Published online Jun 16, 2010. doi: 10.4253/wjge.v2.i6.232
Revised: May 13, 2010
Accepted: May 20, 2010
Published online: June 16, 2010
Complications due to diagnostic colonoscopy are uncommon and acute appendicitis is a very rare complication of colonoscopy. This poses a diagnostic challenge as the presentation of appendicitis is similar to that of other complications of colonoscopy such as perforation or postpolypectomy syndrome. It is hypothesized that postcolonoscopy appendicitis might be associated with obstruction of the appendiceal lumen with fecal matter during colonoscopy. None of the previous reports in the literature have described findings of appendicitis after colonoscopy in a patient with active ulcerative colitis. We present a case of a 28 year-old man with active ulcerative colitis who underwent colonoscopy and subsequently developed acute appendicitis.
- Citation: Bachir NM, Feagins LA. Postcolonoscopy appendicitis in a patient with active ulcerative colitis. World J Gastrointest Endosc 2010; 2(6): 232-234
- URL: https://www.wjgnet.com/1948-5190/full/v2/i6/232.htm
- DOI: https://dx.doi.org/10.4253/wjge.v2.i6.232
We have recently seen an ulcerative colitis (UC) patient with acute appendicitis following colonoscopy. To our knowledge, only two cases of postcolonoscopy appendicitis have been reported in patients with UC and neither occurred while the patient had active colitis.
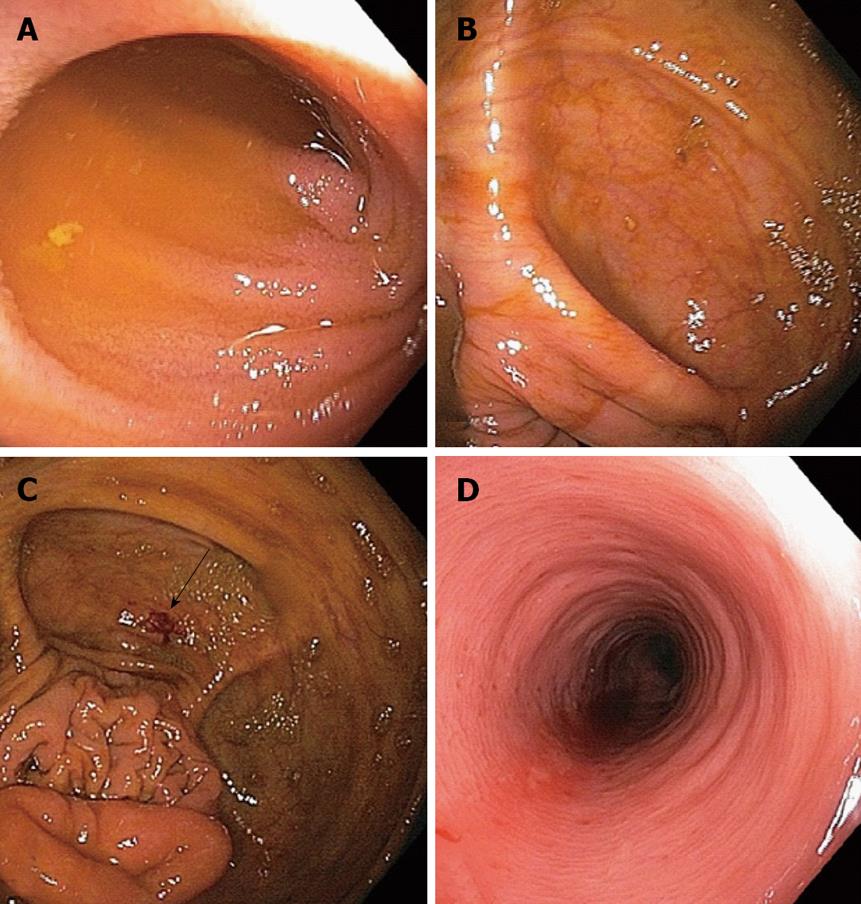
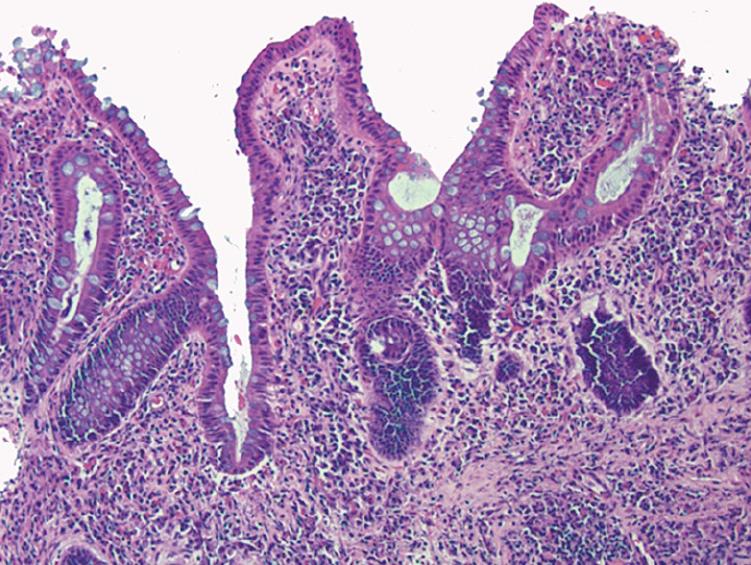
A 28 year-old man with an 8 year history of ulcerative colitis underwent colonoscopy for evaluation of his poorly controlled symptoms of colitis. He complained of 8-10 bowel movements a day with occasional blood and mucus, left lower quadrant abdominal pain, low-grade fevers and chills. The colonoscopy revealed diffuse, mild inflammation characterized by erythema, mild friability and loss of vascular pattern that extended from the rectum to the distal ascending colon. The procedure was uneventful without signs of inflammation in the cecum or around the appendiceal orifice. The terminal ileum was intubated easily and appeared normal (Figure 1). Biopsies were taken with jumbo forceps every 10 cm in 4 quadrants throughout the colon. Histological examination confirmed chronic active colitis in the left colon with normal mucosa in the right colon and terminal ileum (Figure 2).
Two days after the colonoscopy, the patient complained of new-onset fever and admitted to continued right lower quadrant abdominal pain since the colonoscopy. On examination he was found to have a blood pressure of 139/81, pulse of 105 and a temperature of 98.1oF. Abdominal examination was remarkable for diffuse tenderness to palpation, especially in the right and left lower quadrants, without rebound tenderness. The white blood cell count was 6 100 cells/mm3. An abdominal CT scan showed an appendix with a diameter of 9 mm and surrounding inflammatory changes consistent with early acute appendicitis. He was treated with antibiotics and underwent laparoscopy. Examination of the peritoneal cavity revealed no evidence of injury; areas of inflammation were noted only in the right lower quadrant. The appendix was removed and histological examination confirmed acute appendicitis without fecalith in the appendiceal lumen. The patient tolerated the procedure well and recovered without incident. He was discharged 1 d after the operation and treated with balsalazide and mesalamine enemas. On follow-up in the clinic the next week, he had improved with 1-2 bowel movements a day and no blood in his stool.
The pathogenesis of appendicitis starts with luminal obstruction, usually by fecal material, which causes a rise in intraluminal pressure that compromises blood flow and lymphatic drainage. This results in ischemia, inflammation, bacterial overgrowth and invasive infection. Other causes of appendiceal luminal obstruction include lymphoid hyperplasia, vegetable matter and fruit seeds, intestinal worms and tumors[1].
Iatrogenic causes of appendicitis include barium contrast examinations and colonoscopy. In the case of barium appendicitis, inspissated barium is considered to be the cause of obstruction[1-2]. In the case of postcolonoscopy appendicitis, it has been proposed that gas insufflation of the colon might force material in the lumen to lodge in and obstruct the appendix[3] or that trauma caused by the colonoscope or local intervention performed in or around the appendiceal orifice may cause intramural bleeding and edema that obstructs the appendiceal lumen[4]. In many of the published case reports however, overinsufflation during colonoscopy is not described and no obstructing lesion is identified in the resected appendix. In our patient, there was no obvious overinsufflation of the bowel or apparent trauma to the appendiceal orifice noted during colonoscopy and no fecal matter was found in the appendix on histopathology. Biopsies were taken in the cecum but in an area distant from the appendiceal orifice.
Our patient is the third of 20 reported cases of postcolonoscopy appendicitis that has been associated with ulcerative colitis. This observation raises the possibility that ulcerative colitis may be a risk factor for this phenomenon. Appendectomy has been proposed as a factor that protects against the development of ulcerative colitis[5-7]. However, in patients with established ulcerative colitis it is not clear whether inflammatory bowel disease influences the development of appendicitis[8]. Conceivably, ulcerative colitis might cause inflammation in the appendix that compromises its blood supply or lymphatic drainage, predisposing to postcolonoscopy appendicitis. Irrespective of the underlying mechanism, appendicitis is a rare but important complication of colonoscopy and should be included in the differential diagnosis for any patient who develops abdominal pain after the procedure. Postcolonoscopy appendicitis may be a particularly important consideration in patients with ulcerative colitis.
Peer reviewer: Oscar Tatsuya Teramoto-Matsubara, MedCenter, Av. Paseo de las Palmas 745-102, Lomas de Chapultepec, México D.F. 11000, México
| 1. | Prystowsky JB, Pugh CM, Nagle AP. Current problems in surgery. Appendicitis. Curr Probl Surg. 2005;42:688-742. |
| 2. | Sisley JF, Wagner CW. Barium appendicitis. South Med J. 1982;75:498-499. |
| 3. | Horimatsu T, Fu KI, Sano Y, Yano T, Saito Y, Matsuda T, Fujimori T, Yoshida S. Acute appendicitis as a rare complication after endoscopic mucosal resection. Dig Dis Sci. 2007;52:1741-1744. |
| 4. | Izzedine H, Thauvin H, Maisel A, Bourry E, Deschamps A. Post-colonoscopy appendicitis: case report and review of the literature. Am J Gastroenterol. 2005;100:2815-2817. |
| 5. | Andersson RE, Olaison G, Tysk C, Ekbom A. Appendectomy and protection against ulcerative colitis. N Engl J Med. 2001;344:808-814. |
| 6. | Frisch M, Pedersen BV, Andersson RE. Appendicitis, mesenteric lymphadenitis, and subsequent risk of ulcerative colitis: cohort studies in Sweden and Denmark. BMJ. 2009;338:b716. |
| 7. | Koutroubakis IE, Vlachonikolis IG, Kouroumalis EA. Role of appendicitis and appendectomy in the pathogenesis of ulcerative colitis: a critical review. Inflamm Bowel Dis. 2002;8:277-286. |
| 8. | Frisch M, Biggar RJ. Appendectomy and protection against ulcerative colitis. N Engl J Med. 2001;345:222-223; author reply 223-234. |