Published online Mar 16, 2015. doi: 10.4253/wjge.v7.i3.278
Peer-review started: August 15, 2014
First decision: September 16, 2014
Revised: January 20, 2015
Accepted: February 4, 2015
Article in press: February 9, 2015
Published online: March 16, 2015
Processing time: 217 Days and 7.9 Hours
AIM: To evaluate the success rates of performing therapy utilizing a rotational assisted enteroscopy device in endoscopic retrograde cholangiopancreatography (ERCP) in surgically altered anatomy patients.
METHODS: Between June 1, 2009 and November 8, 2012, we performed 42 ERCPs with the use of rotational enteroscopy for patients with altered anatomy (39 with gastric bypass Roux-en-Y, 2 with Billroth II gastrectomy, and 1 with hepaticojejunostomy associated with liver transplant). The indications for ERCP were: choledocholithiasis: 13 of 42 (30.9%), biliary obstruction suggested on imaging: 20 of 42 (47.6%), suspected sphincter of Oddi dysfunction: 4 of 42 (9.5%), abnormal liver enzymes: 1 of 42 (2.4%), ascending cholangitis: 2 of 42 (4.8%), and bile leak: 2 of 42 (4.8%). All procedures were completed with the Olympus SIF-Q180 enteroscope and the Endo-Ease Discovery SB overtube produced by Spirus Medical.
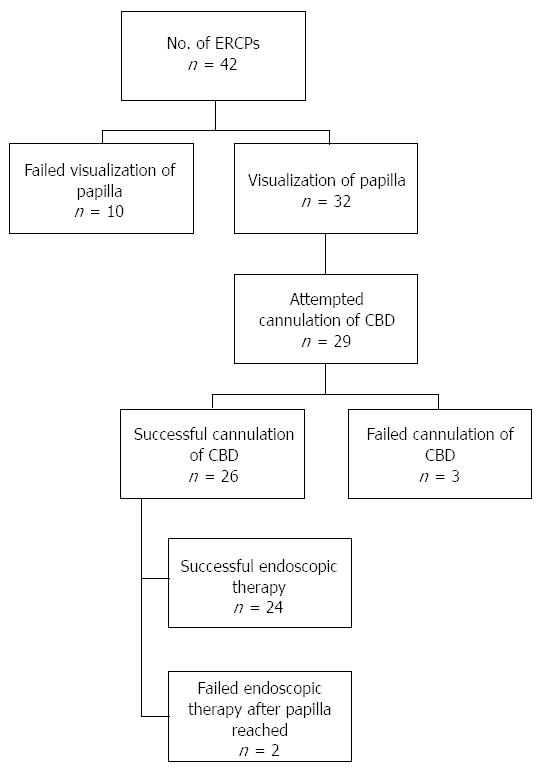
RESULTS: Successful visualization of the major ampulla was accomplished in 32 of 42 procedures (76.2%). Cannulation of the bile duct was successful in 26 of 32 procedures reaching the major ampulla (81.3%). Successful therapeutic intervention was completed in 24 of 26 procedures in which the bile duct was cannulated (92.3%). The overall intention to treat success rate was 64.3%. In terms of cannulation success, the intention to treat success rate was 61.5%. Ten out of forty two patients (23.8%) required admission to the hospital after procedure for abdominal pain and nausea, and 3 of those 10 patients (7.1%) had a diagnosis of post-ERCP pancreatitis. The average hospital stay was 3 d.
CONCLUSION: It is reasonable to consider an attempt at rotational assisted ERCP prior to a surgical intervention to alleviate biliary complications in patients with altered surgical anatomy.
Core tip: This manuscript shows a single tertiary care center experience in a large number of patients with surgically altered anatomy by evaluating the success rates of reaching the major ampulla, cannulating the bile duct, and subsequently performing therapy utilizing a rotational assisted enteroscopy device in an endoscopic retrograde cholangiopancreatography. This study will also determine the associated morbidity, mortality, and length of hospitalization associated with the procedures. Given our institutions success rates and minimal complication profile, specialized centers could consider this approach in this rapidly growing population. This will be instrumental in the development of new therapeutic options for patients suffering from this condition.
- Citation: Zouhairi ME, Watson JB, Desai SV, Swartz DK, Castillo-Roth A, Haque M, Jowell PS, Branch MS, Burbridge RA. Rotational assisted endoscopic retrograde cholangiopancreatography in patients with reconstructive gastrointestinal surgical anatomy. World J Gastrointest Endosc 2015; 7(3): 278-282
- URL: https://www.wjgnet.com/1948-5190/full/v7/i3/278.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i3.278
Endoscopic retrograde cholangiopancreatography (ERCP) remains the gold standard in both diagnosis and therapeutic management of pancreato-biliary diseases. However, patients with surgically altered anatomy present a unique endoscopic challenge. In patients with normal anatomy, rate of successful cannulation and sphincterotomy by expert endoscopists is greater than ninety percent[1]. In patients who have had reconstructive gastrointestinal surgery, reaching the ampulla and subsequently performing therapy during ERCP has been reported in a multicenter study to be 63%[2]. Additionally, as the obesity epidemic has widened in the United States, patients with altered anatomy due to bariatric surgery are increasingly presenting with the need for evaluation for pancreato-biliary disease[3].
Multiple methods have been described to gain access to the biliary tract in post surgical patients, which is particularly challenging because the standard duodenoscope cannot reach the ampulla due to increased distance of the Roux limb. Methods to gain biliary access with a standard duodenoscope, such as a surgically created gastrostomy have been previously described[4-6]. Non-surgical endoscopic methods using different types of enteroscopy techniques have also been described. These endoscopic techniques include double-balloon, single-balloon, and rotational assisted-ERCP (RA-ERCP)[7-9].
The goal of this retrospective study is to review a single tertiary care center experience in RA-ERCP in patients with reconstructive gastrointestinal surgery. Outcomes measured include the success rates of reaching the major ampulla, cannulating the bile duct, and subsequently performing a complete ERCP. Additionally, the associated morbidity, mortality, and length of hospitalization associated with RA-ERCP were measured.
An IRB approved retrospective review of all patients undergoing rotational assisted ERCP was performed.
Between June 1, 2009 and November 8, 2012, a total of 42 RA-ERCPs were attempted for patients with altered anatomy. Thirty-three of these patients underwent Roux-en-Y gastric bypass, 2 underwent Billroth II gastrectomy, and 1 underwent hepaticojejunostomy associated with liver transplant. A total of 6 patients had repeat procedures.
Sedation for the procedures were either moderate sedation (9 patients) or general anesthesia (33 patients) with the positioning of all patients in the prone position. An attending advanced endoscopist performed all procedures with the assistance of the advanced endoscopy fellow. A total of 4 attending physicians with experience in rotational assisted ERCP performed the procedures.
All RA-ERCPs were performed using an Olympus SIF-Q180 enteroscope and the Endo-Ease Discovery SB overtube manufactured by Spirus Medical.
Patients were not randomized, as the procedure was chosen based on availability and physician discretion. Procedural time for RA-ERCP was determined from the onset of the “time-out” patient verification to the time the patient arrived in the recovery bay.
The statistical methods of this study were reviewed by Majed El Zouhairi, MD and Rebecca Burbridge, MD from Duke University Medical Center.
Rotational enteroscopy was performed in forty-two separate procedures, in thirty-six patients with altered anatomy. Thirty-four patients were women (94.4%) and the mean age was 49.3 (range 29-75) (Table 1). The indications for ERCP were: biliary obstruction suggested on imaging 20 of 42 (47.6%), choledocholithiasis 13 of 42 (30.9%), suspected sphincter of Oddi dysfunction 4 of 42 (9.5%), ascending cholangitis 2 of 42 (4.8%), bile leak 2 of 42 (4.8%), and abnormal liver enzymes 1 of 42 (2.4%) (Table 2). The ability to reach and visualize the major ampulla was successful in 32 of 42 procedures (76.2%) (Figure 1). Attempted cannulation of the bile duct was performed in 29 out of the 32 procedures which successfully reached the major ampulla, with a subsequent bile duct cannulation rate of 89.7% (Figure 2). No attempt was made to cannulate the bile duct in three patients because procedures were only intended to remove previously placed stents. The reason for failed cannulation in the three patients in whom we were not able to cannulate the bile duct despite reaching the ampulla was an ampullary polyp (1 patient) and biliary stricture (2 patients). Successful therapeutic intervention including, but not limited to, sphincterotomy, stone removal, bile duct/pancreatic duct stent placement, balloon sweeping, and brushing was completed in 24 of 26 procedures in which the bile duct was cannulated (92.3%) (Figure 3). Of the total 42 cases, there were 15 failed cases, and 27 successful procedures, therefore the overall intention to treat success rate was 64.3%. In terms of cannulation success, 24 of 39 attempts at cannulation were successful, with an intention to treat success rate of 61.5%.
| No. of patients | 36 |
| No. of ERCPs | 42 |
| Age | 49.3 |
| Sex | M = 2, F = 34 |
| BMI | 36.3 |
| Roux-en-Y surgery patients | 33 |
| Billroth II surgery patients | 2 |
| Hepaticojejunostomy associated with liver transplant | 1 |
| Suspected gallstones/choledocholithiasis | 13 |
| Sphincter of Oddi dysfunction I/II | 1/3 |
| Biliary obstruction on imaging | 20 |
| Ascending cholangitis | 2 |
| Biliary obstruction with negative imaging | 1 |
| Bile leak | 2 |
Ten patients out of 42 procedures (23.8%) required hospital admission for abdominal pain and nausea following the procedure. Three of those 10 patients (7.1%) had a diagnosis of post-ERCP pancreatitis. The average hospital stay was 3 d (Table 3). There were no overtube related complications.
| Adverse events | 10 |
| No. of admission | 10 |
| Length of hospital stay after admission (d) | 3 |
Surgically altered anatomy has become increasingly more common in the United States, particularly due to bariatric surgery. Reaching the ampulla in patients with surgically altered anatomy remains challenging even for skilled endoscopists despite advances in deep small bowel enteroscopy. Currently, the standard of care for pancreato-biliary disease in these patients often involves surgical assistance to help access the major ampulla. Success rates with single-balloon[10-13] and double-balloon enteroscopy systems[2,14-19] have been reported to range from 60% to 88%[2]. In limited studies, RA-ERCP has been shown to be a promising technique for pancreato-biliary access in post surgical patients. Hegde et al[7] reported that RA-ERCP allowed successful cannulation in 2 patients after double-balloon assisted ERCP had failed, but that it was more time-consuming. Al-Lehibi et al[8], also noted that RA-ERCP was successful in 5 of 6 cases. A recent prospective study reported in 2012 by Wagh et al[9] on 13 patients showed that cannulation of the desired duct and endoscopic therapy using RA-ERCP in patients with surgically altered anatomy was successful in 90% of the procedures if the papilla/duct-enterostomy was reached.
A recent multi-center retrospective study published in January 2013 by Shah et al[2] compared ERCP success in 129 patients with surgically altered anatomy utilizing single-balloon (SBE), double-balloon (DBE), or rotational overtube enteroscopy. Fifty-seven RA-ERCP cases were performed with an intention to treat success rate of 63%, defined as successful planned therapeutic intervention. They concluded that therapeutic success in long-limb surgical bypass was similar irregardless of the endoscopic method used.
Our study is the largest single-center experience evaluating RA-ERCP in patients with reconstructed gastrointestinal anatomy. We noted RA-ERCP procedural success rate in visualizing the ampulla of 76.2%, cannulating the bile duct in procedures reaching the major ampulla of 81.3%, and successfully completing therapeutic interventions after cannulating the major ampulla of 92.3% with an overall intention to treat success rate of 61.5%. This seems consistent with the rate published by Shah et al[2], and would suggest that RA-ERCP is on par with other non-surgical endoscopic techniques.
Limitations of this study include the lack of direct comparison with other deep enteroscopy techniques. A second limitation is that all procedures were performed in a tertiary-care center which may not be generalizable to smaller gastroenterology practices which serve a local community. Additionally, the strength of one specific endoscopic technique for non-ERCP enteroscopy has not been consistently demonstrated. The concept that experience may play an important role in success is supported by data from the non-ERCP enteroscopy literature. For example the efficacy of double balloon compared to rotation assisted enteroscopy is still debatable and experience in either modality may be more important than the type of enteroscopy modality chosen[20-22].
Given our institution’s success rates and minimal complication profile, we believe it is reasonable to consider an attempt at rotational assisted ERCP prior to a surgical intervention to evaluate pancreato-biliary diseases in patients with altered surgical anatomy. Our data, as well as other smaller studies, have confirmed the safety and relative efficacy of this approach. In determining the method of endoscopic approach to ERCP in post surgical patients, relative experience with other enteroscopy modalities such as DBE or SBE should also be considered.
Endoscopic retrograde cholangiopancreatography (ERCP) has been a mainstay in the diagnosis and management of pancreato-biliary diseases. With the use of a standard duodenoscope, success rates are greater than ninety percent in patients with normal gastrointestinal anatomy. However, reaching the ampulla and subsequently performing therapy during ERCP is difficult in patients with surgically altered anatomy. Utilizing a rotational enteroscopy device to assist in reaching the ampulla in this population may increase the chances of being able to successfully complete the procedure.
There have been only a few small number of studies examining the use of RA-ERCP in approaching biliary complications in patients with Roux-en-Y gastric bypass surgery.
This manuscript shows a single tertiary care center experience in a large number of patients with surgically altered anatomy by evaluating the success rates of reaching the major ampulla, cannulating the bile duct, and subsequently performing therapy utilizing a rotational assisted enteroscopy device in order to complete an ERCP. This study will also determine the associated morbidity, mortality, and length of hospitalization associated with the procedures.
Surgically altered anatomy has become increasingly more common in the United States, particularly due to bariatric surgery. Currently, the standard of care for pancreatico-biliary complications in these patients often involves surgical assistance to help access the major ampulla. Given our institutions success rates and minimal complication profile, the authors believe it is reasonable to consider an attempt at rotational assisted ERCP prior to a surgical intervention to alleviate biliary complications in patients with altered surgical anatomy.
ERCP; rotational assisted-ERCP (RA-ERCP); single-balloon enteroscopy (SBE); double-balloon enteroscopy (DBE).
This paper is interesting.
P- Reviewer: Murata A, Tekin A S- Editor: Ji FF L- Editor: A E- Editor: Zhang DN
| 1. | Huibregtse K, Kimmey MB. Endoscopic retrograde cholangiopancreatography, endoscopic sphincterotomy and stone removal, and endoscopic biliary and pancreatic drainage. Textbook of gastroenterology. Philadelphia: J.B. Lippincott 1995; 2590-2617. |
| 2. | Shah RJ, Smolkin M, Yen R, Ross A, Kozarek RA, Howell DA, Bakis G, Jonnalagadda SS, Al-Lehibi AA, Hardy A. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc. 2013;77:593-600. |
| 3. | Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, Lamonte MJ, Stroup AM, Hunt SC. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753-761. |
| 4. | Baron TH, Vickers SM. Surgical gastrostomy placement as access for diagnostic and therapeutic ERCP. Gastrointest Endosc. 1998;48:640-641. |
| 5. | Peters M, Papasavas PK, Caushaj PF, Kania RJ, Gagné DJ. Laparoscopic transgastric endoscopic retrograde cholangiopancreatography for benign common bile duct stricture after Roux-en-Y gastric bypass. Surg Endosc. 2002;16:1106. |
| 6. | Lopes TL, Wilcox CM. Endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y anatomy. Gastroenterol Clin North Am. 2010;39:99-107. |
| 7. | Hegde SR, Downey S, Iffrig K, Heller SJ, Tokar JF, Haluszka O. Overtube-assisted ERCP in patients with surgically altered anatomy: a single center one-year experience [abstract]. Gastrointest Endosc. 2009;69 AB193. |
| 8. | Al-Lehibi AH, Kumar N, Sayuk GS, Ammar T, Murad F, Mullady D, Early DS, Azar RR, Edmundowicz SA, Jonnalagadda SS. Success rates for endoscopic retrograde cholangiopancreatography (ERCP) in patients with altered anatomy from prior surgical intervention [abstract]. Gastrointest Endosc. 2010;71:AB228. |
| 9. | Wagh MS, Draganov PV. Prospective evaluation of spiral overtube-assisted ERCP in patients with surgically altered anatomy. Gastrointest Endosc. 2012;76:439-443. |
| 10. | Dellon ES, Kohn GP, Morgan DR, Grimm IS. Endoscopic retrograde cholangiopancreatography with single-balloon enteroscopy is feasible in patients with a prior Roux-en-Y anastomosis. Dig Dis Sci. 2009;54:1798-1803. |
| 11. | Mönkemüller K, Fry LC, Bellutti M, Neumann H, Malfertheiner P. ERCP using single-balloon instead of double-balloon enteroscopy in patients with Roux-en-Y anastomosis. Endoscopy. 2008;40 Suppl 2:E19-E20. |
| 12. | Neumann H, Fry LC, Meyer F, Malfertheiner P, Monkemuller K. Endoscopic retrograde cholangiopancreatography using the single balloon enteroscope technique in patients with Roux-en-Y anastomosis. Digestion. 2009;80:52-57. |
| 13. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010;105:93-99. |
| 14. | Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc. 2007;66:1038-1041. |
| 15. | Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39:1068-1071. |
| 16. | Mönkemüller K, Bellutti M, Neumann H, Malfertheiner P. Therapeutic ERCP with the double-balloon enteroscope in patients with Roux-en-Y anastomosis. Gastrointest Endosc. 2008;67:992-996. |
| 17. | Maaser C, Lenze F, Bokemeyer M, Ullerich H, Domagk D, Bruewer M, Luegering A, Domschke W, Kucharzik T. Double balloon enteroscopy: a useful tool for diagnostic and therapeutic procedures in the pancreaticobiliary system. Am J Gastroenterol. 2008;103:894-900. |
| 18. | Chu YC, Yang CC, Yeh YH, Chen CH, Yueh SK. Double-balloon enteroscopy application in biliary tract disease-its therapeutic and diagnostic functions. Gastrointest Endosc. 2008;68:585-591. |
| 19. | Iwamoto S, Ryozawa S, Yamamoto H, Taba K, Ishigaki N, Harano M, Iwano H, Sakaida I. Double balloon endoscope facilitates endoscopic retrograde cholangiopancreatography in roux-en-y anastomosis patients. Dig Endosc. 2010;22:64-68. |
| 20. | Khashab MA, Lennon AM, Dunbar KB, Singh VK, Chandrasekhara V, Giday S, Canto MI, Buscaglia JM, Kapoor S, Shin EJ. A comparative evaluation of single-balloon enteroscopy and spiral enteroscopy for patients with mid-gut disorders. Gastrointest Endosc. 2010;72:766-772. |
| 21. | Messer I, May A, Manner H, Ell C. Prospective, randomized, single-center trial comparing double-balloon enteroscopy and spiral enteroscopy in patients with suspected small-bowel disorders. Gastrointest Endosc. 2013;77:241-249. |
| 22. | Akerman PA. Spiral enteroscopy versus double-balloon enteroscopy: choosing the right tool for the job. Gastrointest Endosc. 2013;77:252-254. |