Published online Jul 16, 2011. doi: 10.4253/wjge.v3.i7.140
Revised: June 23, 2011
Accepted: July 31, 2011
Published online: July 16, 2011
Endoscopic retrograde cholangiopancreatography (ERCP) is an important tool for the diagnosis and treatment of the hepatobiliary system. The use of fluoroscopy to aid ERCP places both the patient and the endoscopy staff at risk of radiation-induced injury. Radiation dose to patients during ERCP depends on many factors, and the endoscopist cannot control some variables, such as patient size, procedure type, or fluoroscopic equipment used. Previous reports have demonstrated a linear relationship between radiation dose and fluoroscopy duration. When fluoroscopy is used to assist ERCP, the shortest fluoroscopy time possible is recommended. Pulsed fluoroscopy and monitoring the length of fluoroscopy have been suggested for an overall reduction in both radiation exposure and fluoroscopy times. Fluoroscopy time is shorter when ERCP is performed by an endoscopist who has many years experience of performing ERCP and carried out a large number of ERCPs in the preceding year. In general, radiation exposure is greater during therapeutic ERCP than during diagnostic ERCP. Factors associated with prolonged fluoroscopy have been delineated recently, but these have not been validated.
- Citation: Boix J, Lorenzo-Zúñiga V. Radiation dose to patients during endoscopic retrograde cholangiopancreatography. World J Gastrointest Endosc 2011; 3(7): 140-144
- URL: https://www.wjgnet.com/1948-5190/full/v3/i7/140.htm
- DOI: https://dx.doi.org/10.4253/wjge.v3.i7.140
Endoscopic retrograde cholangiopancreatography (ERCP) is an important tool for the diagnosis and treatment of the hepatobiliary system. Recent data indicate that ERCP is becoming a major therapeutic strategy for biliary disease in developed and developing countries. In the diagnosis process, MRCP is generally preferred to ERCP. During the performance of ERCP, a large number of X-ray fluoroscopy and digital radiographs are performed, making it an interventional radiological (IR) procedure. ERCP is highly technical and depends on endoscopist’s experience. High quality ERCP outcomes and limitation of ERCP-related complications depend on good training. The use of fluoroscopy to aid ERCP, places both the patient and the endoscopy staff at risk of radiation-induced injury[1,2]. It is essential to establish the appropriate conditions for radiography in all circumstances, in order to avoid unnecessary exposure of patients and staff to potentially harmful radiation. This means that precautions should be taken to keep the radiation dose to both the personnel participating in ERCP procedures and to patients as low as reasonably achievable (ALARA principle).
The identification of predictive factors of fluoroscopy time and radiation exposure to patients undergoing ERCP are beyond the scope of this guideline.
X-rays consist of ionizing radiation, such as gamma rays, emitted by radioactive substances. They cause ionization in the medium through which they pass. The ionization produced can lead to DNA damage or cell death. Radiation effects are broadly divided into two categories: deterministic effects (e.g. cataract formation, infertility, skin injury, and hair loss); and stochastic effects (cancer and genetic effects). The harm depends on the amount of radiation absorbed by the body, known as the radiation dose or, simply -dose.
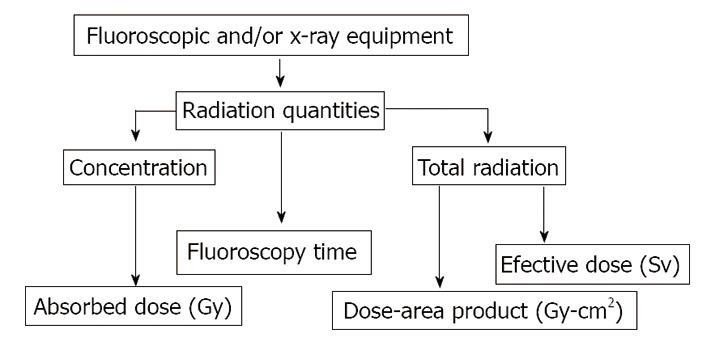
There are two types of expression for quantities of radiation, those that express the concentration of radiation at some point, or to a specific tissue or organ, and those that express the total radiation delivered to a body.
Exposure indicators usually measured in ERCP are absorbed dose, as a measure of radiation concentration, two measures of total radiation (effective dose and dose-area product) and fluoroscopy time.
Absorbed dose is the measure used to quantify the concentration of radiation energy actually absorbed in a specific tissue. This is the measure that is most directly related to biological effects. Dose values can be in the traditional unit of the rad or the SI unit of the gray (Gy).
Effective dose is a very useful radiation quantity for expressing relative risk to humans, both patients and other personnel. It is actually a simple and very logical concept, and is expressed as joules per kilogram (J kg-1), expressed in the SI unit of the sievert (Sv). For the purpose of determining effective dose, the different areas and organs have been assigned tissue weighting factor (wT) values. It is generally assumed that the exposure to natural background radiation is somewhat uniformly distributed over the body. Since the tissue WT for the total body has the value of one (1), the effective dose is equal to the absorbed dose.
Effective dose (Sv)= Absorbed dose (Gy) × WT (1)
Dose-area product (DAP) provides a good estimation of the total radiation energy delivered to a patient during a procedure and is strongly correlated to the fluoroscopy time. It is the most practical measure for monitoring the radiation delivered to patients. DAP is just the product of the air kerma ,in Gy or mGy, and the exposed area in cm2 (Gy-cm2)(Figure 1).
Radiation dose monitoring in patients undergoing diagnostic or IR procedures has been widely adopted in clinical practice, but data on patient doses during ERCP are very scarce[3-7].
Gastroenterologists who are involved in ERCP procedures may work at specialized centres and may perform multiple procedures daily. In all circumstances in which fluoroscopic and/or x-ray equipment is used, gastroenterologists should minimize the risks to patients, themselves, and other members of the staff[3,4,7]. The amount of radiation currently being used by endoscopist is relatively small, effective doses of 0-3 mSv/year, in comparison with interventional radiologists and interventional cardiologists[8]. When physician doses were serially measured, endoscopists was found to be exposed to larger amounts of radiation than their assistants because the endoscopist was typically closer to the x-ray sources[7]. The dose limit that is recommended by the International Commission on Radiological Protection (ICRP) and adopted by most countries is 20 mSv/year[9]. For situations where the annual dose limit exceeds 20 mSv, it is recommended that the dose should not exceed 50 mSv in any particular year or 100 mSv over 5 years. This dose limit is based on the calculation of radiation risk over a full working life from the age of 18 years to 65 years (47 years) at the rate of 20 mSv per year, amounting to 20 × 47 = 940 mSv (approximately 1 Sv). Epidemiologic research has estimated a 10% increase in cancer risk with a lifetime occupational exposure of 1 Sv[10]. An occupational exposure of 1 Sv of radiation is probably significantly greater than the true effective dose that would be accumulated by an endoscopist with radiation exposure solely from ERCP. Despite the relatively low risk of radiation-induced injury, endoscopists should be aware that all exposure carries a cumulative risk[11]. Additionally, tracking the radiation dose can be difficult because almost 50% of endoscopist performing ERCPs never wear a dosimeter[12]. For the patient, the source of exposure is the direct beam from the x-ray tube. It is estimated that patients receive about 2-16 min of fluoroscopy during ERCP, with therapeutic procedures taking significantly longer[13]. Studies have found that DAP values of approximately 13-66 Gy/cm2 are used during ERCP, with effective doses ranging from 2 to 6 mSv per procedure[11].
Radiation dose to patients during ERCP depends on many factors[14], and the endoscopist cannot control some variables, such as patient size, procedure type, or fluoroscopic equipment used.
During ERCP, the positioning of catheters and guide wires is verified fluoroscopically. Once contrast injections have been given, fluoroscopy is used to evaluate the anatomy of the ductal systems of both the biliary tree and pancreas and to help assess whether disease is present. Photographic documentation is usually obtained to record the findings by capturing the last fluoroscopic image, spot image, or image sequence, depending on the available features of the equipment used. Finally, fluoroscopy is also needed to assist with therapy in, for example, sphincterotomy, stone extraction, biopsy or cytology, and stent placement. Additional devices that allow direct visualization of the ductal anatomy may ultimately reduce the need for fluoroscopy.
Previous reports have demonstrated a linear relationship between radiation dose and fluoroscopy duration[2,3,13]. When fluoroscopy is used to assist ERCP, the shortest fluoroscopy time possible is recommended[11].
Monitoring the length of fluoroscopy has been recommended as part of an overall reduction in both radiation exposure and fluoroscopy times[15]. Factors associated with prolonged fluoroscopy duration have been delineated re-
cently[11], but have not been validated.
In order to determine what factors influence fluoroscopy time, several aspects should be considered.
Some factors, such as the type of equipment (fixed units vs portable C-arm units) have been shown to reduce radiation dose but are unfortunately not easily implemented[16]. The radiation beam can be adjusted to use the lowest effective voltage required to a produce clinically useful image, and shielding of patients and staff with either permanent (walls or barriers) or portable (drapes, aprons) mechanisms has also been shown to reduce exposure effectively[7].
A specific intervention directed at decreasing radiation exposure involves the use of intermittent or pulsed fluoroscopy that substantially reduces the radiation dose without sacrificing image quality[17]. Time-limited fluoroscopy, in which x-ray exposure was limited to a set period each time that the foot- operated switch is depressed, led to decreased fluoroscopy duration in a prospective study[18]. In addition, alarms that indicate prolonged fluoroscopy time could potentially reduce radiation by increased awareness during the procedure.
More modern equipment incorporates features such as pulsed fluoroscopy, whereby the x-ray beam is turned on and off at a fixed rate (eg, at 4, 8, or 15 pulses per second), significantly reducing exposure compared with an x-ray beam used continuously[4,18].
ERCP is traditionally performed with the patient in the prone position as this is considered optimal for cannulation of the papilla, for obtaining high-quality radiographic images and for the prevention of pulmonary aspiration. Patients who cannot tolerate the prone position for ERCP are often placed in the left lateral decubitus or supine positions. However, the supine position allows improved fluoroscopic visualization, especially when rotatable fluoroscopic equipment (eg, C-Arm) is not available[19]. In addition, the supine position sometimes allows superior visualization of hilar anatomy[20]. Nonetheless, little data exist regarding performance of ERCP with the patient in the supine position. In one randomized trial of patients undergoing ERCP in the prone and supine positions, there were significantly more failures and a significantly higher number of adverse cardio-respiratory events in the supine group when they were not endotracheally intubated[21]. In another retrospective study of 649 patients undergoing ERCP by a single endoscopist, success and complication rates were similar for supine and prone patients (90.2% and 11.2% for supine and 92.5% and 9.1%for prone, respectively), although the degree of procedural difficulty was significantly higher in the supine group[20].
Both cumulative years of performing ERCP and ERCP volume in the preceding year have been independently associated with shorter fluoroscopy exposure.Currently, there are insufficient data to support the use of fluoroscopy time as a surrogate end point for competency, even though this is an easily measureable and comparable variable. Fluoroscopy time is shorter when ERCP is performed by endoscopist with many years of performing ERCP and a large number of ERCPs in the preceding year[14]. In interventional radiology, increased levels of physician training have been found to correlate with decreases in patient radiation exposure during fluoroscopic procedures[22]. Uradomo et al[23] showed that radiation exposure during ERCP was directly related to the experience of trainees. Furthermore, as GI fellows accumulate ERCP experience, the amount of time that patients are exposed to fluoroscopy, and thus radiation exposure, is decreased. Jowell et al[24] assessed the ability of GI fellows to competently complete specific technical component of ERCP. They found that between 180 and 200 ERCPs were required for the trainees to consistently complete these procedures. The median fluoroscopy duration decreased by almost 3 min during cases performed by GI fellows with experience of more than 50 previous ERCPs[11]. The lack of correlation of fluoroscopy time and endoscopist experience, reported in another study, may actually reflect case complexity because the more difficult and refractory cases were clearly referred to the more senior endoscopist[11].
In general, radiation exposure is greater during therapeutic ERCP than during diagnostic ERCP[4,7,23,25]. In a recent prospective study[11], the procedure variables that significantly increased fluoroscopy duration were stent insertion, lithotripsy, use of a needle-knife, biopsies, the use of a guide wire or additional wires other than the standard, and use of a balloon catheter.
The factors found to extend the length of the procedure and increase fluoroscopy duration probably relate to differences in case complexity. Stent insertion may prolong fluoroscopy duration because this procedure requires fluoroscopy to confirm proper placement[25]. The use of a lithotripter is associated with a significant increase in fluoroscopy duration because this device is often used for difficult stone extractions. A needle-knife is usually used for second-line access techniques when conventional methods have failed and is often associated with long procedures. Guide wires used during ERCP are associated with longer fluoroscopy. The use of an “other wire” is associated with one of the greatest increases in fluoroscopy duration and is probably associated with difficult access/cannulation during procedures where there have been multiple previous attempts using more conventional guide wires. Finally, the use of the balloon catheter is often followed by a balloon cholangiogram, requiring more fluoroscopy time.
A person’s biological risk is measured by using the conventional unit rem (radiation equivalents in man) or the SI unit equivalent called the sievert, where 1 Sv = 100 rem. Estimates of radiation exposure to endoscopy staff vary, but it should be noted that radiation exposure is cumulative over time. In a recent study, the estimated annual whole-body effective dose equivalent received by the endoscopist ranged between 3.35 and 5.87 mSv[26]. The ICRP has classified radiation exposure as low (≤ 3 mSv per year), moderate (3-20 mSv per year), or high (> 20-50 mSv per year).
The primary source of radiation to endoscopy personnel is radiation scattered from the patient, not the primary x-ray beam. Positioning staff as far away from the patient as possible is essential in limiting exposure. If an endoscopy staff member is standing 1 m from the patient, the radiation exposure for that individual is 1/1000 the patient’s exposure.
Shielding is required for all staff in the fluoroscopy unit. Aprons containing lead shielding 0.5 mm thick are standard in most fluoroscopy units and block more than 90% of scattered radiation[9]. Average effective doses of about 0.07 mSv per procedure have been observed for endoscopists wearing a lead apron. Although the endoscopist’s body is well protected by a lead apron, there can also be substantial doses to unshielded parts. Average doses to the eyes in the range of 0.1-1.7 mGy per procedure and doses of about 0.5 mGy to the hands have been reported[9]. Optically clear lead glasses can reduce the operator’s eye exposure by 85% to 90%. There are no mandatory requirements for either thyroid shields or leaded glasses, although many have recommend that thyroid shields should be used routinely and leaded glasses should be used by individuals with high case loads[1].
During pregnancy, the most common indication for ERCP is treatment of choledocholitiasis. The incidence of gallstone disease during pregnancy has been estimated to be between 4.5% and 12%[27]. Patients usually require immediate intervention because of potentially life-threatening cholangitis or gallstone pancreatitis.
When a pregnant patient requires ERCP for therapy, the procedure should be optimized by strict adherence to good technique. In addition, if there is a possibility that the primary x-ray beam may intercept the fetus, placing a lead apron between the x-ray source and the fetus is effective. However, a lead apron placed externally is ineffective for protection of the fetus from exposure to radiation that is scattered inside the patient’s body. The patient’s position (supine, prone, or lateral) should be adjusted to minimize fetal exposure. A poster anterior projection of the x-ray beam is recommended, as this results in a fetal dose that is 20%-30% lower than in the anteroposterior projection due to increased shielding from the mother’s tissues[28]. The lateral projection also provides increased fetal shielding, but the patient’s entrance dose rate may be three to seven times higher in comparison with a frontal projection. As a result, the lateral projection results in a higher fetal dose[28].
Intraductal ultrasound can be used instead of fluoroscopy to check for bile duct stones and to place guide a wire for a biliary stent. An alternative technique, avoiding radiation exposure completely, involves conducting ERCP without fluoroscopy, using wire-guided cannulation. Choledochoscopy can be used to confirm stone clearance. However, this approach is technically challenging and has only been used by very experienced biliary endoscopists. Further studies are required to prove that the clinical efficiency of radiation-free ERCP remains at the same level as that of conventional fluoroscopically guided ERCP[29].
The use of fluoroscopy to aid ERCP, places both the patient and the endoscopy staff at risk of radiation-induced injury. ERCP is highly technical and depends on the endoscopist’s experience. Radiation dose to patients during ERCP depends on many factors, and the endoscopist cannot control some variables, such as patient size, procedure type, or fluoroscopic equipment used. Previous reports have demonstrated a linear relationship between radiation dose and fluoroscopy duration. When fluoroscopy is used to assist ERCP, the shortest fluoroscopy time possible is recommended. Factors associated with prolonged fluoroscopy duration have been delineated recently, but these have not been validated.
Peer reviewers: Wai-Keung Chow, Visiting Staff, Division of Gastroenterology, Department of Internal Medicine, China Medical University Hospital, Taichung, Taiwan, China; Viktor Ernst Eysselein, MD, Professor of Medicine, Division of Gastroenterology, Harbor-UCLA Medical Center, 1000 W. Carson Street, Box 483, Torrance, CA 90509, United States
S- Editor Zhang HN L- Editor Hughes D E- Editor Zhang L
| 1. | Amis ES, Butler PF, Applegate KE, Birnbaum SB, Brateman LF, Hevezi JM, Mettler FA, Morin RL, Pentecost MJ, Smith GG. American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol. 2007;4:272-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 637] [Cited by in RCA: 579] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 2. | Campbell N, Sparrow K, Fortier M, Ponich T. Practical radiation safety and protection for the endoscopist during ERCP. Gastrointest Endosc. 2002;55:552-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Buls N, Pages J, Mana F, Osteaux M. Patient and staff exposure during endoscopic retrograde cholangiopancreatography. Br J Radiol. 2002;75:435-443. [PubMed] |
| 4. | Larkin CJ, Workman A, Wright RE, Tham TC. Radiation doses to patients during ERCP. Gastrointest Endosc. 2001;53:161-164. [PubMed] |
| 5. | Cohen G, Brodmerkel GJ, Lynn S. Absorbed doses to patients and personnel from endoscopic retrograde cholangiopancreatographic (ERCP) examinations. Radiology. 1979;130:773-775. [PubMed] |
| 6. | Heyd RL, Kopecky KK, Sherman S, Lehman GA, Stockberger SM. Radiation exposure to patients and personnel during interventional ERCP at a teaching institution. Gastrointest Endosc. 1996;44:287-292. [PubMed] |
| 7. | Chen MY, Van Swearingen FL, Mitchell R, Ott DJ. Radiation exposure during ERCP: effect of a protective shield. Gastrointest Endosc. 1996;43:1-5. [PubMed] |
| 8. | Brambilla M, Marano G, Dominietto M, Cotroneo AR, Carriero A. Patient radiation doses and references levels in interventional radiology. Radiol Med. 2004;107:408-418. [PubMed] |
| 9. | Pedrosa MC, Farraye FA, Shergill AK, Banerjee S, Desilets D, Diehl DL, Kaul V, Kwon RS, Mamula P, Rodriguez SA. Minimizing occupational hazards in endoscopy: personal protective equipment, radiation safety, and ergonomics. Gastrointest Endosc. 2010;72:227-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 10. | Hendee WR. Estimation of radiation risks. BEIR V and its significance for medicine. JAMA. 1992;268:620-624. [PubMed] |
| 11. | Kim E, McLoughlin M, Lam EC, Amar J, Byrne M, Telford J, Enns R. Prospective analysis of fluoroscopy duration during ERCP: critical determinants. Gastrointest Endosc. 2010;72:50-57. [PubMed] [DOI] [Full Text] |
| 12. | Campbell N, John V, Sparrow R, Ponich T. Radiation monitoring and protection during endoscopic retrograde choliangiopancreatography (ERCP): An ontario survey. Can J Gastroenterol. 2000;14:48 A. [PubMed] [DOI] [Full Text] |
| 13. | Tsalafoutas IA, Paraskeva KD, Yakoumakis EN, Vassilaki AE, Maniatis PN, Karagiannis JA, Koulentianos ED. Radiation doses to patients from endoscopic retrograde cholangiopancreatography examinations and image quality considerations. Radiat Prot Dosimetry. 2003;106:241-246. [PubMed] |
| 14. | Jorgensen JE, Rubenstein JH, Goodsitt MM, Elta GH. Radiation doses to ERCP patients are significantly lower with experienced endoscopists. Gastrointest Endosc. 2010;72:58-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Vehmas T. Hawthorne effect: shortening of fluoroscopy times during radiation measurement studies. Br J Radiol. 1997;70:1053-1055. [PubMed] |
| 16. | Johlin FC, Pelsang RE, Greenleaf M. Phantom study to determine radiation exposure to medical personnel involved in ERCP fluoroscopy and its reduction through equipment and behavior modifications. Am J Gastroenterol. 2002;97:893-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Martin CJ. A review of factors affecting patient doses for barium enemas and meals. Br J Radiol. 2004;77:864-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Uradomo LT, Goldberg EM, Darwin PE. Time-limited fluoroscopy to reduce radiation exposure during ERCP: a prospective randomized trial. Gastrointest Endosc. 2007;66:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Cohen MM, Duncan PG, Tate RB. Does anesthesia contribute to operative mortality? JAMA. 1988;260:2859-2863. [PubMed] |
| 20. | Ferreira LE, Baron TH. Comparison of safety and efficacy of ERCP performed with the patient in supine and prone positions. Gastrointest Endosc. 2008;67:1037-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Terruzzi V, Radaelli F, Meucci G, Minoli G. Is the supine position as safe and effective as the prone position for endoscopic retrograde cholangiopancreatography? A prospective randomized study. Endoscopy. 2005;37:1211-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Hoskins PR, Williams JR. Influence of radiologist grade on fluoroscopic patient dose. Br J Radiol. 1992;65:1119-1123. [PubMed] |
| 23. | Uradomo LT, Lustberg ME, Darwin PE. Effect of physician training on fluoroscopy time during ERCP. Dig Dis Sci. 2006;51:909-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Jowell PS, Baillie J, Branch MS, Affronti J, Browning CL, Bute BP. Quantitative assessment of procedural competence. A prospective study of training in endoscopic retrograde cholangiopancreatography. Ann Intern Med. 1996;125:983-989. [PubMed] |
| 25. | Lorenzo-Zúñiga V, Boix J, Oller B, Naves JE, Leal C, Añaños F, Moreno de Vega V. Variables predictivas de mayor dosis de irradiación en CPRE: Estudio prospectivo en 197 pacientes. Endoscopy. 2010;42:A23. [PubMed] |
| 26. | Naidu LS, Singhal S, Preece DE, Vohrah A, Loft DE. Radiation exposure to personnel performing endoscopic retrograde cholangiopancreatography. Postgrad Med J. 2005;81:660-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Tham TC, Vandervoort J, Wong RC, Montes H, Roston AD, Slivka A, Ferrari AP, Lichtenstein DR, Van Dam J, Nawfel RD. Safety of ERCP during pregnancy. Am J Gastroenterol. 2003;98:308-311. [PubMed] [DOI] [Full Text] |
| 28. | Samara ET, Stratakis J, Enele Melono JM, Mouzas IA, Perisinakis K, Damilakis J. Therapeutic ERCP and pregnancy: is the radiation risk for the conceptus trivial? Gastrointest Endosc. 2009;69:824-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 29. | Shelton J, Linder JD, Rivera-Alsina ME, Tarnasky PR. Commitment, confirmation, and clearance: new techniques for nonradiation ERCP during pregnancy (with videos). Gastrointest Endosc. 2008;67:364-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |