Published online Sep 16, 2014. doi: 10.4253/wjge.v6.i9.415
Revised: July 22, 2014
Accepted: September 4, 2014
Published online: September 16, 2014
Processing time: 125 Days and 8 Hours
Ventriculoperitoneal shunting (VPS) is a widely accepted technique for the treatment of hydrocephalus. The probability of shunt dysfunction is pretty high throughout life. Laparoscopy has become a valuable tool to perform VPS and treat abdominal complications. An electronic literature search was performed to reveal the published data relating laparoscopy and ventriculoperitoneal shunt in Medline, Embase, Scielo and Lilacs databases. The keywords employed were “laparoscopy” OR “laparoscopic surgery” AND “ventriculoperitoneal shunt” OR “shunt” AND “surgery” OR “implantation” OR “revision” OR “complication”. No high quality trials were developed comparing conventional laparotomic incision vs laparoscopic approach. Both approaches have evolved and currently there are less invasive options for laparotomy, like periumbilical small incisions; and for laparoscopy, like smaller and less incisions. Operating room time, blood loss and hospital stay may be potentially smaller in laparoscopic surgery and complications are probably the same as laparotomy. In revision surgery for abdominal complications after VPS, visualization of whole abdominal cavity is fundamental to address properly the problem and laparoscopic approach is valuable once it is safe, fast and much less invasive than laparotomy. Ventriculoperitoneal shunting is a widely accepted technique for the treatment of hydrocephalus. Laparoscopy assisted shunt surgery in selected cases might be a less invasive and more effective option for intrabdominal manipulation. The laparoscopic approach allows a better catheter positioning, lysis of fibrotic bundles and peritoneal inspection as well, without any additional complication.
Core tip: Review of application of laparoscopy in ventriculoperitoneal surgery.
- Citation: Pinto FCG, de Oliveira MF. Laparoscopy for ventriculoperitoneal shunt implantation and revision surgery. World J Gastrointest Endosc 2014; 6(9): 415-418
- URL: https://www.wjgnet.com/1948-5190/full/v6/i9/415.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i9.415
Shunt surgery represents a paramount procedure in neurosurgical practice, as the most widely performed central nervous system surgery. The preferred modality is the ventriculoperitoneal shunt (VPS), which connects the lateral ventricles and the peritoneal cavity[1-4].
Up to 80% of shunts implanted for treatment of hydrocephalus may fail at some point during the patient’s life, with approximately 30% failing within the first year. Although shunt placement is a common procedure and is considered safe, several complications may occur. Shunt-related complications, such as obstruction, overdrainage, loculation, and infection, sometimes require challenging surgical approaches associated with increased morbidity[1-6].
Abdominal complications of VPS are not rare, and the common mechanism involves epithelial responses to the presence of the catheter, which cause peritoneal retraction, intra-abdominal cerebrospinal fluid (CSF) collections, and adhesions. These complications usually worsen with multiple peritoneal revisions, sometimes resulting in peritoneal sclerosis that make further shunt implantation infeasible[7].
Within this context, the laparoscopic approach has grown in popularity as an alternative method for shunt implantation and especially for revision surgery after abdominal complications. This paper summarizes current concepts about its application.
A critical review of the literature was performed after searching the MEDLINE, Embase, SciELO, and LILACS databases for published data on laparoscopy and ventriculoperitoneal shunting. The search query employed was “laparoscopy” OR “laparoscopic surgery” AND “ventriculoperitoneal shunt” OR “shunt” AND “surgery” OR “implantation” OR “revision” OR “complication”.
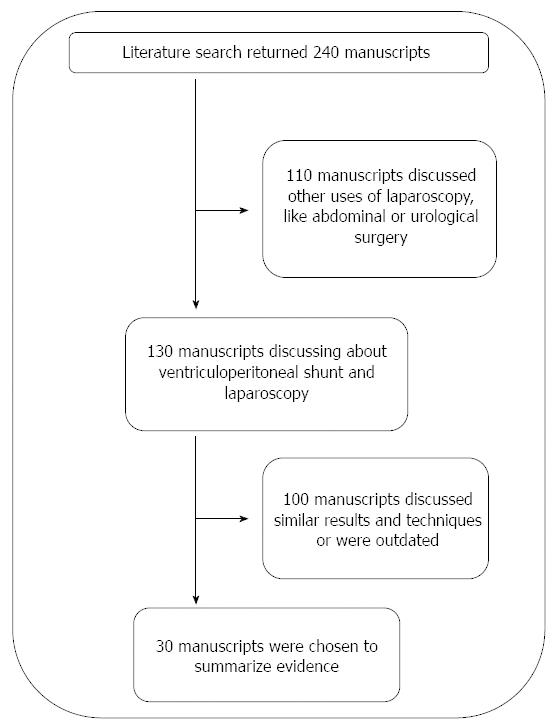
We selected all papers in english, spanish and portuguese. The above search strategy yielded 240 manuscripts. Of these, 110 discussed other uses of laparoscopy not related to ventriculoperitoneal shunting, such as laparoscopy for abdominal and urological surgery. One hundred and thirty papers addressed the topic of interest. As some of these articles presented outdated data or very similar discussions, we selected 30 up-to-date manuscripts discussing different points of view to summarize recent, pertinent information about applications of laparoscopic surgery in ventriculoperitoneal shunting (Figure 1).
Several reports highlight the utility of the laparoscopic approach for abdominal shunt insertion through less invasive incisions[8-10]. No high-quality trials were found comparing conventional laparotomy vs laparoscopic approaches. The rationale supporting conventional laparotomy includes factors such as the simple learning curve, as it can be performed by neurosurgeons, and its established success rate. The rationale for laparoscopic approaches includes wide view of catheter implantation, ability to choose the best site for fixation, and confirmation of patency[11-15].
Both approaches have evolved. Currently, less invasive options are available both for laparotomy - such as small periumbilical incisions - and for laparoscopy, such as smaller and fewer incisions using 2-mm trocars[16-20].
Operating room time, blood loss, and hospital stay may be reduced in laparoscopic surgery, and complications are probably the same as with laparotomy[19].
In revision surgery for abdominal complications after VPS, the main findings may be abdominal adhesions, peritoneal thickening and retraction, and CSF pseudocysts. Additionally, after complicated VPS, catheter malfunctioning may occur due to migration, occlusion, and presence of foreign bodies[8,21-23].
In such scenarios, visualization of the whole abdominal cavity is essential to addressing the issue properly. The laparoscopic approach is valuable in this setting because it is safe, fast, and much less invasive than laparotomy, and is thus associated with fewer complications[24-27].
Ventriculoperitoneal shunting is a widely accepted technique for the treatment of hydrocephalus. The standard procedure to insert the peritoneal catheter requires an abdominal incision, muscle dissection, and opening of the peritoneum. The probability of lifetime shunt dysfunction is quite high. Abdominal complications are major causes of dysfunction. The peritoneal space is forced to accommodate a foreign body (catheter) and receive the flow of approximately 21 mL of CSF per hour, resulting in epithelial responses which may lead to inflammation and obstruction[1-4].
Several alternative procedures have been reported as temporary or permanent solutions to VPS failure, such as catheter implantation in other distal sites in the cervical, thoracic, and abdominal regions. The ventriculo-omental bursa shunt, with catheter insertion through the foramen of Winslow, has been described, even in cases of peritonitis or peritoneum adhesion. However, all of these options are considered third-line procedures, due to their higher complexity and high complication rates[27].
Laparoscopic-assisted surgery has become an useful option, as it allows abdominal exploration with shorter surgical time and complications. In 1993, Armbruster et al[10] and Basauri et al[11] described the laparoscopically assisted implantation of ventriculoperitoneal shunts, and in 1995, Kim first described the laparoscopic management of an abdominal complication[11,21].
On the other hand, laparoscopic surgery for other purposes may interfere with VPS function and even cause obstruction. The impaction of soft tissue or air within the distal catheter as a consequence of peritoneal insufflation may cause shunt obstruction[28]. Furthermore, increased abdominal pressure may have a negative effect on intracranial pressure (ICP). Human data on the effects of laparoscopy on ICP are lacking, but ICP increases significantly with abdominal insufflation and correlates with laparoscopic insufflation pressure. Thus, laparoscopy should be performed cautiously in patients with elevated baseline ICP[29].
In conclusion, we believe that laparoscopic-assisted shunt surgery in selected cases might be a less invasive and more effective option for intra-abdominal manipulation. The laparoscopic approach also enables better catheter positioning, lysis of fibrotic bundles, and peritoneal inspection without any additional complications.
P- Reviewer: Piccolo G, Ieiri S, Soria F, Sandblom G S- Editor: Ji FF L- Editor: A E- Editor: Zhang DN
| 1. | Browd SR, Ragel BT, Gottfried ON, Kestle JR. Failure of cerebrospinal fluid shunts: part I: Obstruction and mechanical failure. Pediatr Neurol. 2006;34:83-92. [Cited in This Article: ] |
| 2. | Lo P, Drake JM. Shunt malfunctions. Neurosurg Clin N Am. 2001;12:695-701, viii. [Cited in This Article: ] |
| 3. | Berry JG, Hall MA, Sharma V, Goumnerova L, Slonim AD, Shah SS. A multi-institutional, 5-year analysis of initial and multiple ventricular shunt revisions in children. Neurosurgery. 2008;62:445-453; discussion 453-454. [Cited in This Article: ] |
| 4. | Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F, Piatt J, Haines S, Schiff S, Cochrane D. Long-term follow-up data from the Shunt Design Trial. Pediatr Neurosurg. 2000;33:230-236. [Cited in This Article: ] |
| 5. | Kulkarni AV, Shams I. Quality of life in children with hydrocephalus: results from the Hospital for Sick Children, Toronto. J Neurosurg. 2007;107:358-364. [Cited in This Article: ] |
| 6. | Yung S, Chan TM. Pathophysiological changes to the peritoneal membrane during PD-related peritonitis: the role of mesothelial cells. Mediators Inflamm. 2012;2012:484167. [Cited in This Article: ] |
| 7. | Chung JJ, Yu JS, Kim JH, Nam SJ, Kim MJ. Intraabdominal complications secondary to ventriculoperitoneal shunts: CT findings and review of the literature. AJR Am J Roentgenol. 2009;193:1311-1317. [Cited in This Article: ] |
| 8. | Martin K, Baird R, Farmer JP, Emil S, Laberge JM, Shaw K, Puligandla P. The use of laparoscopy in ventriculoperitoneal shunt revisions. J Pediatr Surg. 2011;46:2146-2150. [Cited in This Article: ] |
| 9. | Bhasin RR, Chen MK, Pincus DW. Salvaging the “lost peritoneum” after ventriculoatrial shunt failures. Childs Nerv Syst. 2007;23:483-486. [Cited in This Article: ] |
| 10. | Armbruster C, Blauensteiner J, Ammerer HP, Kriwanek S. Laparoscopically assisted implantation of ventriculoperitoneal shunts. J Laparoendosc Surg. 1993;3:191-192. [Cited in This Article: ] |
| 11. | Basauri L, Selman JM, Lizana C. Peritoneal catheter insertion using laparoscopic guidance. Pediatr Neurosurg. 1993;19:109-110. [Cited in This Article: ] |
| 12. | Shao Y, Li M, Sun JL, Wang P, Li XK, Zhang QL, Zhang L. A laparoscopic approach to ventriculoperitoneal shunt placement with a novel fixation method for distal shunt catheter in the treatment of hydrocephalus. Minim Invasive Neurosurg. 2011;54:44-47. [Cited in This Article: ] |
| 13. | Raysi Dehcordi S, De Tommasi C, Ricci A, Marzi S, Ruscitti C, Amicucci G, Galzio RJ. Laparoscopy-assisted ventriculoperitoneal shunt surgery: personal experience and review of the literature. Neurosurg Rev. 2011;34:363-370; discussion 370-371. [Cited in This Article: ] |
| 14. | Hong WC, Lai PS, Chien YH, Tu YK, Tsai JC. Single-Incision laparoscopic surgery (SILS) for ventriculoperitoneal shunt placement. J Neurol Surg A Cent Eur Neurosurg. 2013;74:351-356. [Cited in This Article: ] |
| 15. | Roth J, Sagie B, Szold A, Elran H. Laparoscopic versus non-laparoscopic-assisted ventriculoperitoneal shunt placement in adults. A retrospective analysis. Surg Neurol. 2007;68:177-184; discussion 184. [Cited in This Article: ] |
| 16. | Kurschel S, Eder HG, Schleef J. CSF shunts in children: endoscopically-assisted placement of the distal catheter. Childs Nerv Syst. 2005;21:52-55. [Cited in This Article: ] |
| 17. | Reardon PR, Scarborough TK, Matthews BD, Marti JL, Preciado A. Laparoscopically assisted ventriculoperitoneal shunt placement using 2-mm instrumentation. Surg Endosc. 2000;14:585-586. [Cited in This Article: ] |
| 18. | Park YS, Park IS, Park KB, Lee CH, Hwang SH, Han JW. Laparotomy versus Laparoscopic Placement of Distal Catheter in Ventriculoperitoneal Shunt Procedure. J Korean Neurosurg Soc. 2010;48:325-329. [Cited in This Article: ] |
| 19. | Argo JL, Yellumahanthi DK, Ballem N, Harrigan MR, Fisher WS, Wesley MM, Taylor TH, Clements RH. Laparoscopic versus open approach for implantation of the peritoneal catheter during ventriculoperitoneal shunt placement. Surg Endosc. 2009;23:1449-1455. [Cited in This Article: ] |
| 20. | Handler MH, Callahan B. Laparoscopic placement of distal ventriculoperitoneal shunt catheters. J Neurosurg Pediatr. 2008;2:282-285. [Cited in This Article: ] |
| 21. | Kim HB, Raghavendran K, Kleinhaus S. Management of an abdominal cerebrospinal fluid pseudocyst using laparoscopic techniques. Surg Laparosc Endosc. 1995;5:151-154. [Cited in This Article: ] |
| 22. | Johnson BW, Pimpalwar A. Laparoscopic-assisted placement of ventriculo-peritoneal shunt tips in children with multiple previous open abdominal ventriculo-peritoneal shunt surgeries. Eur J Pediatr Surg. 2009;19:79-82. [Cited in This Article: ] |
| 23. | Potineni LB, Hartin CW, Gemme S, Caty MG, Bass KD. Laparoscopic assessment of a migrated ventriculoperitoneal shunt into an inguinal hernia. J Laparoendosc Adv Surg Tech A. 2012;22:301-303. [Cited in This Article: ] |
| 24. | de Carvalho FO, Bellas AR, Guimarães L, Salomão JF. Laparoscopic assisted ventriculoperitoneal shunt revisions as an option for pediatric patients with previous intraabdominal complications. Arq Neuropsiquiatr. 2014;72:307-311. [Cited in This Article: ] |
| 25. | Schukfeh N, Tschan CA, Kuebler JF, Hermann EJ, Nustede R, Krauss JK, Ure B, Glüer S. Laparoscopically assisted ventriculoperitoneal shunt placement in infants with previous multiple abdominal operations. Eur J Pediatr Surg. 2009;19:168-170. [Cited in This Article: ] |
| 26. | Nfonsam V, Chand B, Rosenblatt S, Turner R, Luciano M. Laparoscopic management of distal ventriculoperitoneal shunt complications. Surg Endosc. 2008;22:1866-1870. [Cited in This Article: ] |
| 27. | Matushita H, Cardeal D, Pinto FC, Plese JP, de Miranda JS. The ventriculoomental bursa shunt. Childs Nerv Syst. 2008;24:949-953. [Cited in This Article: ] |