Published online Dec 16, 2014. doi: 10.4253/wjge.v6.i12.606
Revised: September 11, 2014
Accepted: October 31, 2014
Published online: December 16, 2014
Processing time: 217 Days and 6 Hours
AIM: To compare (using the Ottawa Bowel Preparation Scale) the efficacy of split-dose vs morning administration of polyethylene glycol solution for colon cleansing in patients undergoing colonoscopy, and to assess the optimal preparation-to-colonoscopy interval.
METHODS: Single-centre, prospective, randomized, investigator-blind stud in an academic tertiary-care centre. Two hundred patients requiring elective colonoscopy were assigned to receive one of the two preparation regimens (split vs morning) prior to colonoscopy. Main outcome measurements were bowel preparation quality and patient tolerability.
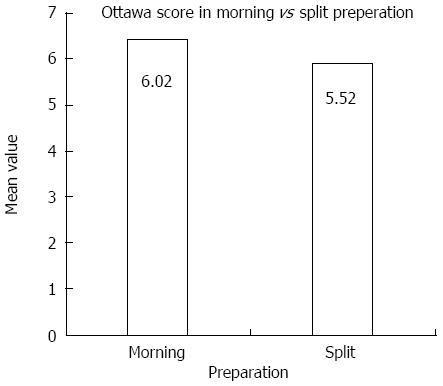
RESULTS: Split-dose regimen resulted in better bowel preparation compared to morning regimen [Ottawa score mean 5.52 (SD 1.23) vs 6.02 (1.34); P = 0.017]. On subgroup analysis, for afternoon procedures, both the preparations were equally effective (P = 0.756). There was no difference in tolerability and compliance between the two regimens.
CONCLUSION: Overall, previous evening - same morning split-dosing regimen results in better bowel cleansing for colonoscopy compared to morning preparation. For afternoon procedures, both schedules are equally effective; morning preparation may be more convenient to the patient.
Core tip: Split bowel reparation compared to single dose morning preparation resulted in a better bowel cleansing using the Ottawa Bowel Preparation Scale. The average score (± SD) using the Ottawa Scale was 6.02 ± 1.34 when morning preparation was given and 5.52 ± 1.23 when split preparation was given (P = 0.017). However, there was no statistical difference in the mean Ottawa score when the procedures were done in the afternoon with either the morning or the split preparation (6.09 vs 5.94, P = 0.756). Hence, AM only dosing is as effective as split dosing for patients scheduled for a colonoscopy in the afternoon.
-
Citation: Shah H, Desai D, Samant H, Davavala S, Joshi A, Gupta T, Abraham P. Comparison of split-dosing
vs non-split (morning) dosing regimen for assessment of quality of bowel preparation for colonoscopy. World J Gastrointest Endosc 2014; 6(12): 606-611 - URL: https://www.wjgnet.com/1948-5190/full/v6/i12/606.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i12.606
Successful completion of colonoscopy depends to a large extent on the quality of bowel preparation[1,2]. Poorly visualized mucosa leads to missed diagnoses and increases colonoscopic risk[3-5]. Even a small amount of residual stool can obscure small lesions such as angiodysplasia[5].
Bowel preparation has evolved from previous evening regimen to split dose regimen. Traditional colon preparation involves the unpleasant task of drinking a large volume of a cleansing solution the evening before the procedure. One way to increase tolerability and patient adherence is to split the dose so that the patient takes half the solution the evening before colonoscopy and the other half in the morning, usually about 4 to 5 h before the scheduled time of the procedure[6,7].
Prior studies have demonstrated that split dosing not only to improves patient acceptability, but also cleans the colon better[8]. Of 13 prospective, randomized studies done previously, 12 showed superior cleansing when whole or part of the bowel preparation was given in the morning of the scheduled colonoscopy[9-21].
However colonoscopies are often scheduled in the afternoon, and split dosing may not leave a clean colon by afternoon. A recent study by Matro et al[22] showing equal cleansing efficacy and tolerability of a morning dosing and split preparation when procedures are slated for the afternoon; this study did not include procedures scheduled in the morning.
The quality of bowel cleansing is generally assessed by the quantity of solid or liquid stool in the lumen. An adequate colonic examination is one that allows confidence that mass lesions other than small (< 5 mm) polyps not to be obscured by the preparation[23].
The primary aim of this study was to evaluate the efficacy of colon cleansing in patients undergoing colonoscopy, comparing the modality of administration, i.e., split (previous eveningsame morning) vs morning-only dose, using the Ottawa Bowel Preparation Scale (Ottawa Scale)[24]. We also assessed how the time interval between the last dose of bowel preparation and the start of colonoscopy, i.e., the preparation-to-colonoscopy (PC) interval, affects the quality of bowel preparation. The secondary aim was to study patient compliance and tolerability to the two preparation regimens and the willingness to repeat the bowel preparation in future if required.
Patients seen in the outpatient clinic of our department as well as hospitalized patients who required elective colonoscopy were screened for enrolment in the study. Exclusion criteria included patients under 18 years of age, presence of severe renal impairment (creatinine clearance < 30 mL/min) or patients on haemodialysis, pregnant or lactating women, severe congestive heart failure (NYHA III or IV), history of bowel obstruction or resection, known allergies to polyethylene glycol (PEG), and refusal of consent for the study. Patients who were inconvenienced by the timing of bowel preparation were also excluded. Approval from the hospital’s ethics committee was obtained. Written, informed consent was obtained from each patient.
Patients were provided written instructions in a sealed opaque envelope, for either of the bowel preparations, by their gastroenterologists who were blinded to the content of the envelope. The envelopes were randomized in blocks of five (using a computer-generated random numbers table) by an independent study assistant who kept the randomization key under lock until the inclusion of the last patient. Investigator and colonoscopist were blinded to group allocation.
All patients were instructed to adhere to a liquid diet the day before their colonoscopy, and only clear liquids orally after midnight until the procedure time. The morning preparation group was instructed to consume one packet of PEG dissolved in 2 L of water on the morning of the colonoscopy (between 5 am and 7 am). The split-dose group was instructed to dissolve one packet of PEG in 2 L of water and consume one-half of this the evening before the day of the colonoscopy (between 6 pm and 7 pm) and the other half on the morning of the procedure (between 6 am and 7 am).
Patients were advised not to discuss their bowel preparation with their endoscopist but to contact the study assistant or the receiving nurse if questions arose. A mechanism was established to address patient concerns and issues of safety, without unblinding the endoscopist. They were given a questionnaire to be completed once their bowel preparation was finished and before coming to the hospital for the colonoscopy. The questionnaire included details about the tolerability of the regimen, compliance with the instructions for bowel preparation and diet, the amount of preparation taken, and completion time of the last PEG dose. Drinking at least 75% of the preparation volume was regarded as proper amount of PEG taken for bowel preparation. The following data were also collected: age, sex, indication for the procedure, history of abdominal or gynaecologic surgery, history of constipation, and other co-morbidities including diabetes, hypertension, and renal failure.
Colonoscopies were performed with the patients under conscious sedation by either a gastroenterology fellow or a consultant gastroenterologist. All colonoscopies were done between 11 am and 4 pm (morning sessions between 11 am and 1 pm, afternoon sessions between 1 pm and 4 pm). Time of completion of the last PEG dose and colonoscopy starting time were recorded, and the PC interval was calculated. A minimum of 4 h was kept between the completion of the last PEG dose and the start of colonoscopy for all patients.
A combination of intravenous fentanyl 50 mcg and midazolam 2 mg was used for sedation in patients in whom there was no contraindication; half the dose was used in patients over the age of 60 years. Additional sedation was used if required and permissible. Pulse, blood pressure, and oxygen saturation were measured in all patients before, during and after the procedure.
Bowel cleansing was evaluated by using the Ottawa Bowel Preparation Scale[24]. This scale assesses cleanliness and fluid volume separately. Cleanliness was assessed separately for the right colon (caecum, ascending), mid colon (transverse, descending), and the rectosigmoid on a 5-point scale (no liquid = 0, minimal liquid, no suctioning required = 1, suction required to see mucosa = 2, wash and suction = 3, solid stool, not washable = 4). Fluid quantity was rated from 0 to 2 for the entire colon (minimal = 0, moderate = 1, large = 2). The Ottawa Scale scores range from 0 (perfect) to 14 (completely unprepared colon). An excellent preparation would score 0 to 2; a good preparation, 3 to 5; and scores higher than 5 would indicate progressively worsening bowel preparation. A completely unprepared colon would score 11 to 14, depending on the amount of colonic fluid. The quality of preparation was assessed at the time of insertion of the colonoscope before any cleansing maneuvers. Each patient’s colonoscopy was recorded on a DVD; the bowel-preparation quality was rated by a single investigator who was blinded to the type of preparation, and the results recorded on a standardized form.
On the basis of data from previous studies[20-22], a sample size of 200 patients was estimated to give an 80% power at a two-sided alpha of 0.05% to detect a 15% difference in the Ottawa bowel preparation quality scale. Bowel preparation scores measured by the Ottawa Scale were compared between the morning and split-dose groups using the Mann-Whitney U test. Pearson χ2 test and continuity correction was used for comparing proportions in the two groups. A value of P < 0.05 was considered statistically significant.
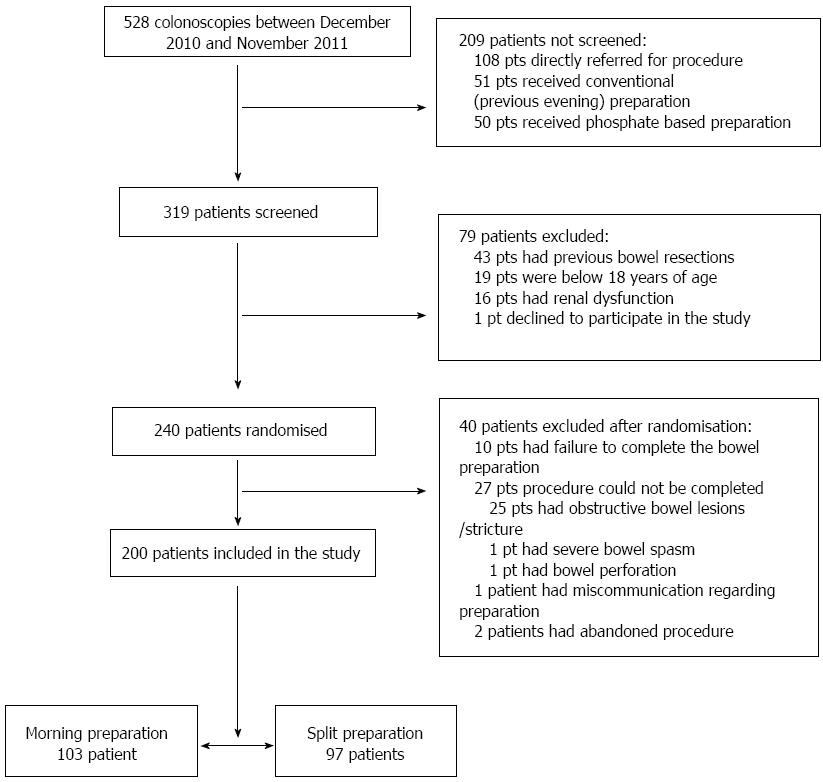
In this prospective, randomized, investigator-blinded study, we enrolled 200 patients (mean age 51.8 years, SD 15.9, range 18-88; 121 men) between December 2010 and November 2011. A total of 528 colonoscopies were done during this period. Of these, 319 patients were screened for inclusion in the study. Screening was not possible in the remaining 209 patients-108 patients were directly referred for colonoscopy without being randomized, 51 were given the conventional previous-evening bowel preparation, and 50 took another bowel-preparation solution as advised by their referring physician. Of the 319 patients screened, 240 were randomized; 79 patients were excluded as they did not meet the inclusion criteria: previous bowel surgeries (n = 43), below age 18 years (19), renal dysfunction or on haemodialysis (16), and refusal of consent (1).
Of the 240 patients randomized, 40 were excluded: failure to complete bowel preparation as advised (n = 10; 6 in morning and 4 in split dose regimen); miscommunication regarding bowel preparation (1); inability to complete colonoscopy due to bowel lesion/stricture (25), spasm (1) and perforation (1). Two patients had extremely poor bowel preparation (both had taken morning preparation) and hence colonoscopy was abandoned and they were given a repeat bowel preparation.
Cecal intubation rate was 99.5% in our study. Only patients who had a complete colon examination from anal verge up to the cecum were included in the analysis. Of 200 such patients (109 outpatients, 91 inpatients), 103 received morning preparation and 97 received the split preparation (Figure 1). Total 135 patients underwent endoscopies in the morning (70 from morning preparation and 65 from split preparation). Both groups were comparable in terms of demographic data (62 males in morning preparation and 59 males in split preparation, median age = 53 years in both groups) and indications for colonoscopy.
The split preparation had better bowel efficacy compared to the morning preparation. Overall, 88 (44%) patients had Ottawa score 5 or less indicating good bowel preparation. 93 (46.5%) had average bowel preparation with score 6 and 7, and 19 (9.5%) patients had poor bowel preparation with score above 8. The mean Ottawa Scale score (SD) was 6.02 (1.34) with the morning preparation and 5.52 (1.23) with split preparation (P = 0.017) (Figure 2). With morning colonoscopy (11 am-1 pm), the mean Ottawa score was 5.99 and 5.31 (P = 0.007) for the morning and split preparations, respectively. With afternoon colonoscopy, the corresponding scores were 6.09 and 5.94 (P = 0.756), respectively.
A gap of at least 4 h was kept for every patient between the last preparation intake and the time of colonoscopy. Afternoon colonoscopies with PC interval > 6 h had poor bowel preparation (Ottawa score 5.66) compared to morning colonoscopies with PC interval between 4 and 6 h (6.02; P = 0.075).
Nausea was complained of by 29.1% of patients with the morning preparation and 19.6% with split preparation (P = 0.161), abdominal discomfort by 9.7% and 13.4%, (P = 0.551), vomiting by 10.7% and 11.3% (P = 1.0), bloating by 12.6% and 9.3% (P = 0.597), and headache, dizziness and uneasiness by 4.9% and 4.1%, respectively (P = 1.0). Sleep was disturbed in 8 (7.8%) patients receiving the morning preparation and in 14 (14.4%) patients receiving the split preparation (P = 0.201). No patient experienced inconvenience while travelling.
Traditionally, the entire bowel-cleansing preparation solution is given in the evening prior to colonoscopy. In order to avoid sleep disturbance, it has to be given early in the evening. Alternatively, the preparation solution can be taken in a split dose, 8-12 h apart. Studies have shown that ingesting at least a part of the purgative on the day of colonoscopy and coordinating the final dose of purgative with the start time of colonoscopy is more likely to result in adequate colon cleansing[11,25]. Generally, this is accomplished by splitting the purgative between the evening prior and the morning of colonoscopy.
Previous studies have shown that the split preparation is better than the conventional previous-evening preparation in terms of bowel preparation quality and patient compliance[14,17,18,25,26]. The split-dose option is also endorsed by the American College of Gastroenterology and is considered an optimal choice for colonoscopy[27]. However, there have been few studies comparing split preparation to same-day morning preparation, which may be more convenient to patients as it does not interfere with common office schedules. We have shown earlier that same-morning preparation was better than previous-evening preparation[20]. In the present study we compared split dose with same-morning preparation.
In this study, split dosing resulted in better bowel cleansing than the same-morning preparation, both overall and when colonoscopy was performed in the morning. However, there was no difference in the mean Ottawa score when colonoscopies were done in the afternoon. For patients scheduled for a colonoscopy in the afternoon, either of the preparation is comparable. The advantage of the morning preparation is it interferes less with the patient’s routines and work schedules; patients often complain about trouble sleeping after taking the evening preparation.
A PC interval of 4 to 6 h resulted in better bowel preparation compared to one greater than 6 h. When patients were scheduled for the afternoon list, an interval between preparation and procedure greater than 6 h resulted in inferior bowel preparation, although this was not statistically significant. A long interval results in thick secretions emptying out of the small intestine and obscuring the caecum and ascending colon at the time of colonoscopy.
Seo et al[28] evaluated 366 consecutive outpatients undergoing colonoscopy using the split preparation; colonoscopies with PC interval 3 to 5 h had the best bowel preparation quality. Matro et al[22] compared the efficacy and tolerability of morning-only PEG to split-dose PEG for afternoon colonoscopy, and found both equivalent with respect to cleansing efficacy and polyp detection. Morning-only preparation was associated with lower incidence of abdominal pain, superior sleep quality, and less interference with work day prior to colonoscopy. While conventionally colonoscopies are performed in the morning, linking the administration of the preparation to the time of the procedure for both morning-only and split dosing may make late morning and afternoon colonoscopy equally attractive to patients.
In our study, there was no difference in tolerability between the morning and split regimens. Both regimens were equally well tolerated, with most patients willing to repeat the preparation in the future if the need arises.
In conclusion, split evening-morning dosing is superior to morning-only dosing for colon cleansing prior to colonoscopy if the procedure is slated in the morning; for afternoon colonoscopy, morning-only preparation is as effective. Optimal colon cleansing requires purgative administration close to the time of colonoscopy. For patients scheduled for colonoscopy in afternoon, it may be convenient to take the preparation in morning so that PC interval is minimized.
There is no standard recommendation regarding the timing of colonoscopy preparation. Different regimens are mentioned in literature. Traditionally, the entire preparatory solution is given in the evening, a day prior to the procedure. Alternatively, the preparatory solution can be taken in a split dose, 8-12 h apart. Studies have shown that ingesting at least a part of the purgative on the day of colonoscopy and coordinating the final dose of purgative with the start time of colonoscopy is more likely to result in adequate colon cleansing. Generally, this is accomplished by splitting the purgative between the evening prior and the morning of colonoscopy. Previous studies have proved that the split preparation is better than the conventional previous evening preparation in terms of bowel preparation quality and patient compliance. The split dose option is also endorsed by the American College of Gastroenterology and is considered an optimal choice for colonoscopy. But there have been very few studies comparing split preparation to same day morning preparation, which is more relevant to current clinical practice. What people looked at was can people administer the colon preparation the same day and get equal results? Is there a better way for bowel preparation without inconveniencing the patient? This rationale for the study was to compare the quality of bowel preparation using the same morning vs split regimens and also assess the importance of preparation-to-colonoscopy (PC) interval. The primary endpoint was whole colon preparation adequacy.
Though there are several factors implicated in successful completion of a colonoscopy, quality of bowel preparation and timing of colonoscopy are considered two modifiable factors to improve successful completion. Improving the quality of colonoscopy is a major initiative of many digestive disease organizations. Various studies are ongoing to assess how the time interval between the last dose of bowel preparation and the start of colonoscopy, i.e., the PC interval, affects the quality of bowel preparation and to determine the optimal PC interval for satisfactory bowel preparation.
Previous studies have proved that the split preparation is better than the conventional previous evening preparation in terms of bowel preparation quality and patient compliance. However, in this study there was no difference in the quality of bowel preparation for patients undergoing colonoscopy in afternoon with either the split or the same day morning preparation. Hence, same day bowel preparation should become a new standard for afternoon colonoscopy.
This study expands the options for patients by demonstrating that ingestion of polyethylene glycol preparation entirely on the day of colonoscopy is as good as a split dose schedule for an afternoon procedure.
Split preparation: Where the patient takes half the laxative prescription the evening before colonoscopy and the other half in the morning of the scheduled procedure.
The article entitled “Comparison of split-dosing vs non-split (morning) dosing regimen for assessment of quality of bowel preparation for colonoscopy” by Shah et al describes a study comparing the effect of morning-only and split bowel preparation of PEG solutions on bowel cleansing, for both morning and afternoon colonoscopies. Overall this study is timely and interesting to the readership.
P- Reviewer: Damin DC, Gioux S, Souza JLS, Wu B S- Editor: Song XX L- Editor: A E- Editor: Zhang DN
| 1. | Cappell MS, Friedel D. The role of sigmoidoscopy and colonoscopy in the diagnosis and management of lower gastrointestinal disorders: endoscopic findings, therapy, and complications. Med Clin North Am. 2002;86:1253-1288. |
| 2. | Taylor SA, Halligan S, Bartram CI. CT colonography: methods, pathology and pitfalls. Clin Radiol. 2003;58:179-190. |
| 3. | Toledo TK, DiPalma JA. Review article: colon cleansing preparation for gastrointestinal procedures. Aliment Pharmacol Ther. 2001;15:605-611. |
| 4. | Nelson DB, Barkun AN, Block KP, Burdick JS, Ginsberg GG, Greenwald DA, Kelsey PB, Nakao NL, Slivka A, Smith P. Technology Status Evaluation report. Colonoscopy preparations. May 2001. Gastrointest Endosc. 2001;54:829-832. |
| 5. | Neidich RL, Zuckerman GR. Patient preparation. Colonoscopy: Principles and Techniques. New York: Igaku-Shoin 1995; 53-82. |
| 6. | Tan JJ, Tjandra JJ. Which is the optimal bowel preparation for colonoscopy - a meta-analysis. Colorectal Dis. 2006;8:247-258. |
| 7. | Belsey J, Epstein O, Heresbach D. Systematic review: oral bowel preparation for colonoscopy. Aliment Pharmacol Ther. 2007;25:373-384. |
| 8. | Rex DK, Imperiale TF, Latinovich DR, Bratcher LL. Impact of bowel preparation on efficiency and cost of colonoscopy. Am J Gastroenterol. 2002;97:1696-1700. |
| 9. | Church JM. Effectiveness of polyethylene glycol antegrade gut lavage bowel preparation for colonoscopy--timing is the key! Dis Colon Rectum. 1998;41:1223-1225. |
| 10. | Frommer D. Cleansing ability and tolerance of three bowel preparations for colonoscopy. Dis Colon Rectum. 1997;40:100-104. |
| 11. | Parra-Blanco A, Nicolas-Perez D, Gimeno-Garcia A, Grosso B, Jimenez A, Ortega J, Quintero E. The timing of bowel preparation before colonoscopy determines the quality of cleansing, and is a significant factor contributing to the detection of flat lesions: a randomized study. World J Gastroenterol. 2006;12:6161-6166. |
| 12. | Wruble L, Demicco M, Medoff J, Safdi A, Bernstein J, Dalke D, Rose M, Karlstadt RG, Ettinger N, Zhang B. Residue-free sodium phosphate tablets (OsmoPrep) versus Visicol for colon cleansing: a randomized, investigator-blinded trial. Gastrointest Endosc. 2007;65:660-670. |
| 13. | Di Palma JA, Rodriguez R, McGowan J, Cleveland Mv. A randomized clinical study evaluating the safety and efficacy of a new, reduced-volume, oral sulfate colon-cleansing preparation for colonoscopy. Am J Gastroenterol. 2009;104:2275-2284. |
| 14. | Aoun E, Abdul-Baki H, Azar C, Mourad F, Barada K, Berro Z, Tarchichi M, Sharara AI. A randomized single-blind trial of split-dose PEG-electrolyte solution without dietary restriction compared with whole dose PEG-electrolyte solution with dietary restriction for colonoscopy preparation. Gastrointest Endosc. 2005;62:213-218. |
| 15. | Chiu HM, Lin JT, Wang HP, Lee YC, Wu MS. The impact of colon preparation timing on colonoscopic detection of colorectal neoplasms--a prospective endoscopist-blinded randomized trial. Am J Gastroenterol. 2006;101:2719-2725. |
| 16. | El Sayed AM, Kanafani ZA, Mourad FH, Soweid AM, Barada KA, Adorian CS, Nasreddine WA, Sharara AI. A randomized single-blind trial of whole versus split-dose polyethylene glycol-electrolyte solution for colonoscopy preparation. Gastrointest Endosc. 2003;58:36-40. |
| 17. | Park JS, Sohn CI, Hwang SJ, Choi HS, Park JH, Kim HJ, Park DI, Cho YK, Jeon WK, Kim BI. Quality and effect of single dose versus split dose of polyethylene glycol bowel preparation for early-morning colonoscopy. Endoscopy. 2007;39:616-619. |
| 18. | Abdul-Baki H, Hashash JG, Elhajj II, Azar C, El Zahabi L, Mourad FH, Barada KA, Sharara AI. A randomized, controlled, double-blind trial of the adjunct use of tegaserod in whole-dose or split-dose polyethylene glycol electrolyte solution for colonoscopy preparation. Gastrointest Endosc. 2008;68:294-300; quiz 334, 336. |
| 19. | Rostom A, Jolicoeur E, Dubé C, Grégoire S, Patel D, Saloojee N, Lowe C. A randomized prospective trial comparing different regimens of oral sodium phosphate and polyethylene glycol-based lavage solution in the preparation of patients for colonoscopy. Gastrointest Endosc. 2006;64:544-552. |
| 20. | Gupta T, Mandot A, Desai D, Abraham P, Joshi A, Shah S. Comparison of two schedules (previous evening versus same morning) of bowel preparation for colonoscopy. Endoscopy. 2007;39:706-709. |
| 21. | Berkelhammer C, Ekambaram A, Silva RG. Low-volume oral colonoscopy bowel preparation: sodium phosphate and magnesium citrate. Gastrointest Endosc. 2002;56:89-94. |
| 22. | Matro R, Shnitser A, Spodik M, Daskalakis C, Katz L, Murtha A, Kastenberg D. Efficacy of morning-only compared with split-dose polyethylene glycol electrolyte solution for afternoon colonoscopy: a randomized controlled single-blind study. Am J Gastroenterol. 2010;105:1954-1961. |
| 23. | Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, Kirk LM, Litlin S, Lieberman DA, Waye JD. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2002;97:1296-1308. |
| 24. | Rostom A, Jolicoeur E. Validation of a new scale for the assessment of bowel preparation quality. Gastrointest Endosc. 2004;59:482-486. |
| 25. | Marmo R, Rotondano G, Riccio G, Marone A, Bianco MA, Stroppa I, Caruso A, Pandolfo N, Sansone S, Gregorio E. Effective bowel cleansing before colonoscopy: a randomized study of split-dosage versus non-split dosage regimens of high-volume versus low-volume polyethylene glycol solutions. Gastrointest Endosc. 2010;72:313-320. |
| 26. | Park SS, Sinn DH, Kim YH, Lim YJ, Sun Y, Lee JH, Kim JY, Chang DK, Son HJ, Rhee PL. Efficacy and tolerability of split-dose magnesium citrate: low-volume (2 liters) polyethylene glycol vs. single- or split-dose polyethylene glycol bowel preparation for morning colonoscopy. Am J Gastroenterol. 2010;105:1319-1326. |
| 27. | Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol. 2009;104:739-750. |
| 28. | Seo EH, Kim TO, Park MJ, Joo HR, Heo NY, Park J, Park SH, Yang SY, Moon YS. Optimal preparation-to-colonoscopy interval in split-dose PEG bowel preparation determines satisfactory bowel preparation quality: an observational prospective study. Gastrointest Endosc. 2012;75:583-590. |