Published online Dec 16, 2012. doi: 10.4253/wjge.v4.i12.556
Revised: September 5, 2012
Accepted: October 20, 2012
Published online: December 16, 2012
AIM: To prospectively assess the hemostatic efficacy of the endoscopic topical use of ankaferd blood stopper (ABS) in active non-variceal upper gastrointestinal system (GIS) bleeding.
METHODS: Endoscopy was performed on 220 patients under suspiciency of GIS bleeding. Patients with active non-variceal upper gastrointestinal bleeding (NVUGIB) with a spurting or oozing type were included. Firstly, 8-10 cc of isotonic saline was sprayed to bleeding lesions. Then, 8 cc of ABS was applied on lesions in which bleeding continued after isotonic saline application. The other endoscopic therapeutic methods were applied on the lesions in which the bleeding did not stop after ABS.
RESULTS: Twenty-seven patients had an active NVUGIB with a spurting or oozing type and 193 patients were excluded from the study since they did not have non-variceal active bleeding. 8 cc of ABS was sprayed on to the lesions of 26 patients whose bleeding continued after isotonic saline and in 19 of them, bleeding stopped after ABS. Other endoscopic treatment methods were applied to the remaining patients and the bleeding was stopped with these interventions in 6 of 7 patients.
CONCLUSION: ABS is an effective method on NVUGIB, particularly on young patients with no coagulopathy. ABS may be considered as part of a combination treatment with other endoscopic methods.
- Citation: Gungor G, Goktepe MH, Biyik M, Polat I, Tuna T, Ataseven H, Demir A. Efficacy of ankaferd blood stopper application on non-variceal upper gastrointestinal bleeding. World J Gastrointest Endosc 2012; 4(12): 556-560
- URL: https://www.wjgnet.com/1948-5190/full/v4/i12/556.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i12.556
Upper gastrointestinal system (GIS) bleeding is a frequently seen emergent situation with a mortality of about 7%-10%[1]. This rate may increase with concomitant co-morbid diseases.
Endoscopy is the gold-standard technique in the diagnosis of gastrointestinal bleeding. It provides important information about the bleeding point, its localization, the amount of bleeding and risk for re-bleeding. Active bleeding may be stopped with therapeutic applications and the risk of re-bleeding may be reduced. Endoscopic treatment methods are indicated in lesions with active bleeding and with a visible vessel[2]. Endoscopic treatment may be disputable for lesions with a blood clot; however, the data of recent years demonstrate that it may be effective to apply endoscopic treatment for these lesions rather than to observe them[3]. Endoscopic treatment is not necessary for a clean-based ulcer since the re-bleeding risk is minimal[2]. Injection treatments, cauterization methods and mechanical therapies are the major endoscopic treatment modalities[4].
In recent years, it was reported that ankaferd blood stopper (ABS), of which each 100 milliliter of folkloric liquid product contains a standard mixture of 5 mg of Thymus Vulgaris (thyme-dried herbal extract), 9 mg of Glycyrrhiza Glabra (licorice-dried leaf extract), 8 mg of Vitis Vinifera (grape-dried leaf extract), 7 mg of Alpinia Officinarum (lesser galangal-dried leaf extract) and 6 mg of Urtica Dioica (stinging nettle-dried root extract), forms a system by precipitating fibrinogen and forming a protein network which acts as an anchor for vital physiological erythrocyte aggregation, covering the classical cascade model of the clotting system, independently acting on coagulation factors and platelets in blood and serum. It was also reported that it provides this effect in milliseconds in in vitro conditions and seconds in in vivo conditions. The topical use of ABS has been approved by the Turkish Ministry of Health for the management of dermal, external post-surgical and post-dental surgery bleeding[5].
It was reported that ABS was applied on bleeding lesions of GIS malignancies[6,7], peptic ulcers[8], fundal varices[9], dieulafoy lesions[10,11], radiation colitis[12], rectal ulcers[13] and non-variceal upper gastrointestinal bleeding (NVUGIB)[14]. Most of the bleeding lesions were controlled in all patient groups. However, controlled trials are not available about this topic.
We researched the efficacy of ABS application with a spray catheter on active NVUGIB lesions.
Endoscopy was performed on 220 patients under suspiciency of GIS bleeding within 12 h of admission to Selcuk University, Meram Faculty of Medicine, between April 2009 and August 2010, after approval of the local ethics committee. All volunteers gave written informed consent. Twenty-seven patients with active spurting or oozing type NVUGIB were included in the study and 193 patients without these conditions were excluded. Firstly, 8-10 cc of isotonic saline was sprayed on to the bleeding lesions. 8 cc of ABS was applied with a Medi-Globe® spray catheter on lesions in which bleeding continued after isotonic saline application. Air was applied with an injector to the catheter after ABS application and the product was completely discharged from the catheter. The other endoscopic hemostatic methods (injection treatment, hemoclip, electro-coagulation, heater probe, Argon Plasma Coagulation) were applied on the lesions in which the bleeding did not stop within one minute after ABS application. They were then observed for re-bleeding. The control endoscopy was performed approximately 48 h after the first endoscopy. Also, we treated all patients during admission and at the time of discharge with specific medical therapies (such as proton pump inhibitors, transfusion, intravenous hydration, other co-mobidity drugs).
Endoscopy was performed on 220 patients with suspiciency of NVUGIB. Twenty-seven of these patients had NVUGIB with a spurting or oozing type. 193 patients were excluded from the study since they did not have non-variceal active bleeding. In most of these 193 patients, in endoscopy, bleeding was stopped or there was hematinized blood in the stomach, visible vessel or blood clot stuck on their lesions. Ten patients (37%) were women, 17 (63%) men and the mean age was 59.1% ± 17%. 70% of all patients (19 patients) had co-morbid diseases. Two patients had chronic obstructive lung diseases, 2 a mitral valve replacement, 2 chronic renal failure, 2 malignancy, 1 liver cirrhosis, 1 atrial fibrillation, 1 coronary artery disease and 4 patients had a history of gastric surgery. Twelve patients had a GIS bleeding history. It was observed that 46% of patients complained of melena, 38.4% hematemesis and melena, 7.7% hematemesis and 7.4% malaise, anemia and other complaints.
Firstly, 8 cc isotonic saline was sprayed on to bleeding lesions. The bleeding was stopped in one patient after isotonic saline application but re-bleeding was observed during the follow up.
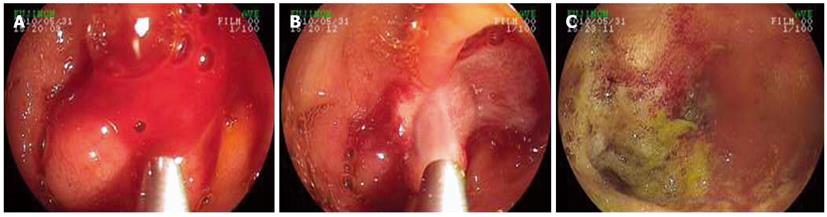
8 cc of ABS was sprayed to the lesions of 26 patients whose bleeding continued after isotonic saline and bleeding was stopped in 19 of these 26 patients after ABS. Images of endoscopic ABS application are shown in Figures 1 and 2.
The other endoscopic methods could not be applied to 1 of 7 patients whose bleeding continued after ABS since the bleeding was a widespread mucosal oozing type. The other endoscopic treatment methods in addition to ABS were applied to the remaining 6 patients (argon plasma coagulation, injection sclerotherapy, hemoclip) and it was observed that the bleeding stopped with these interventions on all patients.
It is not ethical to form only one placebo group of active bleeding patients. It was statistically significant that ABS only and ABS + other methods are superior to stop the bleeding when isotonic saline application is considered as an ineffective placebo (McNemar test, for each P = 0.001) and no statistically significant difference was observed between ABS only and ABS + classical methods.
The rate of re-bleeding was 15.8% in patients whose bleeding was controlled with ABS only, 33.3% in patients whose bleeding was brought under control by applying ABS + classical methods and 20% in all patients. Results of endoscopic treatments are shown Table 1.
| Group | |||||
| Endoscopic treatment | Stopped (n) | Not stopped (n) | Re-bleeding, n (%) | Transfusion (unit) | Hospitalization (d) |
| Isotonic saline | 1 | 26 | 1 (3.8) | 3 | 1 |
| ABS only | 19 | 7 | 3 (15.8) | 2.4 | 6 |
| ABS + Other Methods | 2 (33.3) | 4.4 | 6.75 | ||
| ABS + Adrenaline | 4 | 0 | |||
| ABS + Adrenaline + Hemoclip | 1 | 0 | |||
| ABS + Adrenaline + Polidocanol | 1 | 0 | |||
No statistically significant difference was found in patients whose bleeding was stopped by applying ABS only in terms of age and gender.
The mean age of 19 patients whose bleeding was stopped by applying ABS was 55 and 68 in the 7 patients whose bleeding could not be stopped by applying ABS. Although this is not a statistically significant difference (Mann Whitney U test, P = 0.95), the mean age was higher in patients whose bleeding could not be stopped.
Peptic ulcer was the most common bleeding lesion and this is compatible with the literature. The endoscopic diagnosis and results of ABS application are given in Table 2.
| Group | |||
| Endoscopic finding | Stopped (n) | Not Stopped (n) | Total (n) |
| Gastric ulcer | 2 | 1 | 3 |
| Duodenal ulcer | 9 | 3 | 12 |
| Erosive ulcer | 0 | 2 | 2 |
| Esophagitis | 2 | 0 | 2 |
| Anastomosis ulcer | 2 | 0 | 2 |
| Dieulafoy lesion | 1 | 1 | 2 |
| Post-polypectomy | 2 | 0 | 2 |
| Malignancy | 1 | 0 | 1 |
| Total | 19 | 7 | 26 |
Patients in whom only ABS was applied were evaluated according to the bleeding type. 15.3% of them had a spurting type and 84.7% an oozing type. Bleeding control was provided with ABS on 3 of 4 patients (75%) with bleeding of a spurting type and 16 of 22 patients (72%) with bleeding of an oozing type. There was no statistically significant difference between spurting and oozing types of lesions for bleeding control with ABS (Fisher’s Exact test, P = 1.0).
The mean thrombocyte count was 229.771/mm3 of the 19 patients whose bleeding was stopped by applying ABS and 132.232/mm3 of the 7 patients whose bleeding could not be stopped by applying ABS. This difference was statistically significant (independent sample test, P = 0.005). However, the mean INR value of 19 patients whose bleeding was controlled was 1.33 and activa partial thromboplastin time (aPTT) was 27.5 s, while the mean INR value of 7 patients whose bleeding could not be controlled was 3.07 and aPTT was 39.1 s.
If one or more of the abnormal results of thrombocyte count, PT-INR or aPTT levels were defined as coagulopathy, it was abnormal in patients whose bleeding could not be stopped with ABS application and it was statistically significant (F-test, P = 0.006).
The drug usage and results of the only ABS group are given in Table 3. It was observed that the bleeding of 3 of 6 patients who were taking ASA and 1 of 2 patients who were taking ASA + warfarin did not stop with applying ABS. These results demonstrated that the bleeding control with ABS was more difficult for patients who were taking ASA and/or warfarin.
| Group | |||
| Drug | Stopped (n) | Not Stopped (n) | Total (n) |
| Not taking a drug | 10 | 2 | 12 |
| ASA | 3 | 3 | 6 |
| Warfarin | 1 | 1 | 2 |
| ASA + NSAID | 1 | 0 | 1 |
| ASA + Warfarin | 0 | 1 | 1 |
| Steroid | 1 | 0 | 1 |
| Other | 3 | 0 | 3 |
| Total | 19 | 7 | 26 |
There is insufficient literature that demonstrates the efficacy of ABS on gastrointestinal bleeding and the available data are mostly case reports or case series. This study is the first prospective study in which ABS is applied on non-variceal gastrointestinal system bleeding and the effects of many factors on bleeding control analyzed.
According to these results, the rate of bleeding control was 73% with ABS only, 100% with ABS in combination with classical methods and 96% with ABS only and ABS + classical methods. When isotonic saline application is considered an ineffective placebo, it was observed that ABS only and ABS + other methods are superior to placebo and statistically significant. The advanced age of patients made it difficult to control bleeding with ABS.
When the study is evaluated in terms of re-bleeding, re-bleeding was observed in 15.8% of patients whose hemostasis was provided with ABS only, 33.3% with ABS + classical methods and 20% with ABS only and ABS + classical methods. According to the literature, the rate of re-bleeding is about 100%[4] in spurting or oozing type bleedings if no endoscopic treatment is applied, 20% in adrenaline injection, 15%-20% in ablative treatment and 5%-15% in combination treatment. In this study, the rate of re-bleeding of patients with ABS only and provided hemostasis was similar to the other endoscopic methods[15-17] mentioned in the literature.
The results of this study also demonstrate that ABS application with a spray catheter may have a limited effect on bleeding control of patients with coagulopathy or using ASA and/or warfarin. In such situations, more ABS and a mechanical compress may be applied on lesions as an alternative technique or ABS may be applied on patients with other endoscopic methods, such as a combination treatment, as a different approach.
The application of ABS on lesions with a spray catheter may provide a more homogenous and effective contact with lesions compared to the application with a nasogastric catheter or tools like tubes. In addition, the contact time of ABS applied to the bleeding point may have an important role in stopping the bleeding. The methods which provide a longer contact time of ABS to the bleeding point (balloon or compression tools like a funnel) may be more useful.
In summary, these results demonstrate that the application of ABS with topical spraying for bleeding control on non-variceal upper GIS bleeding, particularly on young patients without coagulopathy, is effective. ABS may be considered as a part of combination treatment for cases with a higher re-bleeding possibility (coagulopathy, dieulafoy lesion, arterial bleeding, etc.)[10,11].
Randomized controlled studies are needed for the comparison of ABS application alone and in combination with other endoscopic methods (e.g., thermo-coagulation, clips or adrenaline injection).
Injection treatments, cauterization methods and mechanical therapies are the major endoscopic treatment modalities in active gastrointestinal bleeding. In recent years, it was reported that ankaferd blood stopper (ABS) forms a system by precipitating fibrinogen and forming a protein network which acts as an anchor for vital physiological erythrocyte aggregation, covering the classical cascade model of the clotting system, independently acting on coagulation factors and platelets in blood and serum. The authors researched the efficacy of ABS application with a spray catheter on active non-variceal upper gastrointestinal bleeding (NVUGIB) lesions.
This study investigated the efficacy of a different technique in non-variceal gastrointestinal bleeding.
It was reported that ABS was applied on bleeding lesions of gastrointestinal system (GIS) malignancies, fundal varices, dieulafoy lesions, radiation colitis, rectal ulcers and NVUGIB. Most of the bleeding lesions were controlled in all patient groups. However, controlled trials are not available about this topic.
This study demonstrates that the application of ABS with topical spraying for bleeding control on non-variceal upper GIS bleeding, particularly on young patients without coagulopathy, is effective.
The application of ABS on lesions with a spray catheter may provide a more homogenous and effective contact with lesions compared to the application with a nasogastric catheter or tools like tubes. In addition, the contact time of ABS applied to the bleeding point may have an important role in stopping the bleeding. The methods which provide a longer contact time of ABS to the bleeding point (balloon or compression tools like a funnel) may be more useful.
Ankafeld blood stopper contains a standard mixture of 5 mg of Thymus Vulgaris (thyme-dried herbal extract), 9 mg of Glycyrrhiza Glabra (licorice-dried leaf extract), 8 mg of Vitis Vinifera (grape-dried leaf extract), 7 mg of Alpinia Officinarum (lesser galangal-dried leaf extract) and 6 mg of Urtica Dioica (stinging nettle-dried root extract) in each 100 mL of liquid folkloric product effective in coagulation.
The application of ABS on lesions with a spray catheter may be helpful in the control of gastrointestinal bleeding alone or in combination treatment with other endoscopic methods.
Peer reviewer: Naoki Muguruma, MD, PhD, Department of Gastroenterology and Oncology, the University of Tokushima Graduate School, 3-18-15, Kuramoto-cho, Tokushima 770-8503, Japan
S- Editor Song XX L- Editor Roemmele A E- Editor Zhang DN
| 1. | Yavorski RT, Wong RK, Maydonovitch C, Battin LS, Furnia A, Amundson DE. Analysis of 3,294 cases of upper gastrointestinal bleeding in military medical facilities. Am J Gastroenterol. 1995;90:568-573. [PubMed] |
| 2. | Johnston JH. Endoscopic risk factors for bleeding peptic ulcer. Gastrointest Endosc. 1990;36:S16-S20. [PubMed] |
| 3. | Bleau BL, Gostout CJ, Sherman KE, Shaw MJ, Harford WV, Keate RF, Bracy WP, Fleischer DE. Recurrent bleeding from peptic ulcer associated with adherent clot: a randomized study comparing endoscopic treatment with medical therapy. Gastrointest Endosc. 2002;56:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 95] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Adler DG, Leighton JA, Davila RE, Hirota WK, Jacobson BC, Qureshi WA, Rajan E, Zuckerman MJ, Fanelli RD, Hambrick RD. ASGE guideline: The role of endoscopy in acute non-variceal upper-GI hemorrhage. Gastrointest Endosc. 2004;60:497-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Goker H, Haznedaroglu IC, Ercetin S, Kirazli S, Akman U, Ozturk Y, Firat HC. Haemostatic actions of the folkloric medicinal plant extract Ankaferd Blood Stopper. J Int Med Res. 2008;36:163-170. [PubMed] |
| 6. | Kurt M, Akdogan M, Onal IK, Kekilli M, Arhan M, Shorbagi A, Aksu S, Kurt OK, Haznedaroglu IC. Endoscopic topical application of Ankaferd Blood Stopper for neoplastic gastrointestinal bleeding: A retrospective analysis. Dig Liver Dis. 2010;42:196-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 54] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Ozaslan E, Purnak T, Yildiz A, Haznedaroglu IC. A new practical alternative for tumoural gastrointestinal bleeding: Ankaferd blood stopper. Dig Liver Dis. 2010;42:594-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Purnak T, Ozaslan E, Beyazit Y, Haznedaroglu IC. Upper gastrointestinal bleeding in a patient with defective hemostasis successfully treated with ankaferd blood stopper. Phytother Res. 2011;25:312-313. [PubMed] |
| 9. | Tuncer I, Doganay L, Ozturk O. Instant control of fundal variceal bleeding with a folkloric medicinal plant extract: Ankaferd Blood Stopper. Gastrointest Endosc. 2010;71:873-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Kurt M, Kacar S, Onal IK, Akdogan M, Haznedaroglu IC. Ankaferd Blood Stopper as an effective adjunctive hemostatic agent for the management of life-threatening arterial bleeding of the digestive tract. Endoscopy. 2008;40 Suppl 2:E262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Kurt M, Onal I, Akdogan M, Kekilli M, Arhan M, Sayilir A, Oztas E, Haznedaroglu I. Ankaferd Blood Stopper for controlling gastrointestinal bleeding due to distinct benign lesions refractory to conventional antihemorrhagic measures. Can J Gastroenterol. 2010;24:380-384. [PubMed] |
| 12. | Ozaslan E, Purnak T, Yildiz A, Akar T, Avcioglu U, Haznedaroglu IC. The effect of Ankaferd blood stopper on severe radiation colitis. Endoscopy. 2009;41 Suppl 2:E321-E322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Ibis M, Kurt M, Onal IK, Haznedaroglu IC. Successful management of bleeding due to solitary rectal ulcer via topical application of Ankaferd blood stopper. J Altern Complement Med. 2008;14:1073-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Ozaslan E, Purnak T, Yildiz A, Haznedaroglu IC. The effect of a new hemostatic agent for difficult cases of non-variceal gastrointestinal bleeding: Ankaferd blood stopper. Hepatogastroenterology. 2010;57:191-194. [PubMed] |
| 15. | Elta GH. Acute Nonvariceal Upper Gastrointestinal Hemorrhage. Curr Treat Options Gastroenterol. 2002;5:147-152. [PubMed] |
| 16. | Kovacs TO, Jensen DM. Endoscopic treatment of ulcer bleeding. Curr Treat Options Gastroenterol. 2007;10:143-148. [PubMed] |
| 17. | Llach J, Bordas JM, Salmerón JM, Panés J, García-Pagán JC, Feu F, Navasa M, Mondelo F, Piqué JM, Mas A. A prospective randomized trial of heater probe thermocoagulation versus injection therapy in peptic ulcer hemorrhage. Gastrointest Endosc. 1996;43:117-120. [PubMed] |