Published online Sep 16, 2012. doi: 10.4253/wjge.v4.i9.434
Revised: May 27, 2012
Accepted: September 12, 2012
Published online: September 16, 2012
The clinical and endoscopic features of amyloid light-chain (AL) amyloidosis are diverse and mimic various other diseases. Endoscopically, few reports on submucosal hematomas of the gastrointestinal (GI) tract are available in the literature. Here, we report two cases of AL amyloidosis presenting as submucosal hematomas in the absence of clinical disease elsewhere in the body. The 2 cases were referred to our hospital because of hematochezia. The endoscopic findings in both cases were similar in submucosal hematoma formation. However, the clinical courses differed. In the first case, there was no evidence of systemic amyloidosis and the disease was conservatively managed. In the second case, the disease progressed to systemic amyloidosis and the patient died within a short time. We conclude that the endoscopic detection of a submucosal hematoma in the setting of GI bleeding should raise suspicion of AL amyloidosis. Referral to a hematologist should be done immediately for treatment while the involvement is limited to the GI tract.
- Citation: Yoshii S, Mabe K, Nosho K, Yamamoto H, Yasui H, Okuda H, Suzuki A, Fujita M, Sato T. Submucosal hematoma is a highly suggestive finding for amyloid light-chain amyloidosis: Two case reports. World J Gastrointest Endosc 2012; 4(9): 434-437
- URL: https://www.wjgnet.com/1948-5190/full/v4/i9/434.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i9.434
Early diagnosis of amyloid light-chain (AL) amyloidosis is important because most cases are diagnosed late and have a grave prognosis. The clinical manifestations of amyloidosis may mimic other diseases, such as inflammatory bowel disease, malignancy, ischemic colitis and collagenous colitis[1]. Endoscopically, the fine granular appearance is significantly found more often in AA amyloid cases, whereas multiple polypoid protrusions and thickening of the valvulae conniventes were observed solely in AL cases[2]. However, those results were mainly obtained from investigations of cases associated with the small intestine.
Previous case reports have identified submucosal hematomas associated with AL amyloidosis; however, these were single cases in which the endoscopic appearance was not completely characterized[3,4]. Here, we report two cases of AL amyloidosis presenting as submucosal hematomas during colonoscopy.
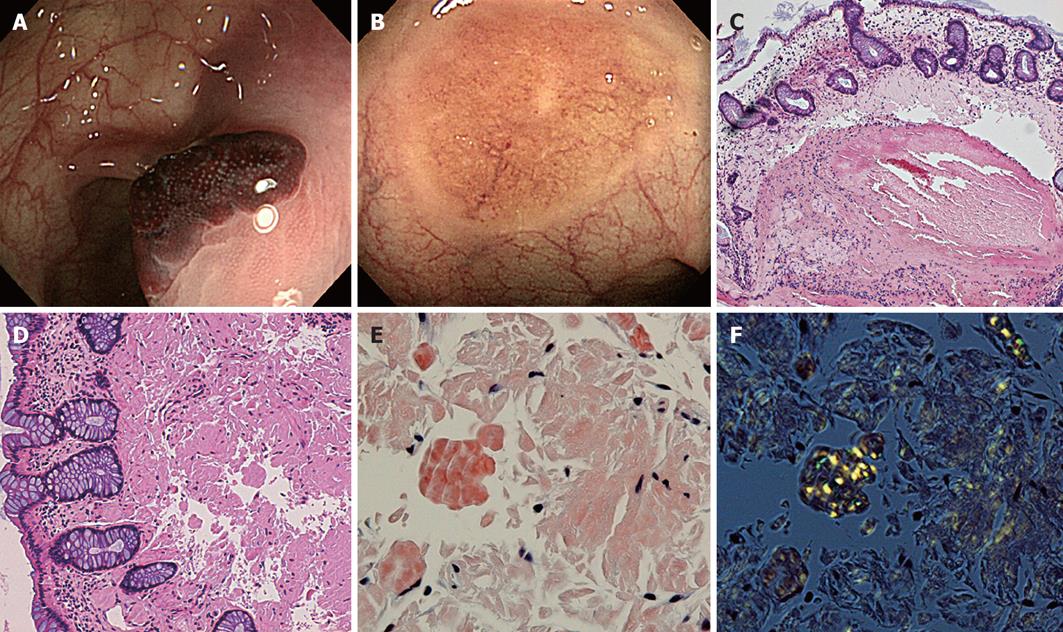
A 48-year-old woman was referred because of hematochezia. She had no past history of tuberculosis, rheumatoid arthritis or collagen vascular disease. The results of routine laboratory tests were normal. Initial colonoscopy revealed reddish elevated lesions within plaque-like erythema in the sigmoid and transverse colon. The colon surface was covered by non-neoplastic mucosa (Figure 1A).
A biopsy was not performed in the initial colonoscopy because of the possibility of vascular lesions, such as blue rubber bleb nevus syndrome, and because it might induce bleeding. Repeat colonoscopy performed after approximately 1 mo revealed a healed scar and discoid discoloration where the submucosal hematoma was located; this suggested that the lesion had healed without intervention (Figure 1B). However, another distally developed submucosal hematoma was found (not shown). It was similar to the lesion in the initial colonoscopy. Endoscopic biopsies were performed for the submucosal hematomas and discoid discoloration. There were active bleedings from both after biopsy but hemostasis was achieved by the hemoclip method.
Histological examination of a biopsy specimen from one of the submucosal hematomas revealed mucosal hemorrhages (Figure 1C) and that from the submucosal hematomas and discoid discoloration revealed deposition of amorphous material in the lamina propria and in the vessel walls of the submucosa (hematoxylin-eosin stain and Congo red stain) (Figure 1D and E). On examining the same specimen under polarized light with Congo red stain, an apple-green birefringence, which is characteristic of amyloid, was observed (Figure 1F). Staining with amyloid A, κ and λ was negative. AL amyloidosis was strongly considered in this case because a significant proportion of AL amyloid deposits could not be stained while AA amyloid could be diagnosed in all cases. Biopsies of the stomach and duodenum and immunoelectrophoresis results of the serum and urine were negative. An echocardiogram showed no evidence of amyloid infiltration. This was believed to be a case of localized AL amyloidosis of the colon. During a follow-up of approximately 2 years, the patient has been conservatively managed and remains healthy.
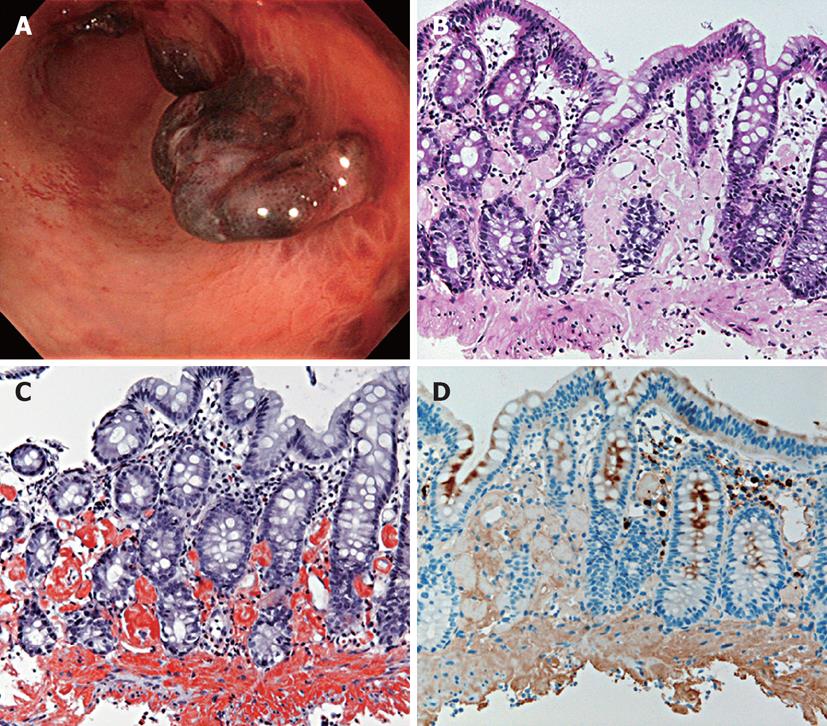
A 50-year-old woman was referred because of hematochezia and abdominal pain. Her past history solely revealed bronchial asthma. Colonoscopy revealed submucosal hematomas that resembled case 1, from the ascending colon to the rectum (Figure 2A). Endoscopic biopsies were performed for the submucosal hematomas. There was active bleeding after biopsy but hemostasis was achieved by the hemoclip method.
Histological examination revealed amyloid deposition in the lamina propria and in the vessel walls of the submucosa (hematoxylin-eosin stain and direct fast scarlet stain) (Figure 2B and C). Direct fast scarlet stain produced birefringence under polarized light. Staining with κ was positive (Figure 2D). Subcutaneous biopsy of the auricle produced the same result. A 24 h urine specimen contained more than 5 g of protein and an echocardiogram revealed thickening of the left ventricle wall. Systemic AL amyloidosis was diagnosed. We referred the patient to a hematologist and high-dose chemotherapy with hematopoietic stem cell transplantation was planned. However, the cardiac amyloidosis deteriorated and she died 2 mo later.
The clinical and endoscopic features of AL amyloidosis are diverse and mimic various other diseases[1]. Endoscopically, few reports are available in the literature on submucosal hematomas of the gastrointestinal (GI) tract[3,4]. Early diagnosis of AL amyloidosis is important because most cases are diagnosed late and have a grave prognosis. The endoscopic findings in both cases were similar in the formation of a submucosal hematoma; however, the clinical courses differed. James et al[5] investigated endoscopic findings of AL amyloidosis of the GI tract, including stomach, duodenum and colon, and reported that submucosal hematomas, as well as mucosal erosions and ulcerations, were the most common endoscopic findings. Therefore, gastroenterologists should diagnose submucosal hematomas more frequently than that indicated in past reports.
The pathogenesis of submucosal hematomas in AL amyloidosis remains unclear. Deposition of AL amyloid within vascular walls increases vessel fragility and possibly results in spontaneous bleeding beneath the lamina propria, which results in hematoma formation[5].
Untreated AL has a median 1 year mortality rate of approximately 50%[6] and survival is largely dependent on the degree of cardiac and renal involvement. Recently, high-dose chemotherapy with hematopoietic stem cell transplantation has been performed for patients with good performance status and limited cardiac involvement[1] and the 5-year survival rate in such patients is 60%. Patients in whom involvement is limited to the GI tract should be immediately referred to a hematologist for consideration of treatment.
In conclusion, the endoscopic detection of submucosal hematomas in a setting of GI bleeding should raise suspicion of AL amyloidosis, which might lead to improved prognosis of AL amyloidosis.
Peer reviewers: Jaekyu Sung, MD, PhD, Assistant Professor, Division of Gastroenterology, Department of Internal Medicine, Chungnam National University Hospital, 33 Munhwa-ro, Jung-gu, Daejeon 301-721, South Korea; Naoto Sakamoto, Associate Professor, Department of Gastroenterology, Juntendo University, 2-1-1 Hongo Bunkyo-ku Tokyo, 113-8421, Japan
S- Editor Song XX L- Editor Roemmele A E- Editor Zheng XM
| 1. | Ebert EC, Nagar M. Gastrointestinal manifestations of amyloidosis. Am J Gastroenterol. 2008;103:776-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 203] [Article Influence: 11.9] [Reference Citation Analysis (2)] |
| 2. | Tada S, Iida M, Yao T, Kawakubo K, Yao T, Okada M, Fujishima M. Endoscopic features in amyloidosis of the small intestine: clinical and morphologic differences between chemical types of amyloid protein. Gastrointest Endosc. 1994;40:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 85] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Perarnau JM, Raabe JJ, Courrier A, Peiffer G, Hennequin JP, Bene MC, Arbogast J. A rare etiology of ischemic colitis - amyloid colitis. Endoscopy. 1982;14:107-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Kaiserling E, Kröber S. Massive intestinal hemorrhage associated with intestinal amyloidosis. An investigation of underlying pathologic processes. Gen Diagn Pathol. 1995;141:147-154. [PubMed] |
| 5. | James DG, Zuckerman GR, Sayuk GS, Wang HL, Prakash C. Clinical recognition of Al type amyloidosis of the luminal gastrointestinal tract. Clin Gastroenterol Hepatol. 2007;5:582-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Comenzo RL. Amyloidosis. Curr Treat Options Oncol. 2006;7:225-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |