Published online May 16, 2014. doi: 10.4253/wjge.v6.i5.200
Revised: March 12, 2014
Accepted: April 25, 2014
Published online: May 16, 2014
Processing time: 240 Days and 16.5 Hours
AIM: To study the cannulation and complication rates of early pre-cut sphincterotomy vs persistent attempts at cannulation by standard approach.
METHODS: Systematic search of PubMed, EMBASE, Web of Science, and the Cochrane Library for relevant studies published up to February 2013. The main outcome measurements were cannulation rates and post-endoscopic retrograde cholangiopancreatography (ERCP) complications. A comprehensive systematic search of the Cochrane library, PubMed, Google scholar, Scopus, National Institutes of Health, meta-register of controlled trials and published proceedings from major Gastroenterology journals and meetings until February 2013 was conducted using keywords. All Prospective randomized controlled trials (RCT) studies which met our inclusion criteria were included in the analysis. Prospective non-randomized studies and retrospective studies were excluded from our meta-analysis. The main outcomes of interest were post-ERCP pancreatitis, overall complication rates including cholangitis, ERCP-related bleeding, perforation and cannulation success rates.
RESULTS: Seven RCTs with a total of 1039 patients were included in the meta-analysis based on selection criteria. The overall cannulation rate was 90% in the pre-cut sphincterotomy vs 86.3% in the persistent attempts group (OR = 1.98; 95%CI: 0.70-5.65). The risk of post-ERCP pancreatitis (PEP) was not different between the two groups (3.9% in the pre-cut sphincterotomy vs 6.1% in the persistent attempts group, OR = 0.58, 95%CI: 0.32-1.05). Similarly, there was no statistically significant difference between the groups for overall complication rate including PEP, cholangitis, bleeding, and perforation (6.2% vs 6.9%, OR = 0.85, 95%CI: 0.51-1.41).
CONCLUSION: This meta-analysis suggests that pre-cut sphincterotomy and persistent attempts at cannulation are comparable in terms of overall complication rates. Early pre-cut implementation does not increase PEP complications.
Core tip: Selective cannulation of the bile duct remains the limiting step in therapeutic post-endoscopic retrograde cholangiopancreatography (ERCP). Greater than 90% of cannulation is achieved through standard techniques. In 10% of patients, cannulation is difficult and requires additional techniques such as pre-cut sphincterotomy. Early use of pre-cut sphincterotomy is suggested as a means to prevent excessive and repetitive papillary trauma which may in turn increase the risk of post-ERCP pancreatitis. The use of pre-cut sphincterotomy has been considered to increase risk of post-ERCP complications, in particular post-ERCP pancreatitis. We studied the literature on the use of pre-cut sphincterotomy in biliary access. Our meta-analysis showed that pre-cut sphincterotomy and persistent attempts at cannulation are comparable in terms of overall complication rates including post-ERCP pancreatitis. Early pre-cut implementation does not increase PEP complications.
- Citation: Navaneethan U, Konjeti R, Venkatesh PG, Sanaka MR, Parsi MA. Early precut sphincterotomy and the risk of endoscopic retrograde cholangiopancreatography related complications: An updated meta-analysis. World J Gastrointest Endosc 2014; 6(5): 200-208
- URL: https://www.wjgnet.com/1948-5190/full/v6/i5/200.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i5.200
Endoscopic retrograde cholangiopancreatography (ERCP) has been widely used for treatment of a variety of biliary disorders and cannulation of the bile duct remains one of the most important steps for successful therapeutic endoscopy. The success of biliary cannulation depends on several factors including patient anatomy, utilization of specialized catheters, and the skill and experience of the endoscopist[1]. Deep biliary cannulation by an experienced endoscopist using standard cannulation techniques is successful in approximately 90% of the cases[1]. Biliary cannulation becomes difficult in about 5%-10% of the cases[2,3] especially in patients with abnormal anatomy, ampullary or pancreatic tumors, and periampullary diverticuli. Precut sphincterotomy, also referred to as needle knife sphincterotomy (NKS), has been advocated in situations where routine biliary cannulation has been unsuccessful. The presumed risks and morbidity associated with NKS, particularly risk of post-ERCP pancreatitis (PEP) has discouraged use of this technique in patients with difficult biliary access[4]. The assessment of this risk, however, is confounded by pre-cut sphincterotomy being done as a last resort after repeated failed attempts at biliary cannulation and in some cases repeated inadvertent pancreatic duct (PD) cannulations. Repeated failed attempts at biliary cannulation and repeated pancreatic duct cannulations have been shown to be independently associated with a higher incidence of PEP[5-7]. In addition to PEP, reported complications of NKS are bleeding[8] and perforation[9]. The main goal of therapeutic ERCP is to achieve biliary cannulation with least possible adverse events. Early use of pre-cut sphincterotomy is suggested as a means to prevent excessive and repetitive papillary trauma which may in turn increase the risk of PEP. The few randomized controlled trials (RCTs) that have tried to assess the differences in the complication rates between early pre-cut sphincterotomy and persistent cannulation groups, have shown variable results and are limited by small number of patients and therefore inadequate power to demonstrate any potential differences between the groups[10-12].
An earlier meta-analysis demonstrated that early precut sphincterotomy reduces PEP risk but not the overall complication rate or cannulation success[13]. Subsequent to this publication, another RCT has been published[14]. This study showed that early use of NKS during difficult cannulation does not increase the risk of PEP. Given the importance of this topic for the clinical practice of ERCP, we sought to perform an updated meta-analysis to study the differences in cannulation rates, PEP and overall complication risk between early pre-cut sphincterotomy and persistent attempts at cannulation, taking the new randomized study into consideration.
Two authors (Navaneethan U, Konjeti R) independently conducted a comprehensive search of the Cochrane library, PUBMED, Google scholar, Scopus, National Institutes of Health, meta-register of controlled trials and published proceedings from major Gastroenterology journals and meetings until February 2013. The search was conducted using the key words endoscopic retrograde cholangiopancreatography, ERCP, precut, cannulation, needle-knife, papillotomy, sphincterotomy, fistulotomy. All relevant articles irrespective of language, year of publication, type of publication, or publication status were included. The titles and abstracts of all potentially relevant studies were screened for eligibility. The reference lists of studies of interest were then manually reviewed for additional articles. In the case of studies with incomplete information, the principal authors were contacted to obtain additional data.
We applied the following inclusion criteria for identifying studies for our analysis: (1) prospective RCTs comparing cannulation techniques: “early precut” group in which precutting was done early during the procedure and the “persistent attempts” group in which persistent attempts were made with standard cannulation; and (2) Comparison of major complications (PEP, cholangitis, ERCP-related bleeding and perforation) between the two groups. Our outcomes of interest were PEP, overall complication rates and cannulation rates. Prospective non-randomized studies and retrospective studies were excluded from our meta-analysis.
The quality of the studies was assessed according to quality criteria (Table 1). Simple and direct questions were organized to investigate each quality measure by two independent investigators (Navaneethan U, Konjeti R).
| Ref. | Were patients randomized | Was generation of allocation sequence adequate | Eligibility criteria mentioned | Both patients and clinicians blinded | Participants baseline characteristics similar in both groups | Treatment allocation concealed | Study adequately powered to asses significant clinical outcome |
| Tang et al[10] | Yes | Yes | Yes | Partially fulfilled | Yes | Yes | No |
| Zhou et al[19] | Yes | Yes | Partially | Partially fulfilled | Yes | Yes | N/A |
| de Weerth et al[12] | Yes | N/A | Yes | Partially fulfilled | Yes | N/A | N/A |
| Khatibian et al[18] | Yes | Yes | Yes | Partially fulfilled | Yes | Yes | Partially |
| Manes et al[20] | Yes | Yes | Yes | Partially fulfilled | Yes | N/A | No |
| Cennamo et al[11] | Yes | Yes | Yes | Partially fulfilled | Yes | Yes | No |
| Swan et al[14] | Yes | Yes | Yes | Yes | Yes | Yes | No |
Data was extracted by two independent reviewers with discrepancies settled by a third investigator (Sanaka MR). We performed the review and meta-analyses following the recommendations of The Cochrane Collaboration[15]. The analyses were performed using RevMan version 5.1. Binary outcomes were expressed as relative risks (RR) and continuous outcomes as median or mean difference, with 95%CI. Data was analyzed by fixed or random-effects model depending on heterogeneity[16]. Regression analyses were performed to estimate funnel plot asymmetry[17]. In our analysis, heterogeneity was explored by the chi-square test, with significance set at a P value of 0.05, and measured by I[15]. A sensitivity analysis using random effects models for the overall deep-biliary cannulation rate was also performed.
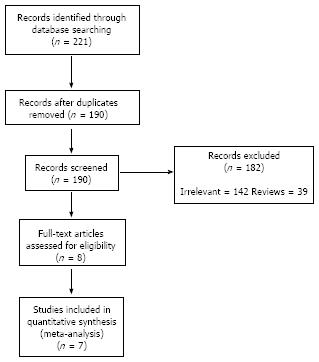
Two-hundred and twenty one potentially relevant studies were identified by our primary search of the electronic databases for published work on the subject. Of these studies, 214 were excluded after further review of the title and abstract for irrelevant topics, duplication of the reports, prospective non-RCTs or not meeting inclusion criteria. After careful review, 7 RCTs were eligible for meta-analysis. The detailed process of this literature search is shown in Figure 1. The characteristic of each included study is shown in Table 2.
| Ref. | Country | Center involved | No. of patients screened | Patients allocated to early precut/persistent attempts |
| Tang et al[10] | Canada | Single center | 642 | 32/30 |
| Zhou et al[19] | China | Single center | 948 | 43/48 |
| de Weerth et al[12] | Germany | Single center | 291 | 145/146 |
| Khatibian et al[18] | Iran | Single center | 242 | 106/112 |
| Manes et al[20] | Italy | Multicenter | 1654 | 80/78 |
| Cennamo et al[11] | Italy | Single center | 1078 | 36/110 |
| Swan et al[14] | Australia | Single center | 464 | 39/34 |
The study quality characteristics are discussed in Table 1. The recent RCT by Swan et al[14] was a blinded study. Immediate precut was performed in two studies in patients randomized to precut arm without any previous cannulation attempts[12,18]. In the remaining 5 RCTs, precut randomized patients had 5-12 min of biliary cannulation attempts[10,11,14,19,20], or if there was three accidental pancreatic duct cannulations[11,19]. In the study by Swan et al[14], endoscopists placed a pancreatic stent (Zimmon; Cook Medical, Bloomington, IN; single pigtail, 2-5 cm 5F) before pre-cut sphincterotomy if the PD had been cannulated at least twice. If the PD had not been cannulated during the biliary cannulation attempt(s), a PD stent was not placed. There was no significant difference in the use of PD stents between the 2 randomized groups; 15 of 34 (44%) in the persistent attempts group and 23 of 39 (59%) in the pre-cut sphincterotomy arm. Similarly, there was no statistical difference in the use of PD stents in the successful continued cannulation group vs those in the continued cannulation group who required crossover to pre-cut sphincterotomy; 5 of 12 (41%) vs 10 of 22 (45%) respectively. In rest of the studies pancreatic stent placement was not implemented in both the randomized arms. Six studies[10-12,14,18,20] defined procedure-related complications.
The techniques employed for cannulation and precut were different in the included studies (Table 3). In the persistent attempts group, the wire-guided technique was implemented to achieve deep biliary cannulation in most of the studies[11,12,14,18].
| Ref. | Technique used in persistent attempts group | Timing of early precut | Precut technique | Timing of persistent attempts |
| Tang et al[10] | Non-wire guided sphincterotome | Biliary cannulation failed within 12 min | Needle knife precut starting at orifice | Biliary cannulation failed within 15 min |
| Zhou et al[19] | Non-wire guided and wire guided sphincterotome | Biliary cannulation failed within 10 min or 3 unintended pancreatic duct cannulation | Needle knife precut starting at orifice and fistulotomy | Not available |
| de Weerth et al[12] | Wire guided sphincterotome | Immediate precut for direct bile duct access | Erlangen type sphincterotome on the papillary roof | Biliary cannulation failed within 10 min or 3 unintended pancreatic duct cannulation |
| Khatibian et al[18] | Wire guided sphincterotome | Immediate needle knife fistulotomy for direct CBD access | Needle knife fistulotomy | Biliary cannulation failed within 15 min |
| Manes et al[20] | Non-wire guided and wire guided sphincterotome | Biliary cannulation failed within 10 min | Needle knife fistulotomy | Biliary cannulation failed within 10 min |
| Cennamo et al[11] | Wire guided sphincterotome | Biliary cannulation failed within 5 min or 3 unintended pancreatic duct cannulation | Needle knife precut starting at orifice | Biliary cannulation failed within 20 min post randomization |
| Swan et al[14] | Wire guided sphincterotome | Biliary cannulation failed within 10 min | Needle knife precut starting from superior aspect of orifice | Biliary cannulation failed within 10 min post randomization |
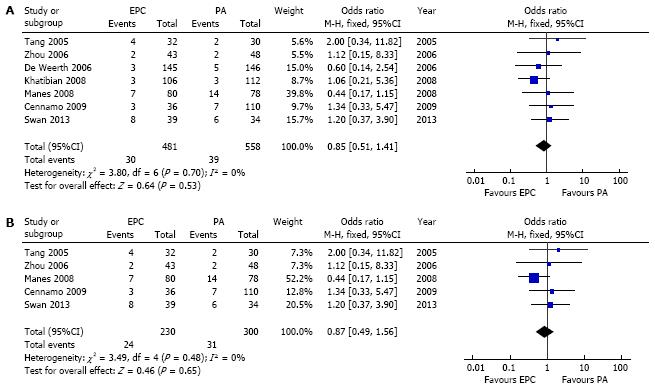
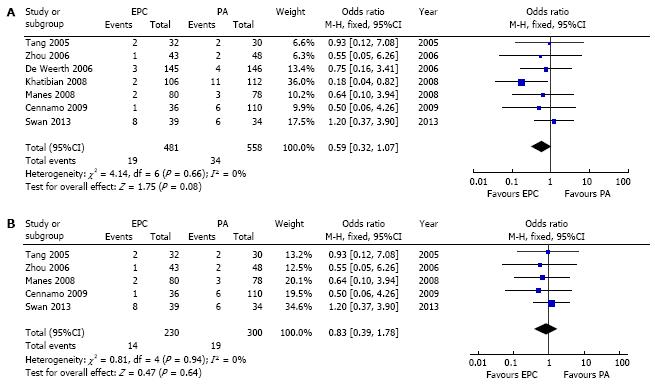
Seven RCTs compared the overall complication rates (Table 1). The baseline characteristics of the studies are presented in detail in Tables 1 and 2. In our meta-analysis (Figure 2A) including 7 studies, the overall complication rates including PEP, bleeding and perforation were 6.2% (30 cases out of 481 patients) in precut group and 6.9% (39 cases out of 558 patients) in persistent attempts group. The pooled analysis didn’t show any statistically significant difference between the two groups with an OR 0.85 (95%CI: 0.51-1.41). As the pooled estimation didn’t showed significant heterogeneity a fixed-effect model was used in this analysis. The risk of PEP was 3.9% (19 cases out of 481 patients) in precut group and 6.1 % (34 cases out of 558 patients) in the persistent attempts group (Figure 3A). Although a trend towards a lower incidence of PEP in the early precut groups was observed, the pooled analysis didn’t show any statistically significant difference between the two groups with an OR 0.59 (95%CI: 0.32-1.07).
The bleeding rate was found to be 1.8% (9 cases out of 481) in precut group and 0.9 % (5 cases out of 558 patients) in the persistent attempts group. The perforation rate was found to be 0.4% (2 cases out of 481) in precut group and 0.18 % (1 case out of 558 patients) in persistent attempts group. An analysis for cholangitis as a complication was not done as rates were not reported in two studies. The numbers were very small to calculate the pooled OR for these complications separately.
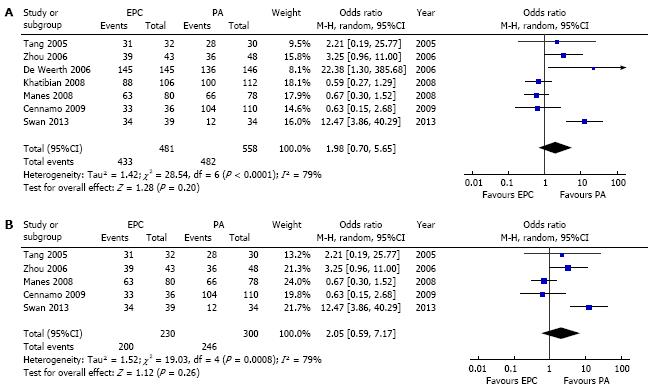
The overall cannulation rate was found to be 90% in pre-cut sphincterotomy group and 86.3% in persistent attempts group. The pooled analysis didn’t show any significant difference between the two groups with an OR 1.98 (95%CI: 0.70-5.65) (Figure 4A). Statistical tests did show the presence of between-study heterogeneity and as such a random effects model was used to account for this heterogeneity.
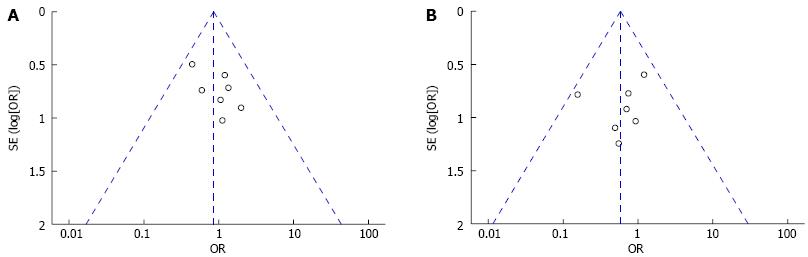
Visual inspection of funnel plots in Figure 5 (for overall complications and post-ERCP pancreatitis) further confirms that publication bias is not a major determinant in this meta-analysis.
In two studies included in our meta-analysis, pre-cut was performed even without attempts at cannulation with the standard approach[12,18]. The other studies had varying periods of cannulation attempts before randomization, reflecting real clinical practice. After excluding the two studies in which direct pre-cut was performed, the results were unchanged (Figure 2B, 3B and 4B).
Despite advances in ERCP, failure of biliary cannulation and PEP remain two major issues where room for improvement exists. In experienced hands, successful biliary cannulation is achieved in over 90% of patients. In 5%-10% of patients, biliary cannulation is difficult for which various methods have been advocated in the literature. Pre-cut sphincterotomy is a valuable technique to achieve biliary access when conventional techniques fail. However, the timing of this procedure is controversial with some literature suggesting that early use of precut sphincterotomy may be preferable to persistent attempts at cannulation with standard approach. In older literature the use of pre-cut technique has been associated with higher rates of PEP, discouraging its use[9,21].
Past studies assessing the association between PEP and precut sphincterotomy have shown seemingly contradictory results. Two prospective studies[22,23] and one meta-analysis[24], suggested a positive association between precut sphincterotomy and risk of PEP, while in 3 prospective studies there was lack of an independent association between pre-cut sphincterotomy and risk of PEP[10,11,20]. There are multiple case series showing similar complication rates for precut and standard sphincterotomy techniques[25,26]. The discrepancy among these studies may be due to factors such as varying experience among endoscopists, varying precut timing during the procedure, different patient populations and use of prophylactic pancreatic stents. Even among the studies included in this meta-analysis, prophylactic pancreatic stents were used only in one study[14]. Also, non-steroidal anti-inflammatory drugs such as indomethacin were not used in any of the studies included in this analysis. Thus, these results do not entirely mirror the current clinical practice of using either pancreatic stents and/or non-steroidal anti-inflammatory medications when performing difficult biliary cannulation during ERCP.
Our meta-analysis, demonstrated that early pre-cut sphincterotomy does not increase the risk of PEP. In fact, although not statistically significant, there was a trend towards a lower risk of PEP with early use of pre-cut sphincterotomy compared to persistent attempts at cannulation. The possible increased risk of PEP with persistent standard cannulation may be because of mechanical damage to the papilla and the pancreatic sphincter[27-33].
In two studies included in our meta-analysis, pre-cut was performed even without attempts at cannulation with the standard approach[12,18]. The other studies had varying periods of cannulation attempts before randomization, reflecting real clinical practice. After excluding the two studies in which direct pre-cut was performed, the results were unchanged. However the question of when to proceed to pre-cut in patients with difficult biliary cannulation has not been studied in RCTs thus far. The most recent RCT included in this meta-analysis suggested that the risk of PEP increased with more than 6-7 attempts at cannulation suggesting the possible threshold to proceed to pre-cut sphincterotomy[14].
In addition to PEP; bleeding[8] and perforation[9] are other complications associated with precut techniques. In this study the bleeding rate was found to be 1.8% in the precut group and 0.9% in the persistent attempts group. The perforation rate was found to be 0.4% in the precut group and 0.2% in persistent attempts group. Although we did not detect any statistically significant difference in bleeding and perforation rates between the two groups, the numbers suggest that a larger patient population may have detected possible subtle differences.
The timing of pre-cut remains controversial. Of the seven studies, Tang et al[10] study did not include late precut in their analysis. The study by Cennamo et al[11] study included early and late pre-cut subgroup and sub-analysis did not showed any difference (P = 0.25). The study by de Weerth et al[12] included both early and late pre-cut, but the authors that there was no difference in the complications. However, no data was available to do sub-analysis. The other two studies by Manes et al[20] and Swan et al[14] included patients in early and late pre-cut, but the authors mentioned that subgroup analysis did not show any statistical difference in the post-ERCP complication rates. The other two studies did not separate into early and late pre-cut group for doing a sub-analysis.
The other issue is the use of pancreatic duct (PD) stents one of the studies included in the meta-analysis. In the study by Swan et al[14], pancreatic duct (PD) stents were used. There was no significant difference in the use of PD stents between the 2 randomized groups, 15 of 34 (44%) in the standard cannulation arm and 23 of 39 (59%) in the NKS arm. Similarly, there was no statistical difference in the use of PD stents in the standard cannulation group vs those in the standard cannulation arm who required crossover to NKS, 5 of 12 (41%) vs 10 of 22 (45%). Multivariate analysis of risk factors for PEP showed clearly that PD stent insertion did not affect the results. Hence it is unlikely that use of PD stents affected our results.
It is important to emphasize that precut sphincterotomy, although did not increase the complication rate should be done only for therapeutic ERCP with failed guidewire cannulation. Certain patients are considered to be high-risk for development of PEP. In a meta-analysis, patients with suspected sphincter of Oddi dysfunction (RR = 4.09, 95%CI: 3.37-4.96, P < 0.001), female gender (RR 2.23, 95%CI: 1.75-2.84, P < 0.001), and those with a previous history of pancreatitis (RR 2.46, 95%CI: 1.93-3.12, P < 0.001) were at high risk; additional procedure-related risk factors for PEP were pancreatic sphincterotomy (RR = 2.71, 95%CI: 2.02-3.63, P < 0.001) and pancreatic injection (RR = 2.2, 95%CI: 1.6-3.01, P < 0.001)[34].
Strengths of this meta-analysis are the inclusion of all RCTs to date. In addition, statistical analysis did not show any significant heterogeneity among the included studies. Furthermore, all included studies reported similar demographic data. However, as all ERCP procedures were done by experienced endoscopists in referral medical centers, the results may not be applicable to community setting practice. Also, the techniques employed for cannulation and precut were different in the included studies. The possible significance of this in altering or modifying the outcomes remains unclear, considering that different techniques may offer different incidence of complications.
To conclude, our study confirms that pre-cut sphincterotomy is a safe and effective strategy when used by experienced biliary endoscopists and does not increase the risk of PEP. However, the exact timing for implementing pre-cut in patients with difficult cannulation remains uncertain and further RCTs employing the time line along with use of pancreatic stents and/or non-steroidal anti-inflammatory medications are required.
The presumed risks and morbidity associated with needle knife sphincterotomy (NKS) in patients with failed routine cannulation, particularly risk of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP) has discouraged use of this technique in patients with difficult biliary access. The authors sought to perform an updated meta-analysis to study the differences in cannulation rates, PEP and overall complication risk between early pre-cut sphincterotomy and persistent attempts at cannulation, taking the new randomized study into consideration.
An earlier meta-analysis demonstrated that early precut sphincterotomy reduces PEP risk but not the overall complication rate or cannulation success. Subsequent to this publication, another RCT has been published.
Based on this meta-analysis, pre-cut sphincterotomy and persistent attempts at cannulation are comparable in terms of overall complication rates.
Although pre-cut is demonstrated as safe, the exact timing for implementing pre-cut in patients with difficult cannulation remains uncertain and further studies should employ the time line along with use of pancreatic stents and/or non-steroidal anti-inflammatory medications to determine the optimal approach for biliary cannulation.
ERCP has been widely used for treatment of a variety of biliary disorders and cannulation of the bile duct remains one of the most important steps for successful therapeutic endoscopy. Precut sphincterotomy, also referred to as NKS, has been advocated in situations where routine biliary cannulation has been unsuccessful.
This paper confirms that precut sphincterotomy is not more harmful that persistent attempts of cannulation of the papilla in terms of pancreatitis and other complications. It is well done and the inclusion criteria are correct and well defined.
P- Reviewers: Contini S, Desilets DJ, Kochhar R S- Editor: Song XX L- Editor: A E- Editor: Zhang DN
| 1. | Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc. 2005;61:112-125. |
| 2. | Huibregste KKM. Endoscopic retrograde cholangiopancreatography, endoscopic sphincterotomy and endoscopic biliary and pancreatic drainage. Textbook of Gastroenterology. Philadelphia: Lippincott Williams & Wilkins 1995; 2590-2617. |
| 3. | Bailey AA, Bourke MJ, Williams SJ, Walsh PR, Murray MA, Lee EY, Kwan V, Lynch PM. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008;40:296-301. |
| 4. | Shakoor T, Geenen JE. Pre-cut papillotomy. Gastrointest Endosc. 1992;38:623-627. |
| 5. | Baillie J. Needle-knife papillotomy revisited. Gastrointest Endosc. 1997;46:282-284. |
| 6. | Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna GS. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425-434. |
| 7. | Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson ML, Williamson PR. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy. 2007;39:793-801. |
| 8. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. |
| 9. | Bruins Slot W, Schoeman MN, Disario JA, Wolters F, Tytgat GN, Huibregtse K. Needle-knife sphincterotomy as a precut procedure: a retrospective evaluation of efficacy and complications. Endoscopy. 1996;28:334-339. |
| 10. | Tang SJ, Haber GB, Kortan P, Zanati S, Cirocco M, Ennis M, Elfant A, Scheider D, Ter H, Dorais J. Precut papillotomy versus persistence in difficult biliary cannulation: a prospective randomized trial. Endoscopy. 2005;37:58-65. |
| 11. | Cennamo V, Fuccio L, Repici A, Fabbri C, Grilli D, Conio M, D’Imperio N, Bazzoli F. Timing of precut procedure does not influence success rate and complications of ERCP procedure: a prospective randomized comparative study. Gastrointest Endosc. 2009;69:473-479. |
| 12. | de Weerth A, Seitz U, Zhong Y, Groth S, Omar S, Papageorgiou C, Bohnacker S, Seewald S, Seifert H, Binmoeller KF. Primary precutting versus conventional over-the-wire sphincterotomy for bile duct access: a prospective randomized study. Endoscopy. 2006;38:1235-1240. |
| 13. | Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, Fabbri C, Bazzoli F. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk? Meta-analysis of randomized controlled trials. Endoscopy. 2010;42:381-388. |
| 14. | Swan MP, Alexander S, Moss A, Williams SJ, Ruppin D, Hope R, Bourke MJ. Needle knife sphincterotomy does not increase the risk of pancreatitis in patients with difficult biliary cannulation. Clin Gastroenterol Hepatol. 2013;11:430-436.e1. |
| 15. | Higgins JPT, Green S, editors . Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. Oxford: The Cochrane Collaboration 2009; . |
| 16. | DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188. |
| 17. | Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-634. |
| 18. | Khatibian M, Sotoudehmanesh R, Ali-Asgari A, Movahedi Z, Kolahdoozan S. Needle-knife fistulotomy versus standard method for cannulation of common bile duct: a randomized controlled trial. Arch Iran Med. 2008;11:16-20. |
| 19. | Zhou PH, Yao LQ, Xu MD, Zhong YS, Gao WD, He GJ, Zhang YQ, Chen WF, Qin XY. Application of needle-knife in difficult biliary cannulation for endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int. 2006;5:590-594. |
| 20. | Manes G, Di Giorgio P, Repici A, Macarri G, Ardizzone S, Porro GB. An analysis of the factors associated with the development of complications in patients undergoing precut sphincterotomy: a prospective, controlled, randomized, multicenter study. Am J Gastroenterol. 2009;104:2412-2417. |
| 21. | Huibregtse K, Katon RM, Tytgat GN. Precut papillotomy via fine-needle knife papillotome: a safe and effective technique. Gastrointest Endosc. 1986;32:403-405. |
| 22. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. |
| 23. | Wang P, Li ZS, Liu F, Ren X, Lu NH, Fan ZN, Huang Q, Zhang X, He LP, Sun WS. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009;104:31-40. |
| 24. | Masci E, Mariani A, Curioni S, Testoni PA. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a meta-analysis. Endoscopy. 2003;35:830-834. |
| 25. | Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80-88. |
| 26. | Goff JS. Long-term experience with the transpancreatic sphincter pre-cut approach to biliary sphincterotomy. Gastrointest Endosc. 1999;50:642-645. |
| 27. | Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, Fabbri C, Bazzoli F. Can a wire-guided cannulation technique increase bile duct cannulation rate and prevent post-ERCP pancreatitis?: A meta-analysis of randomized controlled trials. Am J Gastroenterol. 2009;104:2343-2350. |
| 28. | Gottlieb K, Sherman S. ERCP and biliary endoscopic sphincterotomy-induced pancreatitis. Gastrointest Endosc Clin N Am. 1998;8:87-114. |
| 29. | Chen YK, Foliente RL, Santoro MJ, Walter MH, Collen MJ. Endoscopic sphincterotomy-induced pancreatitis: increased risk associated with nondilated bile ducts and sphincter of Oddi dysfunction. Am J Gastroenterol. 1994;89:327-333. |
| 30. | Sherman S. ERCP and endoscopic sphincterotomy-induced pancreatitis. Am J Gastroenterol. 1994;89:303-305. |
| 31. | Kasmin FE, Cohen D, Batra S, Cohen SA, Siegel JH. Needle-knife sphincterotomy in a tertiary referral center: efficacy and complications. Gastrointest Endosc. 1996;44:48-53. |
| 32. | Vandervoort J, Soetikno RM, Tham TC, Wong RC, Ferrari AP, Montes H, Roston AD, Slivka A, Lichtenstein DR, Ruymann FW. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56:652-656. |
| 33. | Freeman ML, Guda NM. Prevention of post-ERCP pancreatitis: a comprehensive review. Gastrointest Endosc. 2004;59:845-864. |
| 34. | Madácsy L, Kurucsai G, Fejes R, Székely A, Székely I. Prophylactic pancreas stenting followed by needle-knife fistulotomy in patients with sphincter of Oddi dysfunction and difficult cannulation: new method to prevent post-ERCP pancreatitis. Dig Endosc. 2009;21:8-13. |