and conventional liver surgery, will determine the future of this emerging technique.
P- Reviewer: Biebl MO, Sinha R S- Editor: Kong JX L- Editor: A E- Editor: Jiao XK
| 1. | Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009;250:831-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 836] [Cited by in RCA: 878] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 2. | Castaing D, Vibert E, Ricca L, Azoulay D, Adam R, Gayet B. Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg. 2009;250:849-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 203] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 3. | Tzanis D, Shivathirthan N, Laurent A, Abu Hilal M, Soubrane O, Kazaryan AM, Ettore GM, Van Dam RM, Lainas P, Tranchart H. European experience of laparoscopic major hepatectomy. J Hepatobiliary Pancreat Sci. 2013;20:120-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 4. | Cugat E, Pérez-Romero N, Rotellar F, Suárez MA, Gastaca M, Artigas V, Olsina JJ, Noguera J, Martínez S, Moreno-Sanz C. Laparoscopic liver surgery: 8 years of multicenter Spanish register. J Hepatobiliary Pancreat Sci. 2010;17:262-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Azagra JS, Goergen M, Gilbart E, Jacobs D. Laparoscopic anatomical (hepatic) left lateral segmentectomy-technical aspects. Surg Endosc. 1996;10:758-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 215] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 6. | Lai EC, Tang CN, Ha JP, Li MK. Laparoscopic liver resection for hepatocellular carcinoma: ten-year experience in a single center. Arch Surg. 2009;144:143-147; discussion 148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Dagher I, Belli G, Fantini C, Laurent A, Tayar C, Lainas P, Tranchart H, Franco D, Cherqui D. Laparoscopic hepatectomy for hepatocellular carcinoma: a European experience. J Am Coll Surg. 2010;211:16-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 122] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 8. | Pearce NW, Di Fabio F, Teng MJ, Syed S, Primrose JN, Abu Hilal M. Laparoscopic right hepatectomy: a challenging, but feasible, safe and efficient procedure. Am J Surg. 2011;202:e52-e58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Azagra JS, Goergen M, Brondello S, Calmes MO, Philippe P, Schmitz B. Laparoscopic liver sectionectomy 2 and 3 (LLS 2 and 3): towards the “gold standard”. J Hepatobiliary Pancreat Surg. 2009;16:422-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | O’Rourke N, Fielding G. Laparoscopic right hepatectomy: surgical technique. J Gastrointest Surg. 2004;8:213-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 177] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 11. | Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy : scarless cholecystectomy. Surg Endosc. 2009;23:1393-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 166] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 12. | Rao PP, Rao PP, Bhagwat S. Single-incision laparoscopic surgery - current status and controversies. J Minim Access Surg. 2011;7:6-16. [PubMed] |
| 13. | Karabicak I, Karabulut K. Is single-port laparoscopy feasible after liver transplant? Pediatr Transplant. 2016;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Shetty GS, You YK, Choi HJ, Na GH, Hong TH, Kim DG. Extending the limitations of liver surgery: outcomes of initial human experience in a high-volume center performing single-port laparoscopic liver resection for hepatocellular carcinoma. Surg Endosc. 2012;26:1602-1608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Tayar C, Subar D, Salloum C, Malek A, Laurent A, Azoulay D. Single incision laparoscopic hepatectomy: Advances in laparoscopic liver surgery. J Minim Access Surg. 2014;10:14-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Chang SK, Mayasari M, Ganpathi IS, Wen VL, Madhavan K. Single port laparoscopic liver resection for hepatocellular carcinoma: a preliminary report. Int J Hepatol. 2011;2011:579203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Gaujoux S, Kingham TP, Jarnagin WR, D’Angelica MI, Allen PJ, Fong Y. Single-incision laparoscopic liver resection. Surg Endosc. 2011;25:1489-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Pan M, Jiang Z, Cheng Y, Xu X, Zhang Z, Zhou C, He G, Xu T, Liu H, Gao Y. Single-incision laparoscopic hepatectomy for benign and malignant hepatopathy: initial experience in 8 Chinese patients. Surg Innov. 2012;19:446-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Aldrighetti L, Guzzetti E, Ferla G. Laparoscopic hepatic left lateral sectionectomy using the LaparoEndoscopic Single Site approach: evolution of minimally invasive liver surgery. J Hepatobiliary Pancreat Sci. 2011;18:103-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Kobayashi S, Nagano H, Marubashi S, Wada H, Eguchi H, Takeda Y, Tanemura M, Sekimoto M, Doki Y, Mori M. A single-incision laparoscopic hepatectomy for hepatocellular carcinoma: initial experience in a Japanese patient. Minim Invasive Ther Allied Technol. 2010;19:367-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Aikawa M, Miyazawa M, Okamoto K, Toshimitsu Y, Okada K, Ueno Y, Yamaguchi S, Koyama I. Single-port laparoscopic hepatectomy: technique, safety, and feasibility in a clinical case series. Surg Endosc. 2012;26:1696-1701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Hu M, Zhao G, Wang F, Xu D, Liu R. Single-port and multi-port laparoscopic left lateral liver sectionectomy for treating benign liver diseases: a prospective, randomized, controlled study. World J Surg. 2014;38:2668-2673. [PubMed] |
| 23. | Belli G, Fantini C, D’Agostino A, Cioffi L, Russo G, Belli A, Limongelli P. Laparoendoscopic single site liver resection for recurrent hepatocellular carcinoma in cirrhosis: first technical note. Surg Laparosc Endosc Percutan Tech. 2011;21:e166-e168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Wu S, Yu XP, Tian Y, Siwo EA, Li Y, Yu H, Yao D, Lv C. Transumbilical single-incision laparoscopic resection of focal hepatic lesions. JSLS. 2014;18:pii: e2014.00397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Aldrighetti L, Ratti F, Catena M, Pulitanò C, Ferla F, Cipriani F, Ferla G. Laparoendoscopic single site (LESS) surgery for left-lateral hepatic sectionectomy as an alternative to traditional laparoscopy: case-matched analysis from a single center. Surg Endosc. 2012;26:2016-2022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Karabicak I, Yuruker S, Seren DT, Kesicioglu T, Cinar H, Ozen N. Single incision laparoscopic surgery for hepatic hydatid disease. Report of a case. Ann Ital Chir. 2013;84:451-453. [PubMed] |
| 27. | Karabicak I, Karabulut K, Yuruker S, Kesicioglu T, Ozen N. Single-Port laparoscopic liver resection: Largest Turkish Experience. Indian J Surg; Published online: January 11. 2016;1-5. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Patel AG, Belgaumkar AP, James J, Singh UP, Carswell KA, Murgatroyd B. Video. Single-incision laparoscopic left lateral segmentectomy of colorectal liver metastasis. Surg Endosc. 2011;25:649-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Wang E, Kow AW, Chan CY, Liau KH, Ho CK. Starting a laparoscopic hepatectomy programme. Singapore Med J. 2009;50:354-359. [PubMed] |
| 30. | Sasaki K, Watanabe G, Matsuda M, Hashimoto M, Harano T. Original method of transumbilical single-incision laparoscopic deroofing for liver cyst. J Hepatobiliary Pancreat Sci. 2010;17:733-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Geller DA. Laparoscopic or SILS liver resection for hepatic left lateral sectionectomy? World J Surg. 2014;38:2674-2675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Gkegkes ID, Iavazzo C. Single incision laparoscopic hepatectomy: A systematic review. J Minim Access Surg. 2014;10:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Dagher I, Lainas P, Carloni A, Caillard C, Champault A, Smadja C, Franco D. Laparoscopic liver resection for hepatocellular carcinoma. Surg Endosc. 2008;22:372-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 34. | Belli G, Fantini C, D’Agostino A, Cioffi L, Langella S, Russolillo N, Belli A. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc. 2007;21:2004-2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 186] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 35. | Cherqui D, Laurent A, Tayar C, Chang S, Van Nhieu JT, Loriau J, Karoui M, Duvoux C, Dhumeaux D, Fagniez PL. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg. 2006;243:499-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 233] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 36. | Montero PN, Acker CE, Heniford BT, Stefanidis D. Single incision laparoscopic surgery (SILS) is associated with poorer performance and increased surgeon workload compared with standard laparoscopy. Am Surg. 2011;77:73-77. [PubMed] |
| 37. | Machado MA, Surjan RC, Makdissi FF. Intrahepatic glissonian approach for single-port laparoscopic liver resection. J Laparoendosc Adv Surg Tech A. 2014;24:534-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Toyama Y, Yoshida S, Okui N, Kitamura H, Yanagisawa S, Yanaga K. Transumbilical single-incision laparoscopic hepatectomy using precoagulation and clipless technique in a patient with combined hepatocellular-cholangiocarcinoma: a case report. Surg Laparosc Endosc Percutan Tech. 2013;23:e194-e199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 39. | Weiss M, Mittermair C, Brunner E, Schirnhofer J, Obrist C, Pimpl K, Hell T, Weiss H. Inline radiofrequency pre-coagulation simplifies single-incision laparoscopic minor liver resection. J Hepatobiliary Pancreat Sci. 2015;22:831-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 40. | Aldrighetti L, Pulitanò C, Arru M, Catena M, Guzzetti E, Casati M, Ferla G. Ultrasonic-mediated laparoscopic liver transection. Am J Surg. 2008;195:270-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 41. | Imamura H, Kawashita Y, Koga N, Sanada Y, Azuma T, Matsuo S, Eguchi S. A large hepatic cyst with obstructive jaundice successfully treated with single-incision laparoscopic deroofing. Case Rep Gastroenterol. 2013;7:503-510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 42. | Yeo D, Mackay S, Martin D. Single-incision laparoscopic cholecystectomy with routine intraoperative cholangiography and common bile duct exploration via the umbilical port. Surg Endosc. 2012;26:1122-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 43. | Choi HJ, You YK, Na GH, Hong TH, Shetty GS, Kim DG. Single-port laparoscopy-assisted donor right hepatectomy in living donor liver transplantation: sensible approach or unnecessary hindrance? Transplant Proc. 2012;44:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 44. | Gigot JF, Glineur D, Santiago Azagra J, Goergen M, Ceuterick M, Morino M, Etienne J, Marescaux J, Mutter D, van Krunckelsven L. Laparoscopic liver resection for malignant liver tumors: preliminary results of a multicenter European study. Ann Surg. 2002;236:90-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 287] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 45. | Tan EK, Lee VT, Chang SK, Ganpathi IS, Madhavan K, Lomanto D. Laparoendoscopic single-site minor hepatectomy for liver tumors. Surg Endosc. 2012;26:2086-2091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |