Published online Sep 16, 2013. doi: 10.4253/wjge.v5.i9.455
Revised: August 15, 2013
Accepted: August 20, 2013
Published online: September 16, 2013
Processing time: 61 Days and 1.8 Hours
An 85-year-old female, with hereditary nonpolyposis colorectal cancer syndrome, underwent a colonoscopy and endoscopic mucosal resection (EMR) of a 25-mm proximal ascending colon polyp (Paris classification 0-Is). Post-procedure, the patient developed abdominal pain in the right iliac fossa which settled 1 h later. An urgent computed tomography (CT) scan of her abdomen was organised which happened 6 h post onset of abdominal pain. She had radiological evidence of perforation on the CT scan but clinically remained well and was managed conservatively. The exact aetiology of this patient’s symptoms is not known. We suspect the radiological findings are probably due to a combination of injectate within the colonic wall and leakage of insufflated air or CO2 following transmural passage of the EMR needle. As EMR is becoming an increasingly effective treatment modality in the management of large sessile polyps, clinicians need to be aware of potential complications of treatment. It is also important to recognise that radiological features of perforation can be seen post EMR in the absence of an EMR associated perforation.
Core tip: This report highlights the importance of correlating clinical findings with radiological ones in a patient who underwent endoscopic mucosal resection of a large ascending polyp. The computed tomography scan in this case reveals a colonic perforation but the patient was symptom free and was managed conservatively without needing surgery. Colonoscopists who undertake endoscopic mucosal resection (EMR) need to be aware that radiological features of perforation can be seen post EMR in the absence of an EMR associated perforation.
- Citation: Heerasing N, Dowling D, Alexander S. Abdominal pain post endoscopic mucosal resection: Treat the patient not the CT scan. World J Gastrointest Endosc 2013; 5(9): 455-456
- URL: https://www.wjgnet.com/1948-5190/full/v5/i9/455.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i9.455
Endoscopic mucosal resection in a tertiary setting is a safe, efficient and effective minimally invasive outpatient therapy for large sessile polyps or laterally spreading tumors of the colon[1]. In this case report, we describe a patient who, having developed abdominal pain post resection of a large colonic polyp, was managed conservatively.
An 85-year-old female, with hereditary nonpolyposis colorectal cancer syndrome, underwent a colonoscopy and endoscopic mucosal resection (EMR) of a 25-mm proximal ascending colon polyp (Paris classification 0-Is). Piecemeal resection after chromo-saline injection was undertaken.
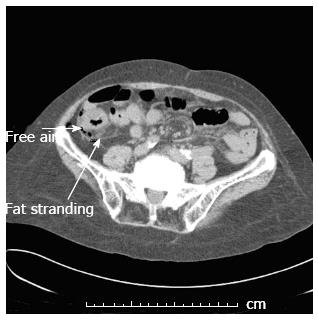
Post procedure, the patient experienced abdominal pain in the right iliac fossa and was monitored. An urgent computed tomography (CT) scan (Figure 1) of the abdomen was ordered but was delayed due to equipment malfunction. Whilst awaiting her scan, the patient’s pain resolved (1 h post resection). Approximately 6 h post EMR, CT scan showed inflammatory stranding at the site of EMR and extra-luminal gas consistent with a colonic perforation. Despite these findings, the patient remained pain free and was discharged the following day.
Non-specific and usually self-resolving abdominal pain is reported to occur in around 2% of EMR procedures[1]. EMR in the colon has become a commonly used technique and a viable alternative to invasive surgery for the treatment of large or complex pre-malignant lesions[2]. The rate of perforation during EMR is estimated to be around 1.3%[3]. In our patient, the radiological findings are probably due to a combination of injectate within the colonic wall and leakage of insufflated air or CO2 following transmural passage of the EMR needle. To our knowledge, this has not been previously reported in the English literature. Our patient has remained well and she had a repeat colonoscopy six months later which showed no recurrent polyp.
Colonoscopists who undertake EMR need to be aware that radiological features of perforation can be seen post EMR in the absence of an EMR associated perforation. As usual, it is essential to treat the patient and not the CT scan findings.
P- Reviewer Day LW S- Editor Wen LL L- Editor A E- Editor Wu HL
| 1. | Bourke MJ. Endoscopic mucosal resection in the colon: a practical guide. Tech Gastrointest Endosc. 2011;13:35-49. [RCA] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Swan MP, Bourke MJ, Alexander S, Moss A, Williams SJ. Large refractory colonic polyps: is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc. 2009;70:1128-1136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 147] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 3. | Moss A, Bourke MJ, Williams SJ, Hourigan LF, Brown G, Tam W, Singh R, Zanati S, Chen RY, Byth K. Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology. 2011;140:1909-1918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 439] [Article Influence: 31.4] [Reference Citation Analysis (0)] |