Published online Jul 10, 2015. doi: 10.4253/wjge.v7.i8.799
Peer-review started: August 28, 2014
First decision: October 14, 2014
Revised: April 13, 2015
Accepted: May 26, 2015
Article in press: May 28, 2015
Published online: July 10, 2015
Processing time: 320 Days and 8 Hours
In recent years, the description of isolated bile duct dilatation has been increasingly observed in subjects with normal liver function tests and nonspecific abdominal symptoms, probably due to the widespread use of high-resolution imaging techniques. However, there is scant literature about the evolution of this condition and the impact of endoscopic ultrasound (EUS) in the diagnostic work up. When noninvasive imaging tests (transabdominal ultrasound, computed tomography or magnetic resonance cholangiopancreatography) fail to identify the cause of dilatation and clinical or biochemical alarm signs are absent, the probability of having biliary disease is considered low. In this setting, using EUS, the presence of pathologic findings (choledocholithiasis, strictures, chronic pancreatitis, ampullary or pancreatic tumors, cholangiocarcinoma), not always with a benign course, has been observed. The aim of this review has been to evaluate the prevalence of disease among non-jaundiced patients without signs of cytolysis and/or cholestasis and the assessment of EUS yield. Data point out to a promising role of EUS in the identification of a potential biliary pathology. EUS is a low invasive technique, with high accuracy, that could play a double cost-effective role: identifying pathologic conditions with dismal prognosis, in asymptomatic patients with negative prior imaging tests, and excluding pathologic conditions and further follow-up in healthy subjects.
Core tip: Common bile duct dilatation, often without identified causes, in subjects with normal liver function tests and nonspecific abdominal symptoms, and absence of lesions on prior noninvasive imaging tests, is increasingly found in the clinical practice. Since the clinical suspicion for biliary pathology in that setting is usually low, and there are limited literature data, this condition is ignored. However, recent evidences show the existence of pathologies among these patients, often with a non-benign course. In this scenario, endoscopic ultrasound may have a role in the identification of the etiology of dilatation.
- Citation: Angelis CD, Marietti M, Bruno M, Pellicano R, Rizzetto M. Endoscopic ultrasound in common bile duct dilatation with normal liver enzymes. World J Gastrointest Endosc 2015; 7(8): 799-805
- URL: https://www.wjgnet.com/1948-5190/full/v7/i8/799.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i8.799
The biliary system plays a central role in digestive pathophysiology, since it allows bile sterile flow from hepatocytes, through intra- and extra-hepatic ducts, Oddi’s sphincter and Vater’s ampulla, to the duodenum determining lipids absorption and excretion of metabolites and toxins in the small bowel[1]. In case of obstruction of these structures (as observed in choledocholithiasis, Mirizzi’s syndrome, neoplastic or flogistic papillary strictures, parasitic infection, cholangiocellular or pancreatic adenocarcinoma), liver biochemical abnormalities and jaundice, sometimes in association with fever or abdominal pain, usually appear[1].
In recent years, due to the widespread use of high-resolution imaging techniques in order to investigate the causes of nonspecific abdominal symptoms, isolated bile duct dilatation in non-jaundiced patients with normal liver function tests has been increasingly reported. There is scant literature about the diagnostic impact of endoscopic ultrasound (EUS) in this setting and not much is known about the natural evolution of this condition. The aim of this review has been to analyze EUS accuracy in this scenario.
There are controversies regarding the upper normal diameter of the common bile duct (CBD) but it is conventionally accepted to be 7 mm[2-6]. A variety of factors can influence bile duct size, prominently imaging modality, age[7-10] and prior cholecystectomy. In transabdominal ultrasound (TUS), distal CBD may be difficult to visualize because of bowel gas, thus resulting in underestimation of duct size compared to other imaging techniques as computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP), endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangiography (PTC)[11]. On CT and MRCP imaging, bile duct wall is included in the measurement and, because of its oblique course and the difficulty to separate a possible low cystic duct insertion, result on the axial source may be inaccurate[8]. Finally, magnification and duct distension by contrast, used in ERCP and transhepatic cholangiography, may overestimate duct size[8].
Several studies in the last 20 years reported an increase in the CBD diameter in older patients, even if with consistent variability[6,7,9,10,12]. Based on autoptic observations, some authors identified loss of elastic fibers and proximal compensatory dilatation due to distal sclerosis as potential causes of the phenomenon[13]. Moreover, the fragmentation of the longitudinal smooth myocyte bands in elderly subjects and use of drugs such as calcium antagonists and nitroglycerine, may reduce contractility and cause hypotonus of the duct[12,14]. Finally, prior cholecystectomy seems to influence CBD diameter since gallbladder physiologically plays a role in accommodation of pressure fluctuation in biliary system which, after surgery, could be transferred to bile duct causing dilatation[11,15-17].
Among non-obstructive etiologies of CBD dilatation, opioids consumption has been described. Opiates may cause an increase in the basic pressure and in frequency of phasic contractions of the Oddi’s sphincter leading to biliary dilatation[18,19]. In a study performed by Farahmand et al[20], the authors showed an association between increased biliary diameter, evaluated on TUS, and addiction to opioids in asymptomatic patients, with normal levels of serum bilirubin and alkaline phosphatase tests and absence of obstructive factors on TUS. In a recent study, opium addicts, symptomatic for abdominal pain were subjected to EUS. The authors observed CBD dilatation, especially in the extra hepatic tract, in all 15 patients included and increased surface area of Vater’s papilla in 12 of them, after a mean of 20 years of opium addiction[21].
Pathologic conditions are also able to induce isolated bile duct dilatations with non-specific symptoms or biochemical abnormalities. Choledocholithiasis, which develops in about 10%-20% of patients with gallbladder stones, may be asymptomatic in half of cases and CBD stones cannot always be identified by traditional non invasive imaging techniques[22]. Reported sensitivity in detection of CBD stones is 18%-74% for TUS and 50%-90% for CT[23-25]. Recently developed imaging modalities, such as MRCP and helical computed tomographic cholangiography (HCT-C) have shown higher sensitivity than TUS and conventional CT, and remain less invasive than ERCP[26]. However, EUS is considered more accurate in detecting CBD stones, especially if smaller than 5 mm in diameter, which are sometimes not identified by MRCP and HCT-C[26]. When choledocholithiasis is suspected, sensitivity of EUS reaches 90% for the detection of CBD stones[27-29]. In a prospective study, performed by Fernández-Esparrach et al[30] on patients with dilatated biliary tree, EUS increased the pretest probability of accurately diagnosing choledocholithiasis as the cause of obstruction from 49% to 84%. On the contrary, this probability decreased from 49% to 0% if EUS ruled out lithiasis as the cause of obstruction[30].
In a meta-analysis published in 2008, on EUS performance in detecting choledocholithiasis, the authors proposed EUS as a less low invasive technique to be incorporated into the diagnostic algorithm of patients with suspected CBD stones, in order to confirm the pathological condition before proceeding with therapeutic ERCP, when indicated[31]. Scheiman et al[32], in a prospective study and cost analysis performed on a cohort of patients referred to ERCP, defined EUS the preferred initial diagnostic test, compared with MRCP, for the evaluation of biliary system and identification of extrahepatic disease.
After excluding tumors, stones, flogistic strictures, a rare cause of CBD dilatation may be identified in choledochal cysts, a heterogeneous group of congenital focal or multiple anomalous dilatations of the biliary tree, usually diagnosed in childhood but remaining undetected until adulthood in 25% of cases[33,34]. Although abdominal pain is the most frequent symptom in adult patients, non-specific symptoms are also reported and the cyst may be incidentally identified in patients undergoing radiologic evaluation for other clinical suspicions[35,36].
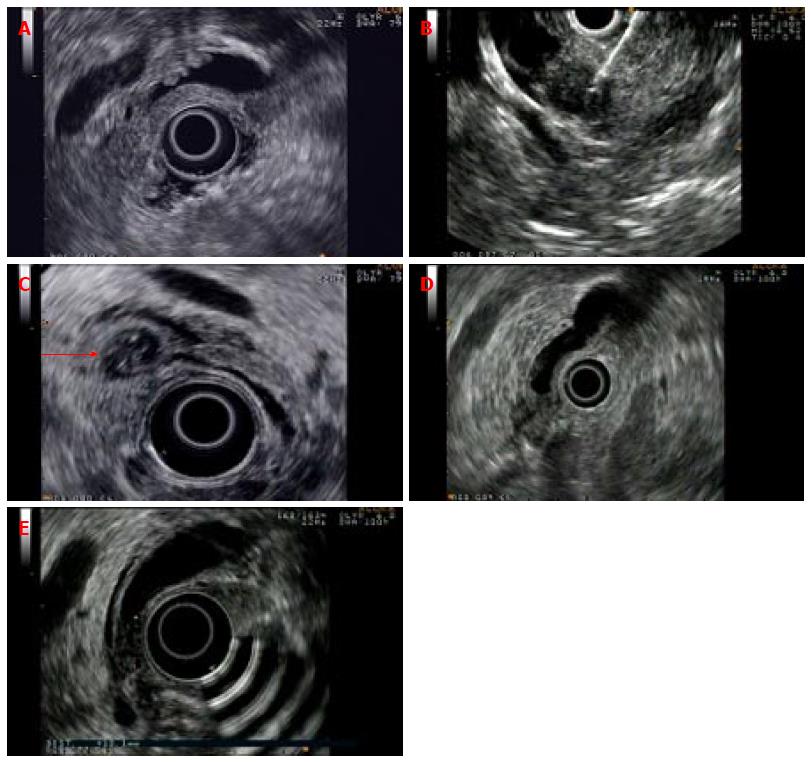
In the presence of CBD dilatation without symptoms or clinical and laboratory alarm signs, when non-invasive imaging test (TUS, CT or MRCP) fail to indentify the etiology, clinical suspicion for biliary pathology is low, thus making further investigations unwarranted[2,8]. In this setting, despite negative results of previous imaging tests, diagnostic EUS could have a role in the identification of the etiology of dilatation (Figure 1) with a very low complication rate[37]. EUS combines endoscopy with real-time and high-resolution ultrasound providing excellent sonographic visualization of the extrahepatic biliary tree without interference of bowel gas, due to its ability to place the transducer in close proximity to the extrahepatic bile duct. Additionally, EUS permits the accurate and systematic visualization of the wall of the duodenum, including the papillary region[38].
Several authors compared MRCP and EUS in detecting choledocholithiasis showing cost-effectiveness and higher accuracy of EUS in detecting distal small stones in non-dilated ducts[26,32,39]. De Lédinghen et al[39] reported a 100% negative predictive value of EUS in the diagnosis of lithiasis, thus excluding the needing for further investigation and limiting unnecessary surgery. In the previously mentioned study by Scheiman et al[32], EUS was the most useful test for confirming a normal biliary tree, and the initial EUS strategy had the greatest cost-utility by avoiding unnecessary ERCPs and preventing ERCP-related complications[40].
In 2001, a prospective study performed by Kim et al[41] showed the existence of pathological conditions in subjects with dilatated CBD, despite the lack of symptoms, jaundice or causative lesions in TUS. Among the 49 patients who underwent ERCP, a significant prevalence of abnormal findings likely causative of dilatation (periampullary duodenal diverticula, benign strictures, choledochal cysts, anomalous pancreaticobiliary ductal anatomy and distal CBD masses), associated with both normal or altered liver chemistry tests, was found.
In 2007, Malik et al[3] retrospectively evaluated a cohort of patients with CBD dilatation and non-diagnostic imaging (TUS, CT or MRCP), previously performed for abdominal pain, weight loss or elevated liver enzymes in serum. These patients underwent EUS, being divided into two groups based on the level of clinical suspicion for biliary pathology (32 patients with normal liver chemistry tests and 15 patients with elevated enzymes)[3]. In the first group, the authors identified two findings on EUS (6%) potentially causative of biliary dilatation, a 7-mm stone of the CBD and a periampullary diverticulum. In the second group, 8 significant findings (53%) were observed: 4 periampullary diverticula, 3 choledocholithiasis and 1 ampullary tumor, not previously detected by TUS and CT.
As expected, the prevalence of biliary pathology is significantly higher in the case of elevated liver chemistry tests; however, despite the lack of pathological findings with non-invasive imaging techniques and normal liver biochemistry, biliary abnormalities may still be present and EUS is recommended for further evaluation.
A study by Carriere et al[42] showed a EUS yield of 28.7% in a cohort of 94 patients with unexplained isolated CBD dilatation, although an undetermined number of subjects of the group underwent endoscopy because of abdominal pain and/or abnormal liver function tests, thus suggesting a higher pre-test probability of pathological findings.
In an abstract published in 2009, based on a retrospective study, 30 patients with biliary dilatation and no evident causes on prior imaging underwent EUS[43]. Four patients had normal biliary system on EUS, 15 patients presented a dilatation of unknown etiology while pathology accounting for CBD dilatation was demonstrated in 11 of them (choledocholithiasis, ampullary adenoma, chronic pancreatitis or cholangiocarcinoma). Similarly to other studies, prevalence of abnormal findings during EUS examination was different between the patients with abnormal and those with normal liver chemistry tests (55% and 33% respectively). Conversely, the number of pathological findings in the latter group differed from percentages reported by other authors[2,3], probably because no details were specified in this study, about clinical presentation and previously used imaging techniques. Notably, none of the patients with unexplained CBD dilatation on EUS was found to have causative lesions after a mean follow-up of 16 mo.
Similarly, Bruno et al[2] studied 57 patients with normal liver enzymes (aminotransferases, gamma glutamyltranspeptidase and bilirubin) referred to EUS at our centre after prior negative imaging studies, excluding previous ERCP or history of biliary obstruction, pancreatitis or jaundice. Reasons for initial investigations were unspecific abdominal pain, dyspepsia, weight loss or pancreatic enzymes elevation in 49.2% of patients but in the majority of them biliary dilatation was an incidental finding. Employed imaging techniques, some of which performed in other centers, were TUS (7%), TUS and MRCP (63.1%), TUS and CT (10.5%) or TUS, MRCP and CT (19.3%). Abnormal EUS findings were observed in 12 patients (21%). As already described by other authors, causative identified lesions were periampullary diverticula, although a true compression on the CBD was rare (2/6), 2 ampullary adenoma, chronic pancreatitis according to predefined criteria[44] in 2 cases, a 7-mm biliary stone and one pancreatic cancer; 66.7% of patients were completely asymptomatic while unspecific abdominal pain or dyspepsia had been reported by the others. As suggested by the authors, a 21% prevalence of pathologic findings among patients with the aforementioned features, is probably overestimated since chronic pancreatitis and periampullary diverticula without bile duct indentation are not sure causes of biliary dilatation. Excluding these cases, the percentage is lower (10.5%) and comparable with Malik’s findings[3].
Recently, a retrospective study was performed by Rana et al[45] about EUS diagnostic accuracy in patients with unexplained dilatation of CBD on MRCP, in order to establish EUS yield in the clinical practice. Among the 40 selected patients, 10 subjects had elevated serum alkaline phosphatase while the others presented normal liver function tests: in the former group, EUS detected a pathological condition causing dilatation of CBD (stones, cholangiocarcinoma, benign strictures) compared to a minority of significant findings identified in patients with normal liver tests (33.3% received diagnosis for stones or chronic pancreatitis). The remnant 20 patients with dilatated biliary system and normal liver function had regular EUS findings. There was no difference in the mean duct diameter in subjects presenting elevated serum alkaline phosphatase compared to patients with normal liver function tests nor between groups with identified pathology or not. The authors concluded, as reported by previous scientific literature, that abnormal liver function tests are useful to identify patients with high pre-test probability of pathological findings underlying however that normal biochemistry does not exclude the existence of biliary ducts abnormalities.
Finally, Oppong et al[46] presented data retrospectively collected from a cohort of patients referred for EUS evaluation to a tertiary center. By excluding subjects with jaundice, liver function tests abnormalities, evidence of mass, stricture or ductal filling defect on pre-EUS imaging or symptoms suggestive of sphincter of Oddi dysfunction or chronic pancreatitis, they selected 40 patients with isolated dilatation of CBD. New findings on EUS were identified in 8 patients (20%). In 7 the following was considered as cause of dilatation: 3 had biliary polyps (not confirmed in 2 patients who later underwent ERCP), 3 had biliary stones and 1 had portal vein compression on the CBD. Microlithiasis, identified in the eighth subject, was assessed as a secondary event. Prior cholecystectomy was significantly more frequent in patients with no new findings on EUS, although CBD diameter did not differ among patients with prior surgery or not.
Changes in bile duct anatomy and adaptation of biliary system to normal or pathological processes, impose an accurate analysis of the patient anamnesis, liver biochemical parameters, clinical context in order to differentiate subjects with higher probability of biliary pathology from those with low index of suspicion. In recent years, the availability of a low-invasive modality, without post-procedural risk of pancreatitis, led to an increasing use of EUS in the investigation of biliary dilatation, even when symptoms or signs typically suggestive of obstruction were absent. On the other hand, the use of high-resolution cross-sectional imaging to investigate abdominal symptoms commonly results in increasing findings of dilatated biliary ducts in patients with normal liver tests. Currently, EUS program presents an increasing number of referrals in this setting and evidences in literature suggest a promising role for this technique in the identification of a potential biliary pathology, despite a low pre-test clinical suspicion. Firstly, in a small subset of patients, although asymptomatic or with vague symptoms, it can underlie pathologic conditions with dismal prognosis even with negative prior imaging tests. Secondly, according to the known high negative predictive value of EUS[47,48], if EUS evaluation does not identify the cause of biliary dilatation, the patient should be reassured and no further follow-up is recommended, since no pathologic conditions emerged during follow-up period in the aforementioned studies.
The authors thank Sharmila Fagoonee (Institute for Biostructures and Bioimages CNR c/o Molecular Biotechnology Center, University of Turin, Turin, Italy) for English revision of the manuscript.
P- Reviewer: Chen JQ, Hu H, Sharma SS S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Holm AN, Gerke H. What should be done with a dilated bile duct. Curr Gastroenterol Rep. 2010;12:150-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 2. | Bruno M, Brizzi RF, Mezzabotta L, Carucci P, Elia C, Gaia S, Mengozzi G, Romito AV, Eloubeidi MA, Rizzetto M. Unexplained common bile duct dilatation with normal serum liver enzymes: diagnostic yield of endoscopic ultrasound and follow-up of this condition. J Clin Gastroenterol. 2014;48:e67-e70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Malik S, Kaushik N, Khalid A, Bauer K, Brody D, Slivka A, McGrath K. EUS yield in evaluating biliary dilatation in patients with normal serum liver enzymes. Dig Dis Sci. 2007;52:508-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Cohen SM, Kurtz AB. Biliary sonography. Radiol Clin North Am. 1991;29:1171-1198. [PubMed] |
| 5. | Parulekar SG. Transabdominal sonography of bile ducts. Ultrasound Q. 2002;18:187-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Bowie JD. What is the upper limit of normal for the common bile duct on ultrasound: how much do you want it to be. Am J Gastroenterol. 2000;95:897-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Wu CC, Ho YH, Chen CY. Effect of aging on common bile duct diameter: a real-time ultrasonographic study. J Clin Ultrasound. 1984;12:473-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 57] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Horrow MM. Ultrasound of the extrahepatic bile duct: issues of size. Ultrasound Q. 2010;26:67-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Kaim A, Steinke K, Frank M, Enriquez R, Kirsch E, Bongartz G, Steinbrich W. Diameter of the common bile duct in the elderly patient: measurement by ultrasound. Eur Radiol. 1998;8:1413-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Perret RS, Sloop GD, Borne JA. Common bile duct measurements in an elderly population. J Ultrasound Med. 2000;19:727-730; quiz 731. [PubMed] |
| 11. | Coss A, Enns R. The investigation of unexplained biliary dilatation. Curr Gastroenterol Rep. 2009;11:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Bachar GN, Cohen M, Belenky A, Atar E, Gideon S. Effect of aging on the adult extrahepatic bile duct: a sonographic study. J Ultrasound Med. 2003;22:879-882; quiz 883-885. [PubMed] |
| 13. | Nakada I. Changes in morphology of the distal common bile duct associated with aging. Gastroenterol Jpn. 1981;16:54-63. [PubMed] |
| 14. | Kialian GP, Aznaurian AV. The age-related characteristics of the muscular layer of the common bile duct in man. Morfologiia. 1995;108:10-12. [PubMed] |
| 15. | Senturk S, Miroglu TC, Bilici A, Gumus H, Tekin RC, Ekici F, Tekbas G. Diameters of the common bile duct in adults and postcholecystectomy patients: a study with 64-slice CT. Eur J Radiol. 2012;81:39-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Benjaminov F, Leichtman G, Naftali T, Half EE, Konikoff FM. Effects of age and cholecystectomy on common bile duct diameter as measured by endoscopic ultrasonography. Surg Endosc. 2013;27:303-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Chawla S, Trick WE, Gilkey S, Attar BM. Does cholecystectomy status influence the common bile duct diameter A matched-pair analysis. Dig Dis Sci. 2010;55:1155-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Wu SD, Zhang ZH, Jin JZ, Kong J, Wang W, Zhang Q, Li DY, Wang MF. Effects of narcotic analgesic drugs on human Oddi’s sphincter motility. World J Gastroenterol. 2004;10:2901-2904. [PubMed] |
| 19. | Helm JF, Venu RP, Geenen JE, Hogan WJ, Dodds WJ, Toouli J, Arndorfer RC. Effects of morphine on the human sphincter of Oddi. Gut. 1988;29:1402-1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 96] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Farahmand H, PourGholami M, Fathollah MS. Chronic extrahepatic bile duct dilatation: sonographic screening in the patients with opioid addiction. Korean J Radiol. 2007;8:212-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Sharma SS, Ram S, Maharshi S, Shankar V, Katiyar P, Jhajharia A, Sardava V, Bhardwaj H. Pancreato-biliary Endoscopic Ultrasound in Opium Addicts Presenting with Abdominal Pain. Endosc Ultrasound. 2013;2:204-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Ledro-Cano D. Suspected choledocholithiasis: endoscopic ultrasound or magnetic resonance cholangio-pancreatography A systematic review. Eur J Gastroenterol Hepatol. 2007;19:1007-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Laing FC, Jeffrey RB, Wing VW, Nyberg DA. Biliary dilatation: defining the level and cause by real-time US. Radiology. 1986;160:39-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 95] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Baron RL. Common bile duct stones: reassessment of criteria for CT diagnosis. Radiology. 1987;162:419-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 66] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Palazzo L, Girollet PP, Salmeron M, Silvain C, Roseau G, Canard JM, Chaussade S, Couturier D, Paolaggi JA. Value of endoscopic ultrasonography in the diagnosis of common bile duct stones: comparison with surgical exploration and ERCP. Gastrointest Endosc. 1995;42:225-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 112] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 26. | Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, Yamamoto N, Hirano K, Komatsu Y, Tada M. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005;54:271-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 139] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 27. | Gan SI, Rajan E, Adler DG, Baron TH, Anderson MA, Cash BD, Davila RE, Dominitz JA, Harrison ME, Ikenberry SO. Role of EUS. Gastrointest Endosc. 2007;66:425-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 28. | Buscarini E, Tansini P, Vallisa D, Zambelli A, Buscarini L. EUS for suspected choledocholithiasis: do benefits outweigh costs A prospective, controlled study. Gastrointest Endosc. 2003;57:510-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 74] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 29. | Kohut M, Nowakowska-Duława E, Marek T, Kaczor R, Nowak A. Accuracy of linear endoscopic ultrasonography in the evaluation of patients with suspected common bile duct stones. Endoscopy. 2002;34:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Fernández-Esparrach G, Ginès A, Sánchez M, Pagés M, Pellisé M, Fernández-Cruz L, López-Boado MA, Quintó L, Navarro S, Sendino O. Comparison of endoscopic ultrasonography and magnetic resonance cholangiopancreatography in the diagnosis of pancreatobiliary diseases: a prospective study. Am J Gastroenterol. 2007;102:1632-1639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 31. | Tse F, Liu L, Barkun AN, Armstrong D, Moayyedi P. EUS: a meta-analysis of test performance in suspected choledocholithiasis. Gastrointest Endosc. 2008;67:235-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 32. | Scheiman JM, Carlos RC, Barnett JL, Elta GH, Nostrant TT, Chey WD, Francis IR, Nandi PS. Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease A prospective trial and cost analysis. Am J Gastroenterol. 2001;96:2900-2904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 133] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 33. | Visser BC, Suh I, Way LW, Kang SM. Congenital choledochal cysts in adults. Arch Surg. 2004;139:855-860; discussion 860-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 97] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 34. | Liu CL, Fan ST, Lo CM, Lam CM, Poon RT, Wong J. Choledochal cysts in adults. Arch Surg. 2002;137:465-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 35. | Liu YB, Wang JW, Devkota KR, Ji ZL, Li JT, Wang XA, Ma XM, Cai WL, Kong Y, Cao LP. Congenital choledochal cysts in adults: twenty-five-year experience. Chin Med J (Engl). 2007;120:1404-1407. [PubMed] |
| 36. | Law R, Topazian M. Diagnosis and treatment of choledochoceles. Clin Gastroenterol Hepatol. 2014;12:196-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 37. | Early DS, Acosta RD, Chandrasekhara V, Chathadi KV, Decker GA, Evans JA, Fanelli RD, Fisher DA, Fonkalsrud L, Hwang JH. Adverse events associated with EUS and EUS with FNA. Gastrointest Endosc. 2013;77:839-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 149] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 38. | Amouyal P, Palazzo L, Amouyal G, Ponsot P, Mompoint D, Vilgrain V, Gayet B, Fléjou JF, Paolaggi JA. Endosonography: promising method for diagnosis of extrahepatic cholestasis. Lancet. 1989;2:1195-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 64] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | de Lédinghen V, Lecesne R, Raymond JM, Gense V, Amouretti M, Drouillard J, Couzigou P, Silvain C. Diagnosis of choledocholithiasis: EUS or magnetic resonance cholangiography A prospective controlled study. Gastrointest Endosc. 1999;49:26-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 135] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 40. | Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V, Ben-Menachem T, Cash BD, Decker GA, Early DS, Fanelli RD. Complications of ERCP. Gastrointest Endosc. 2012;75:467-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 299] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 41. | Kim JE, Lee JK, Lee KT, Park DI, Hyun JG, Paik SW, Rhee JC, Choi KW, Lim JH. The clinical significance of common bile-duct dilatation in patients without biliary symptoms or causative lesions on ultrasonography. Endoscopy. 2001;33:495-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 42. | Carriere V, Conway J, Evans J, Shokoohi S, Mishra G. Which patients with dilated common bile and/or pancreatic ducts have positive findings on EUS. J Interv Gastroenterol. 2012;2:168-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 43. | Kwok A, Lau J, Jones DB. Role of endoscopic ultrasound in evaluation of unexplained common bile duct dilatation. Gastrointest Endosc. 2009;69:AB250. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 44. | Wallace MB, Hawes RH, Durkalski V, Chak A, Mallery S, Catalano MF, Wiersema MJ, Bhutani MS, Ciaccia D, Kochman ML. The reliability of EUS for the diagnosis of chronic pancreatitis: interobserver agreement among experienced endosonographers. Gastrointest Endosc. 2001;53:294-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 133] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 45. | Rana SS, Bhasin DK, Sharma V, Rao C, Gupta R, Singh K. Role of endoscopic ultrasound in evaluation of unexplained common bile duct dilatation on magnetic resonance cholangiopancreatography. Ann Gastroenterol. 2013;26:66-70. [PubMed] |
| 46. | Oppong KW, Mitra V, Scott J, Anderson K, Charnley RM, Bonnington S, Jaques B, White S, French JJ, Manas DM. Endoscopic ultrasound in patients with normal liver blood tests and unexplained dilatation of common bile duct and or pancreatic duct. Scand J Gastroenterol. 2014;49:473-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 47. | Catanzaro A, Richardson S, Veloso H, Isenberg GA, Wong RC, Sivak MV, Chak A. Long-term follow-up of patients with clinically indeterminate suspicion of pancreatic cancer and normal EUS. Gastrointest Endosc. 2003;58:836-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 48. | Klapman JB, Chang KJ, Lee JG, Nguyen P. Negative predictive value of endoscopic ultrasound in a large series of patients with a clinical suspicion of pancreatic cancer. Am J Gastroenterol. 2005;100:2658-2661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |