Published online Aug 16, 2025. doi: 10.4253/wjge.v17.i8.111141
Revised: July 8, 2025
Accepted: August 4, 2025
Published online: August 16, 2025
Processing time: 52 Days and 14 Hours
Post-endoscopic retrograde cholangiopancreatography (ERCP) bleeding is a se
We present a case of a 55-year-old male patient who developed post-ERCP hemo
Post-ERCP bleeding can result from various etiologies, and the rupture of variant vessels is a noteworthy topic warranting further exploration.
Core Tip: This case report describes a 55-year-old male patient who experienced post-endoscopic retrograde cholangiopancreatography (ERCP) hemorrhage one month after undergoing ERCP, endoscopic sphincterotomy, and bile duct stone removal for acute biliary pancreatitis. The patient presented with upper abdominal pain and melena, and imaging studies revealed high-density shadows suggestive of bleeding. Emergency interventional embolization and subsequent endoscopic and interventional therapies were successful in controlling the bleeding, highlighting the importance of recognizing and managing various etiologies of post-ERCP bleeding, including the rupture of variant vessels.
- Citation: Ma ZW, Gong XJ, Chen YJ, Wang B. Vascular anomaly as a cause of late bleeding after endoscopic retrograde cholangiopancreatography: A case report. World J Gastrointest Endosc 2025; 17(8): 111141
- URL: https://www.wjgnet.com/1948-5190/full/v17/i8/111141.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i8.111141
We present a case of a 55-year-old male patient who developed post-endoscopic retrograde cholangiopancreatography (ERCP) hemorrhage one month after undergoing ERCP, endoscopic sphincterotomy (EST), and bile duct stone removal for acute biliary pancreatitis. The patient presented with upper abdominal pain and melena, and imaging studies revealed high-density shadows in the intrahepatic bile duct, gallbladder, and lower segment of the common bile duct, suggestive of bleeding. Emergency interventional embolization was performed, and subsequent endoscopic and interventional therapies were implemented to control the bleeding. The patient’s hemoglobin levels gradually improved, and biliary indicators normalized. Similarly, other related case reports have described various bleeding events following ERCP, including injury to the right gastroepiploic artery[1], bleeding from biliary varices[2], retroperitoneal hematoma in liver transplant recipients[3] and subcapsular liver hematoma after ERCP (Table 1)[4]. Overall, this case highlights the challenges of managing post-ERCP hemorrhage, particularly in the context of vascular variations, and underscores the importance of a multidisciplinary approach to treatment.
| Ref. | Year | Outcome | Management |
| Risher and Smith[1] | 1990 | Injury the gastroepiploic artery | Ligate the right gastroepiploic artery |
| Tighe and Jacobson[2] | 1996 | Bile duct varices | Ligate the bile duct varices |
| Cárdenas et al[3] | 2008 | Subcapsular hepatic hematoma | Place the biliary plastic stent |
| Zizzo et al[4] | 2015 | Subcapsular hepatic hematoma | Embolization the right hepatic artery |
A 55-year-old male patient was admitted to an external hospital for “acute biliary pancreatitis” and underwent ERCP, EST, and bile duct stone extraction. One month of post-procedure, the patient presented with sudden upper abdominal pain and melena, leading to his admission to our hospital. Emergency whole-abdomen computed tomography (CT) revealed high-density shadows in the intrahepatic bile ducts, gallbladder, and lower common bile duct, suggesting possible hemorrhage.
The patient presented with abdominal pain and hematochezia two days ago without any apparent precipitating factors. There were no accompanying symptoms such as nausea, vomiting, dizziness, headache, chest tightness, or palpitations. The patient received symptomatic treatment at a local hospital, but the details of the treatment are unclear, and the symptoms did not improve. The patient was referred to our hospital for further evaluation and management and was admitted to our department with a diagnosis of gastrointestinal bleeding.
On October 18, 2023, the patient was diagnosed with acute biliary pancreatitis and underwent “ERCP + EST + bile duct stone extraction” at an outside hospital. The specific details of the procedure are not available.
The patient has no significant past medical history and denies a history of hypertension or diabetes. The patient also denies a history of infectious diseases such as hepatitis B or tuberculosis. There is no family history of genetic disorders.
There was mild tenderness in the right upper quadrant without rebound tenderness. Bowel sounds were hyperactive.
Blood tests showed: (1) Hemoglobin: 51.0 g/L (normal range: 130.0-175.0 g/L); (2) Total bilirubin: 136.3 μmol/L; (3) Direct bilirubin: 129.1 μmol/L; and (4) Transaminase: 91 U/L.
Emergency whole-abdomen CT revealed high-density shadows in the intrahepatic bile ducts, gallbladder, and lower common bile duct, suggesting possible hemorrhage.
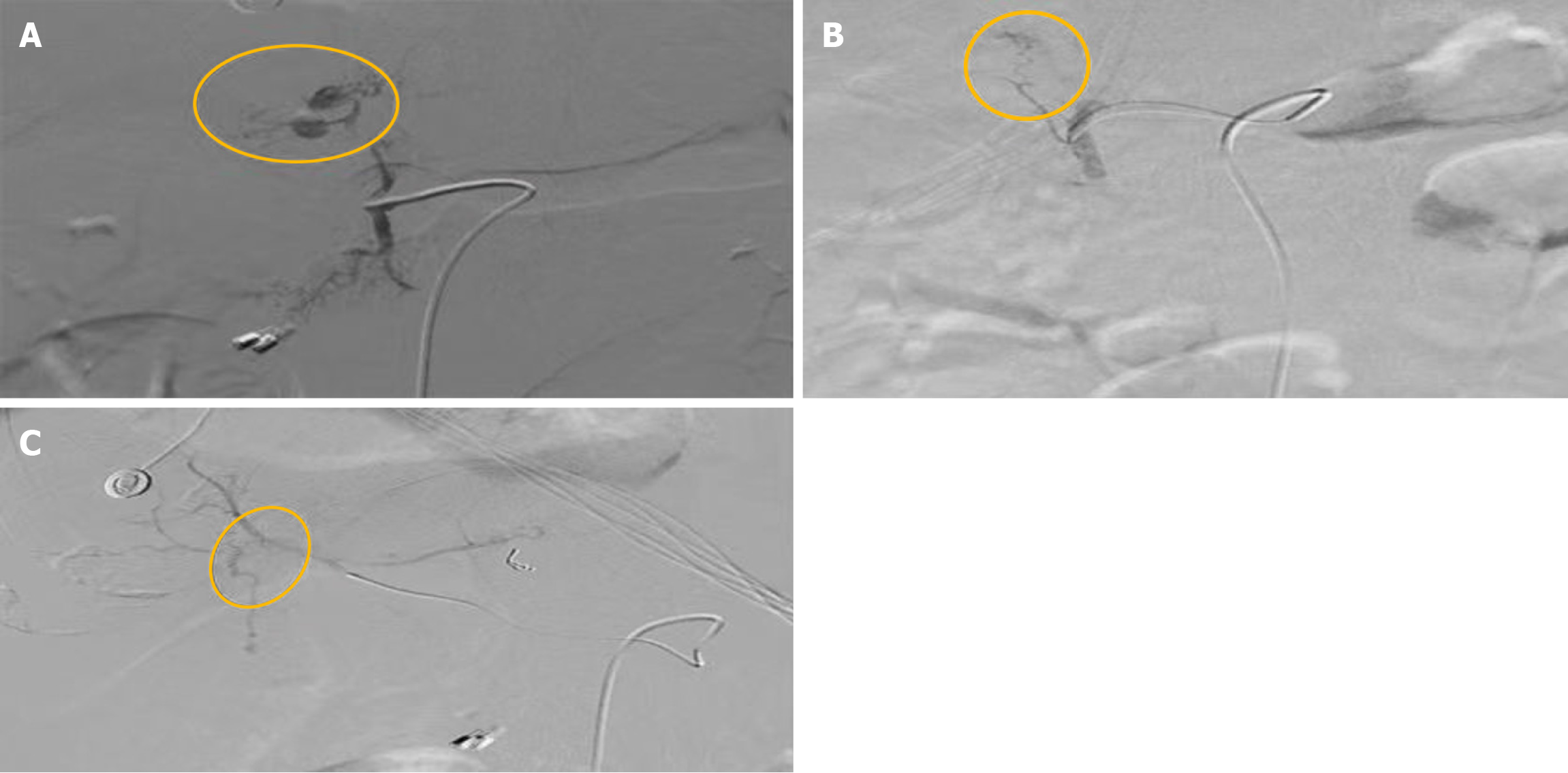
Hemorrhage from the right hepatic artery (Figures 1 and 2).
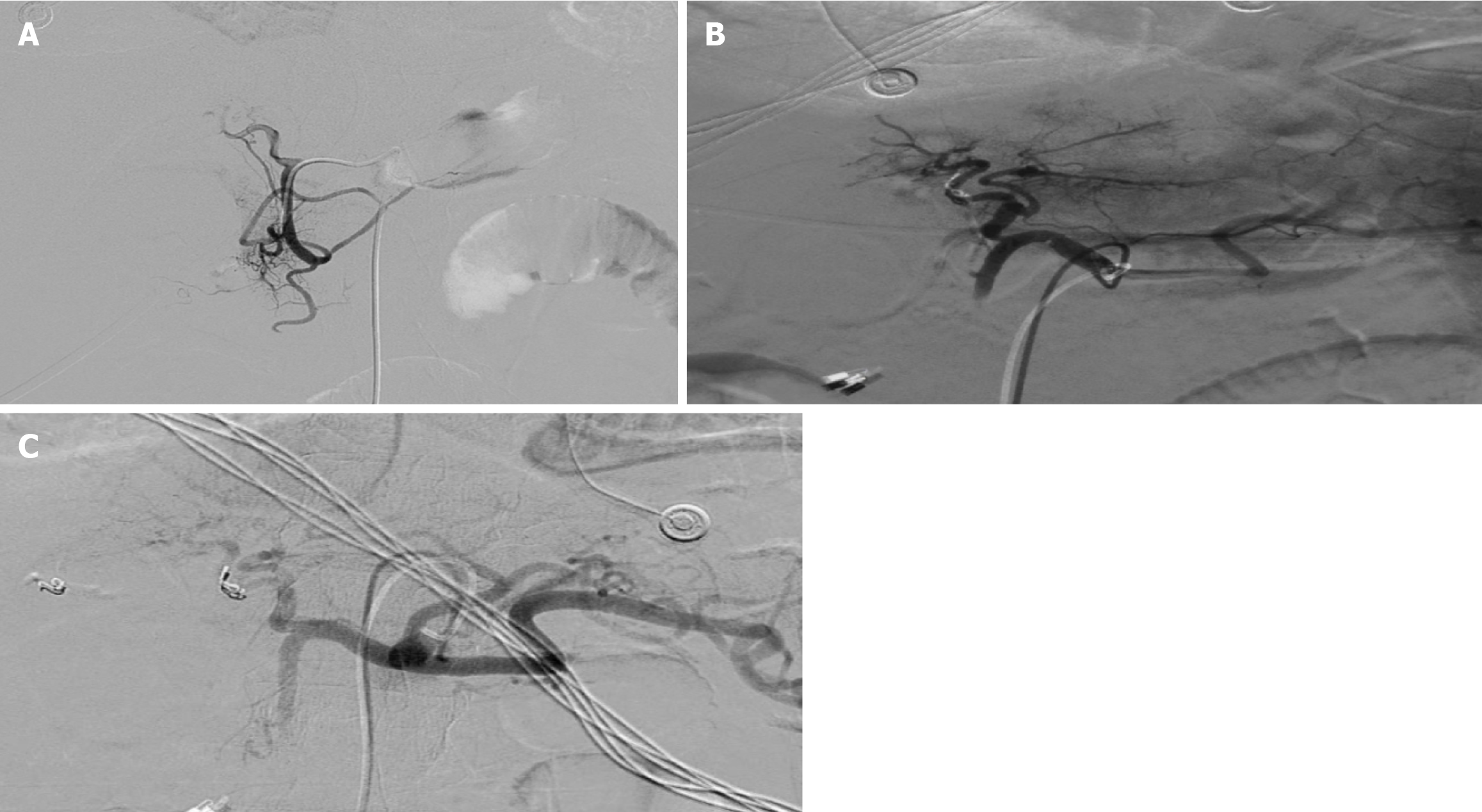
Embolic occlusion of a small branch of the right hepatic artery was performed (Figures 3 and 4).
The patient’s hemoglobin levels showed an upward trend, and his biliary indices gradually returned to normal. His abdominal pain improved, and he recovered well.
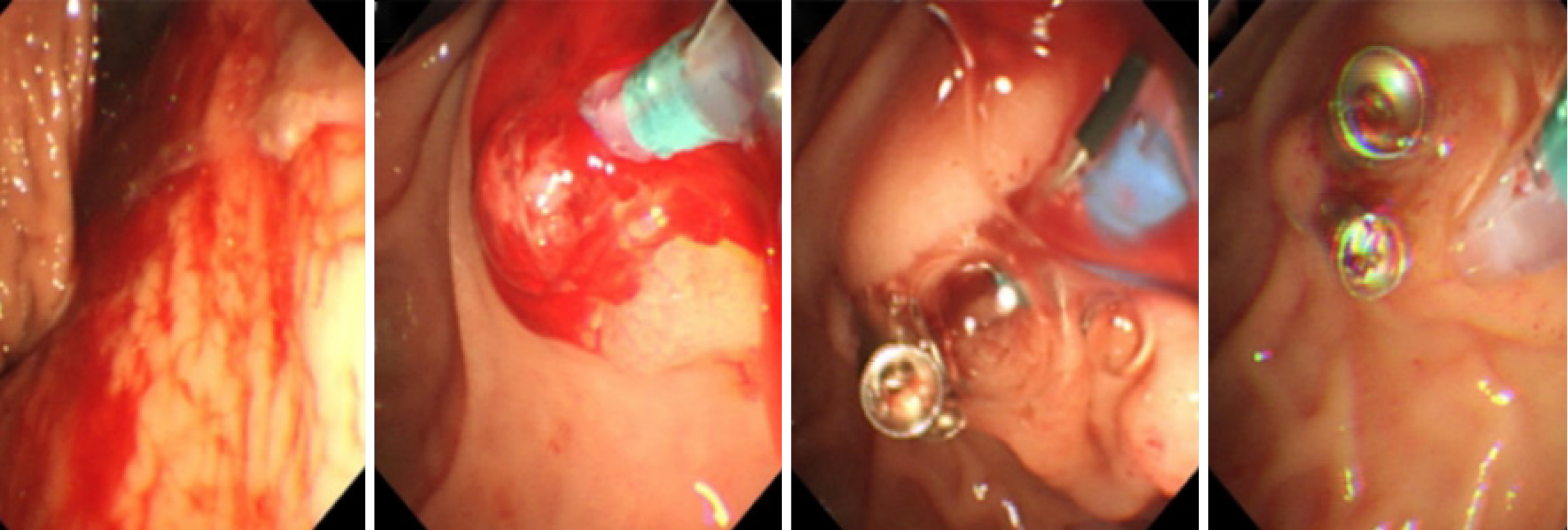
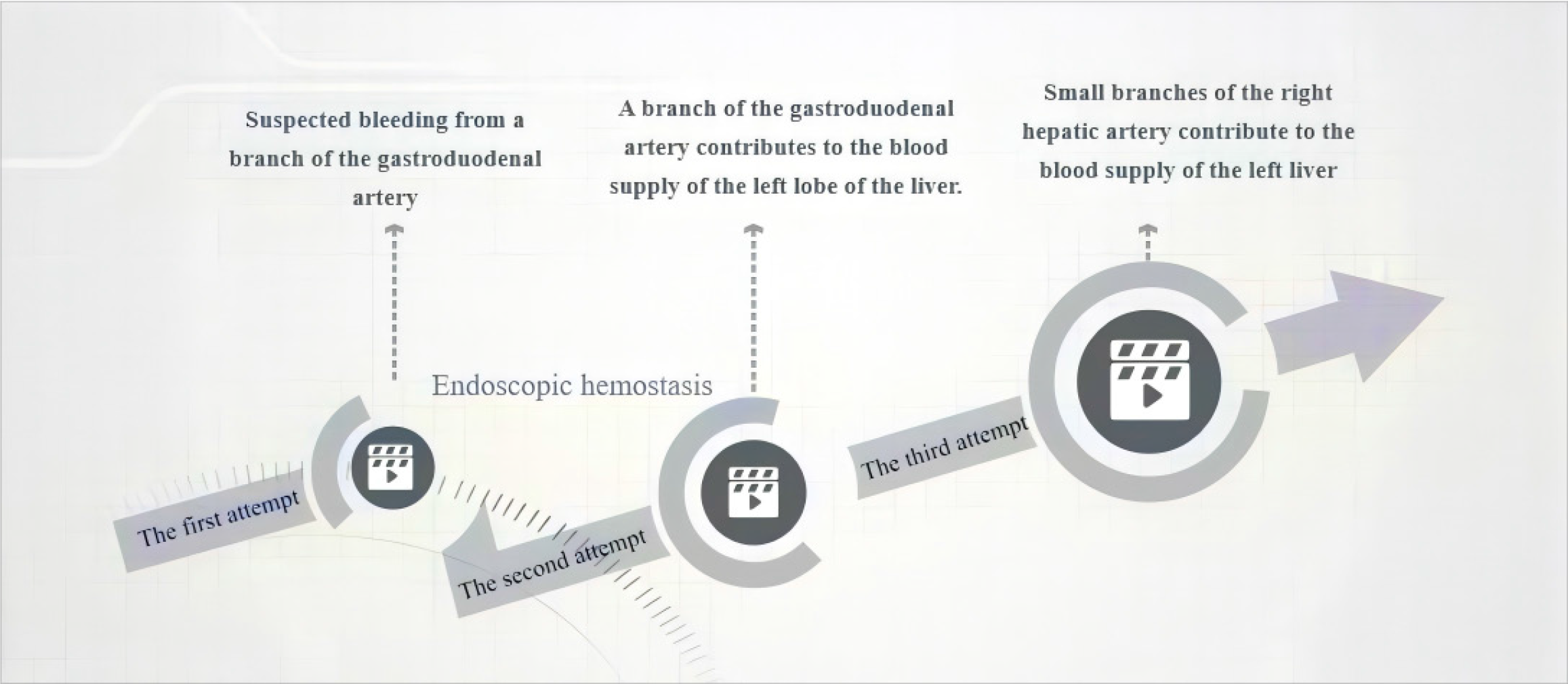
In this case, the patient experienced significant gastrointestinal bleeding one month of post-ERCP, which was successfully managed through three interventional treatments and one endoscopic hemostasis. The most likely cause of the bleeding from the variant vessel was related to the surgical procedure and local inflammatory response.
Accurate identification of the cause of post-ERCP hemorrhage is essential for precise treatment. In decision-making, it is crucial to consider multiple potential causes of bleeding rather than adhering to a single hypothesis.
| 1. | Risher WH, Smith JW. Intraperitoneal hemorrhage from injury to the gastroepiploic artery: a complication of endoscopic retrograde sphincterotomy. Gastrointest Endosc. 1990;36:426-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Tighe M, Jacobson I. Bleeding from bile duct varices: an unexpected hazard during therapeutic ERCP. Gastrointest Endosc. 1996;43:250-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Cárdenas A, Crespo G, Balderramo D, Bordas JP, Sendino O, Llach J. Subcapsular liver hematoma after Endoscopic Retrograde Cholangiopancreatography in a liver transplant recipient. Ann Hepatol. 2008;7:386-388. [PubMed] |
| 4. | Zizzo M, Lanaia A, Barbieri I, Zaghi C, Bonilauri S. Subcapsular Hepatic Hematoma After Endoscopic Retrograde Cholangiopancreatography: A Case Report and Review of Literature. Medicine (Baltimore). 2015;94:e1041. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |