Published online Aug 16, 2025. doi: 10.4253/wjge.v17.i8.107458
Revised: April 23, 2025
Accepted: June 17, 2025
Published online: August 16, 2025
Processing time: 142 Days and 3.7 Hours
Endoscopic ultrasound (EUS) is an indispensable tool for the diagnosis and management of various diseases, particularly biliopancreatic disorders, as it provides detailed visualization of the gastrointestinal tract and surrounding structures. As the demand for diagnostic and interventional EUS procedures increases, ensuring high-quality training for endoscopists is essential to improve patient outcomes. This mini-review provides an overview of the current state of EUS training and emphasizes the importance of a structured approach that integrates theoretical knowledge and hands-on experience. We discuss different training methods, focusing on the main courses available worldwide, and highlight their advantages and limitations. In addition, we examine the challenges of training for diagnostic and interventional EUS, such as limited access to training centers and the need for personalized feedback. Overall, improving EUS training programs is essential to enhance physician skills and ensure this advan
Core Tip: This article discusses various endoscopic ultrasound training methods, focusing on the main courses available worldwide and highlighting their advantages and limitations. This mini-review provides an overview of the current state of endoscopic ultrasound training and emphasizes the importance of a structured approach that integrates both theoretical knowledge and hands-on experience.
- Citation: Delsa H, Khannoussi W, Ghoneem E, Okasha HH. Endoscopic ultrasound training: Current state, challenges, and the path to proficiency. World J Gastrointest Endosc 2025; 17(8): 107458
- URL: https://www.wjgnet.com/1948-5190/full/v17/i8/107458.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i8.107458
Endoscopic ultrasound (EUS) is vital in diagnosing and managing various diseases, particularly biliopancreatic disorders. Compared to gastrointestinal (GI) endoscopy, EUS provides detailed visualization of the structures surrounding the GI tract. Many endoscopy centers worldwide are equipped with EUS, highlighting the need for specialized training. Over the past four decades, several EUS training programs have been developed, incorporating various models including simulators, phantoms, ex vivo models, and live animal models[1].
This mini-review provides an overview of the current state of EUS training and emphasizes the importance of a structured approach, integrating theoretical knowledge and hands-on experience. Different training methods are discussed, focusing on the main courses available worldwide, and their advantages and limitations. The challenges associated with training in diagnostic and interventional EUS, such as limited access to training centers and the need for personalized feedback, are examined.
Introduced in the early 1980s by American, German, and Japanese teams, EUS has since been used worldwide for investigating challenging cases where radiology is ineffective, particularly in pancreatic pathology[2]. EUS requires specialized training under expert supervision, and various societies have adopted EUS training guidelines in many countries.
In 2001, the American Society for Gastrointestinal Endoscopy (ASGE) initially proposed a minimum of 190 supervised EUS procedures, including at least 75 pancreaticobiliary lesions, 75 mucosal tumors, and 40 subepithelial abnormalities. However, in 2017, ASGE increased the required number of EUS procedures to 225[3,4]. More recently, the European Society of Gastrointestinal Endoscopy (ESGE), and the United Kingdom and Ireland Joint Advisory Group recommended that trainees complete a minimum of 250 supervised EUS procedures, including 80 luminal tumors, 20 submucosal lesions, and 150 pancreatobiliary lesions, at least half of which are likely pancreatic adenocarcinomas[5-7]. This training should be conducted by high-volume centers over a minimum of 12 months to ensure adequate experience in diagnostic EUS[5,8].
Once basic skills are acquired, including safe scope handling, and identifying basic anatomy and common pathology, trainees should initiate EUS fine needle aspiration or biopsy (FNA/FNB). ESGE and ASGE recommend 50 EUS-FNA/FNB cases, including 25 to 30 pancreatic lesions[4,5].
In the early 2000s, numerous other interventional devices were developed, leading to the integration of EUS and ERCP in select centers between 2007 and 2010. Over time, EUS has evolved to include increasingly complex interventional procedures, particularly for pancreatobiliary lesions, such as tumor ablation, biliary drainage (BD), and anastomoses[9].
EUS is one of the most technically challenging endoscopic procedures and must be performed by skilled endoscopists trained in ultrasound imaging reconstruction and interpretation. In recent years, the development of EUS training in expert centers has become essential, progressing from diagnostic EUS to basic and advanced therapeutic EUS. One of the most effective ways to learn EUS follows Miller's four-layered pyramid for competency acquisition: "Knows", "Knows how", "Shows how", and "Does". An ideal training program should incorporate both theoretical knowledge and practical procedures using simulators, models, and real patients[9,10].
Regarding theoretical knowledge, endoscopists must develop a strong understanding of the anatomy and pathology of the pancreas, gastrointestinal and biliary tracts, and adjacent organs. Various modalities, such as simulation models and virtual reality, can enhance learning[11,12]. By engaging with digital resources, live endoscopy courses, and conferences, trainees should familiarize themselves with EUS techniques and devices[6]. Since coronavirus disease 2019, numerous online courses have been introduced to address training disruptions, including the virtual EUS training course developed by Dhir et al[13], which enrolled 21 trainees over 3 months and focused on EUS anatomy. The success of this course confirmed the feasibility and effectiveness of virtual EUS training.
Several models have been developed to facilitate training outside the clinical setting to minimize the risk of complications, including computer-based simulators, phantoms, ex vivo animal models, and live animal models[1].
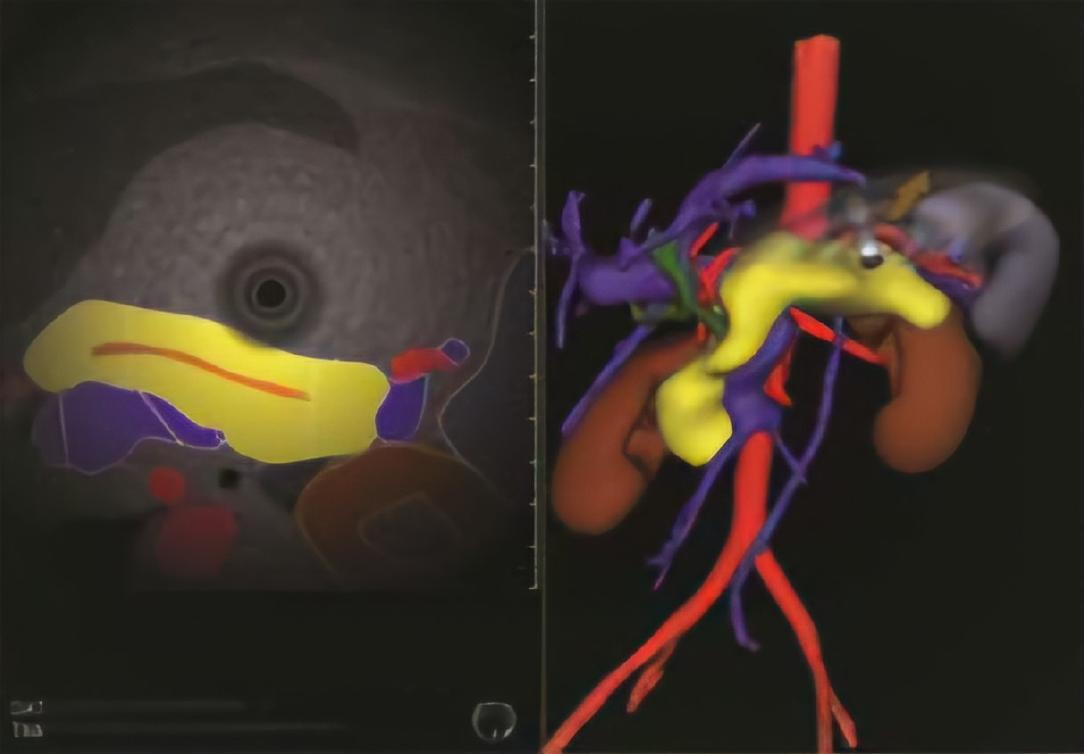
Computer-based simulators: Endoscopy simulators were designed to replicate real-life scenarios for training, initially for GI endoscopy, with EUS modules later added. Based on human anatomy, these simulators provide a realistic, real-time linear or radial ultrasound display with split-screen EUS/three-dimensional (3D) mapping, such as the GI Mentor (Figure 1)[1,14]. Utilizing real cadaver anatomy, EUS meets VOXEL-MAN, and Endo-X has been developed for linear array EUS training[15,16]. These simulators enable trainees to learn proper scope maneuvering and the identification of key EUS landmarks.
Phantoms: Over the past 40 years, training phantoms have been developed for ultrasound and ERCP to support diagnostic and interventional procedures, such as biopsies and drainage. To facilitate hands-on EUS courses, Olympus created EUS phantoms containing tubes and various types and sizes of silicone blocks that simulate different scenarios, including cystic lesions and lymph nodes. These phantoms are easy to use, cost-effective, reusable, and suitable for basic and interventional EUS training. However, their preparation requires more time and a short preservation period of less than 3 weeks[17,18].
Ex vivo animal models: Ex vivo animal simulation models were developed using plastic materials combined with animal organs. The first ex vivo model for therapeutic endoscopy, the Erlangen Active Simulator for Interventional Endoscopy (EASIE), was introduced in 1997. It comprises a human-shaped mannequin with an anatomical torso[19-21]. EASIE models provide a more realistic experience than computer-based simulators but require adaptation for ultrasound imaging, such as the EUS RK model, which incorporates materials like gelatin and silicone. These models are widely used in EUS training courses worldwide[22-25].
The Mumbai EUS II 3D hybrid model was developed using a pig stomach with a molded rubber duodenum and bile duct. This model provides excellent training for various EUS-guided biliary drainage procedures when combined with step-by-step learning[26].
Another hybrid model, the Magic Box, was designed to offer hands-on training in multiple interventional EUS procedures, including choledochoduodenostomy, hepaticogastrostomy, hepaticoenterostomy, and gastro-enteric anastomosis. This model incorporates a porcine esophagus and stomach, a silicone duodenal and pancreatobiliary system, biopsy targets, and a pseudocyst[27].
In 2016, the Thai Association of Gastrointestinal Endoscopy (TAGE) developed an EUS gelatin-starch model for local workshops in Thailand. However, this model required refrigeration, lacked durability, and was costly. To address these issues, the TAGE introduced the TAGE 2 model in 2018, which is more durable, easier to reshape, and has been widely adopted in Southeast Asia, particularly for interventional EUS training[12,28].
With advancements in therapeutic EUS and the development of multiple procedures, including EUS-FNA/FNB, BD, pseudocyst drainage, pancreatic duct drainage, and, more recently, gastro-enterostomy, the need for a comprehensive training tool has emerged. Consequently, the EUS Magic Box was developed to facilitate various EUS procedures. Building on prior experience with other models, this hybrid model combines synthetic components (a synthetic duodenum and pancreatobiliary tree) with porcine tissues (a disinfected terminal esophagus and pig stomach). Additionally, multiple pieces of liver tissue or a pig urinary bladder filled with gelatin can be embedded in the box[27].
Live animal models: The most realistic EUS simulators are live animal models, particularly pigs, due to their anatomical similarities to humans. However, differences exist in the thickness and orientation of various organs[29-31]. These models suit beginners who want to learn scope manipulation and biopsy techniques. However, they require specialized labo
By utilizing these training tools, trainees can enhance their skills in guidewire manipulation, needle puncture, and stent deployment, enabling them to perform interventional EUS procedures. Marc Giovannini proposed a stepwise approach to learning interventional EUS, beginning with the drainage of pancreatic collections using a cystostome and double pigtail stents, followed by cholecystoduodenostomy, choledochoduodenostomy, hepaticogastrostomy, and finally gastro-enterostomy, with a minimum number of procedures required for each (Table 1)[12,32].
| Name of procedure | Number of supervised procedures required |
| Pancreatic fluid collection drainage | 20-30 |
| Cholecystoduodenostomy | 19 |
| Choledocoduodenostomy | 32 (mastery after 100) |
| Hepaticogastrostomy | 33 |
| Pancreatic duct drainage | 27 |
| Gastro-enteric anastomosis | 25 (mastery after 40) |
Many EUS courses have been organized worldwide by various societies. Despite the increasing demand for formal EUS fellowships, such programs are available in only a few countries. However, numerous certified training courses are offered. Below, we overview some of the most significant programs across different continents.
One of the most well-structured EUS training programs is the EUS diploma in France, operated by the Club Francophone d’Écho-endoscopie in collaboration with the French Society of Digestive Endoscopy. Established in 1993 and initially based in Paris, this 2-year program includes 4 weeks of theoretical coursework and 20 1-day practical sessions held annually at three centers in Marseille. The teaching faculty consists primarily of EUS experts, as well as anatomists, radiologists, surgeons, and pathologists. Practical sessions include 1 day with a swine model and 4 days of training on computer-based simulators and live demonstrations. The final examination comprises four written questions and an analysis of EUS videos[2,33].
In 2000, an evaluation of the French EUS diploma included 57 participants from 147 trainees enrolled between 1995 and 1999. The study revealed that trainees valued theoretical and practical sessions, although they requested additional video sessions and simulator training. Nearly 78% of graduates continued practicing EUS after earning the diploma, and most participants recommended the course. Consequently, since 2004, the program has been revised to include 3 weeks of theoretical instruction with multiple video sessions and 1 week of practical training. Additionally, more videos and images have been incorporated into the lectures. Trainees must be Francophone, have at least 2 years of experience, and have access to EUS equipment. The introduction of interventional EUS training on live pigs allowed participants to practice EUS-FNA/FNB, guidewire manipulation, and celiac neurolysis[34]. Since coronavirus disease, online courses have been introduced, supplemented by 1 week of in-person practice. To date, this diploma is not mandatory in France for practicing EUS.
The Mohammed VI International Simulation Center for Sciences and Health (CIM6SS) and the Mohammed VI University of Sciences and Health in Casablanca offer the Digestive EUS University Diploma, a structured and comprehensive EUS training program designed to teach the fundamentals of diagnostic EUS and FNB. It is the first EUS university diploma established in Morocco. The training is conducted at CIM6SS, affiliated with the Mohammed VI Foundation for Sciences and Health, a fully equipped center for endoscopic training across all endoscopy specialties.
The program is overseen by an organizing committee comprising a course director, an EUS expert with over 10 years of experience in clinical practice and university-level teaching, and two young professors and senior endoscopists nearing completion of their EUS training. Additionally, the faculty includes at least three international experts with extensive experience in both diagnostic and interventional EUS.
The course is designed for endoscopists proficient in upper and lower GI endoscopy, particularly those new to EUS. The curriculum consists of four thematic modules, each scheduled two months apart. The first module focuses on normal echoanatomy of the upper GI tract, including the pancreatobiliary system and the lower GI tract, providing the foundational knowledge necessary for diagnostic competency. The second module covers upper and lower digestive tract diseases, while the third addresses pancreatobiliary diseases. The final module explores liver, mediastinal, and other organ pathologies and includes hands-on training in EUS-guided FNA/FNB (Table 2).
| Session | Number of days | Program | |
| First session | 3 | Normal echo-anatomy | 30% hands-on |
| Second session | 3 | Upper and lower GI tract diseases | 50% hands-on |
| Third session | 3 | Pancreatobiliary diseases | 50% hands-on |
| Fourth session | 3 | Liver and other organs/FNA-FNB | 70% hands-on |
| Final assessment | 1 | Attendance > 80%, portfolio > 50 cases > 4 weeks training with expert, video cases quiz, cases presentation | |
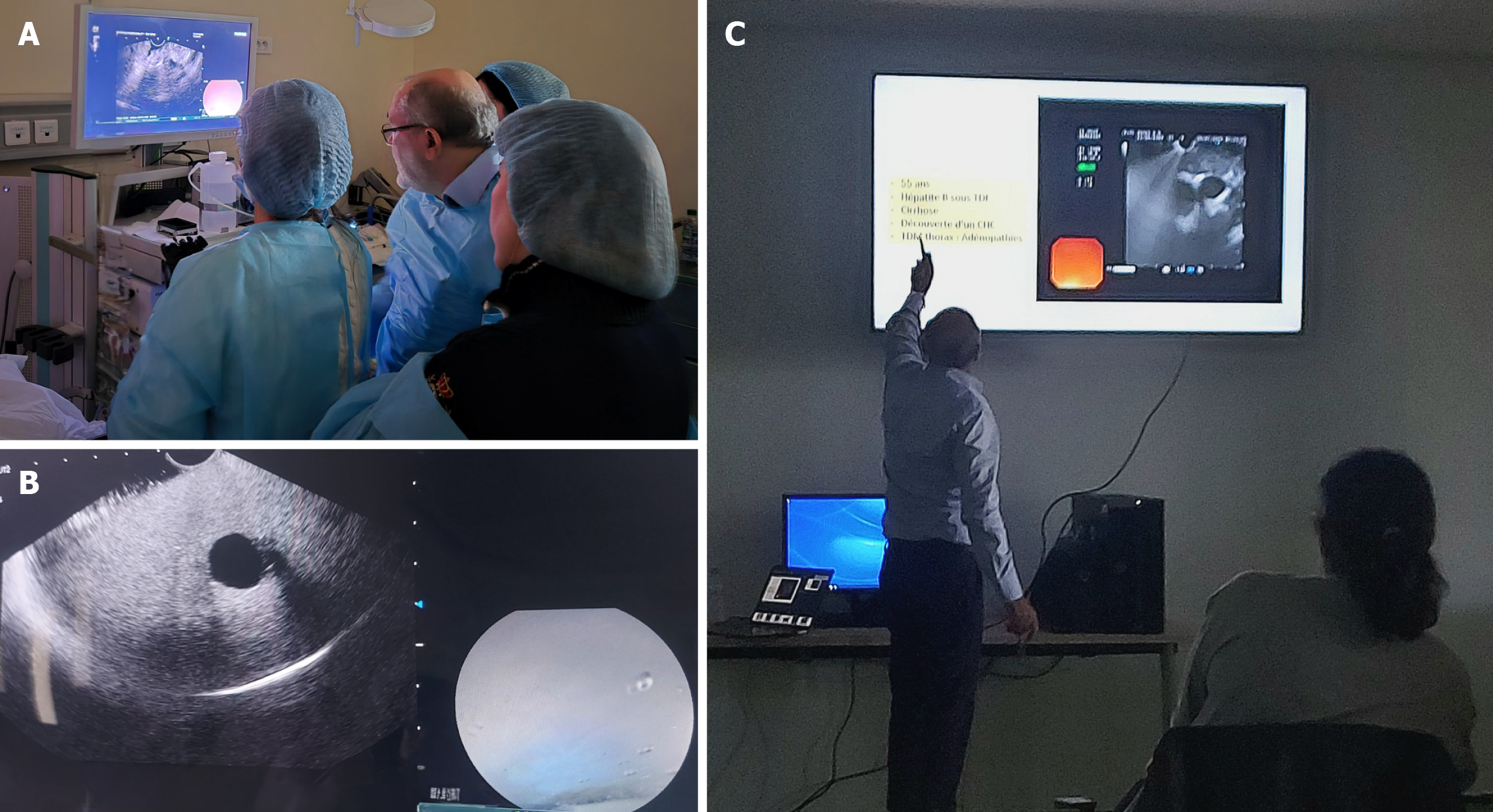
Each module spans 3 days and incorporates various educational methods, including lectures, video case discussions, quizzes, hands-on training using simulators, synthetic and animal models, and live demonstrations in endoscopy rooms. Participants observe cases and perform EUS examinations under expert supervision. The CIM6SS team has developed its own phantom models for initial EUS scope handling and adapted them for FNA/FNB training. Live case training occurs in two international university hospitals in Casablanca, where diagnostic and therapeutic EUS procedures are performed (Figure 2).
Assessment is based on five criteria: (1) At least 80% attendance; (2) A portfolio of over 50 cases attended or performed under expert supervision; (3) A video case quiz; (4) Case presentations; and (5) 4 weeks training in expert center. By the end of the training, participants are expected to independently identify key anatomical landmarks following ESGE quality criteria for diagnostic EUS, accurately exclude common bile duct stones, and perform FNB on pancreatic masses with low technical difficulty. Participants are monitored for 1-year post-training to evaluate their practice and adherence to quality standards.
The number of participants is limited to ensure an optimal learning experience, fostering small-group discussions and hands-on accessibility. The first cohort included 14 participants from diverse practice backgrounds. Selection criteria focus on endoscopic experience, access to a mentor at the participant’s institution, and the availability of an EUS scope during or immediately after training. Age, sex, and country of origin are not limiting factors. The course is conducted in both French and English.
The national and international faculty members have extensive experience in EUS practice and education, distinguished by their patience and passion for the field. All experts have committed to providing training periods for participants to fulfil the course's required 4-week expert center experience.
Course quality, content, and organization are continuously evaluated using participant and expert feedback collected through questionnaires. Adjustments and improvements are implemented based on these responses for subsequent sessions.
In 2018, the World Endoscopy Organization (WEO) launched the first WEO international school of EUS (WISE) in collaboration with the Asian EUS Group Korea. This initiative aimed to provide comprehensive EUS training to a select group of young endoscopists (10 doctors aged 30-45) over 1 year. The curriculum combined theoretical and practical training, including online lectures, web conferences, live case presentations, and hands-on sessions using live pigs and phantoms[35].
Under the leadership of course founder and director Professor Dong-Wan Seo, WISE trainees received structured education covering both fundamental EUS anatomy and advanced techniques. Over the years, the program has expanded, involving more participants and additional training modules
The WISE–Egyptian Chapter was established in 2022 as a hands-on training program to teach the fundamental anatomy and techniques of diagnostic linear EUS. Inspired by the original WISE program, founded by Professor Dong-Wan Seo in 2018, this initiative was co-directed by Dr. Elsayed Ghoneem from Mansoura University (Mansoura, Egypt), who graduated from WISE in 2020. The program was a comprehensive three-module course to equip participants with essential skills and knowledge to master diagnostic linear EUS. Under the guidance of national and international experts, trainees gained extensive practical experience and a deeper understanding of EUS techniques.
The first cohort graduated in 2023, with 12 trainees from North Africa and the Middle East completing the program, marking a significant milestone in advancing EUS expertise in the Arab region. Building on this success, the WISE Egyptian Chapter launched a second course in 2024, further strengthening EUS training in the region. This session witnessed the graduation of 15 participants, reflecting a growing commitment to enhancing EUS expertise in North Africa and Arab countries. The program's hands-on nature and expert-led instruction played a pivotal role in developing the participants' technical skills and confidence.
Each course comprised several modules, with each module spanning 4 to 5 days. The training structure was designed to optimize learning through didactic lectures in the morning and hands-on training in the afternoon. During practical sessions, trainees were divided into three operating rooms, where they initially observed live cases with expert demonstrations before engaging in supervised hands-on practice. The training began with EUS evaluation of the gastric station and mediastinum, progressing to withdrawing the scope while examining structures from the duodenal bulb, followed by scope introduction into the duodenum and, ultimately, tissue acquisition techniques.
A total of 92 cases were included during the first course, while the second course expanded to 120 cases, supported by the involvement of multiple tertiary centers. Participant evaluation was conducted at the beginning, during, and end of the training, following a structured EUS assessment protocol based on the Educational Program of Kindai system[36].
The continued success of the WISE Egyptian Chapter underscores the increasing recognition of EUS as a critical diagnostic and interventional tool. Moreover, it highlights the program’s essential role in advancing EUS education at national and international levels, fostering a new generation of skilled endosonographers dedicated to improving patient care.
UC Louvain University in Brussels offers a certificate in Digestive Endosonography, comprising over 80 hours of training. This includes 40 hours of theoretical education with video sessions and 32 hours of hands-on teaching.
Numerous EUS meetings are held across Europe, such as the Euro EUS Live course, which is typically organized in France and Italy. Additionally, various workshops and congresses are conducted by national clubs, committees, and interest groups in the field of EUS, including the Middle East and Africa EUS Group of Interest, the Turkish EUS Group of Interest, and the United Kingdom EUS Users Group[2].
In 2003, a panel of European experts from Belgium, France, Spain, and Italy established the European Group for Endoscopic Ultrasound (EGEUS), an international EUS working group aimed at uniting the expertise, skills, and innovation of various European EUS societies. Today, with over 1000 regular members from nearly 35 countries, EGEUS is the largest group of endosonographers worldwide. To promote EUS education, EGEUS organizes a European EUS Congress every 2 years and has developed a website and app featuring an extensive library and networking opportunities for the entire EGEUS community. Furthermore, EGEUS collaborates with the ESGE, organizing an EGEUS-ESGE session at ESGE Days since 2018[37].
Similarly, in 2012, the Asian EUS Group (AEG) was founded to advance EUS education in Asia. Since its inception, AEG has organized over 60 EUS teaching programs, training thousands of endoscopists across various Asian regions. Additionally, the group offers specialized "train-the-trainer" courses to enhance instructional capabilities[38].
The EUS Confluence Days organised by the ROEYA Training Centre and EUS-ENDO under the direction of Dr. Marc Giovannini are other important EUS meetings with hands-on training and lectures on the latest advanced EUS techniques.
In 2024, the IHU Strasbourg proposed a unique 3-day course, the International Therapeutic EUS course. It includes 14 hours of Hands-on training with simulated models by international experts.
The primary challenge in EUS training is the establishment of structured, integrated diplomas, fellowships, or long-term courses consisting of multiple modules over several months or years to ensure trainees achieve independent proficiency in performing EUS procedures on real patients. These comprehensive training programs should encompass theoretical instruction, hands-on training using simulators and animal models, live demonstrations of EUS cases in endoscopy rooms, and, most critically, supervised performance of EUS procedures under expert guidance.
Another significant challenge is the availability of simulation models and training centers, as only a limited number of institutions have experienced endosonographers with a high annual volume of procedures to provide optimal-quality training. Trainees must perform a supervised procedure to gain full competency in conducting EUS and EUS-FNA/FNB independently.
According to recommendations from the ASGE and the ESGE, even after a trainee is deemed competent to practice EUS independently, they must document their annual number of EUS procedures and maintain proficiency by performing at least 100 diagnostic EUS examinations annually. Furthermore, regular assessments of procedural quality and outcomes are required using performance measures established by endoscopy societies. Additionally, trainees should continue their education through live courses, congresses, and hands-on workshops[5,39,40].
The ASGE has also published a core curriculum for EUS as a tool to improve the teaching and performance of EUS. It provides an overview of the main components of the procedure and information about the expert practices[41].
For interventional EUS, each procedure has a distinct learning curve, necessitating specialized training programs to mitigate associated risks. Various quality indicators for interventional EUS have been identified, including procedural safety, technical success, and complication management. Standardized training programs have been proposed to ensure competency, emphasizing these critical quality measures[12].
One of the most promising perspectives for EUS learning is the development of artificial intelligence (AI) technology. AI can assist beginners in the learning process by helping to recognise the lesion, reducing procedure times, and the need for mentoring to improve the quality of the procedure. AI also developed various algorithms that can be applied to tumor staging and prognostic analysis, and then provide treatment strategies[42-44].
AI can be used in several EUS fields, from preoperative consultation to intraoperative and postoperative guidance. AI-assisted EUS also plays a key role in interventional procedures, by helping to standardize performance between trainees and expert endosonographers[43].
Effective EUS training requires a structured approach integrating theoretical knowledge with practical experience. Various training programs exist globally, utilizing different modalities, including online lectures and onsite training. Although multiple EUS simulators are currently available, developing more advanced simulators capable of replicating real clinical scenarios remains necessary.
This mini-review outlines the different EUS training methods, emphasizing the major courses in the world and discussing their advantages and limitations. However, additional courses should be developed to enhance the effectiveness of training in both diagnostic and interventional EUS, incorporating more fellowship opportunities and long-term diploma programs that include supervised case observation and performance.
| 1. | Kim GH, Bang SJ, Hwang JH. Learning models for endoscopic ultrasonography in gastrointestinal endoscopy. World J Gastroenterol. 2015;21:5176-5182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 2. | Therapeutic Endoscopic Ultrasound. In: Evangelos Kalaitzakis, Peter Vilmann, Manoop S. Bhutani, editors. Cham: Springer, 2020. [DOI] [Full Text] |
| 3. | Eisen GM, Dominitz JA, Faigel DO, Goldstein JA, Petersen BT, Raddawi HM, Ryan ME, Vargo JJ 2nd, Young HS, Wheeler-Harbaugh J, Hawes RH, Brugge WR, Carrougher JG, Chak A, Faigel DO, Kochman ML, Savides TJ, Wallace MB, Wiersema MJ, Erickson RA; American Society for Gastrointestinal Endoscopy. Guidelines for credentialing and granting privileges for endoscopic ultrasound. Gastrointest Endosc. 2001;54:811-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 153] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | ASGE Standards of Practice Committee; Faulx AL, Lightdale JR, Acosta RD, Agrawal D, Bruining DH, Chandrasekhara V, Eloubeidi MA, Gurudu SR, Kelsey L, Khashab MA, Kothari S, Muthusamy VR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Guidelines for privileging, credentialing, and proctoring to perform GI endoscopy. Gastrointest Endosc. 2017;85:273-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 158] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 5. | Badaoui A, Teles de Campos S, Fusaroli P, Gincul R, Kahaleh M, Poley JW, Sosa Valencia L, Czako L, Gines A, Hucl T, Kalaitzakis E, Petrone MC, Sadik R, van Driel L, Vandeputte L, Tham T. Curriculum for diagnostic endoscopic ultrasound training in Europe: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2024;56:222-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 6. | El Menabawey T, McCrudden R, Shetty D, Hopper AD, Huggett MT, Bekkali N, Carroll NR, Henry E, Johnson GJ, Keane MG, Love M, McKay CJ, Norton S, Oppong K, Penman I, Ramesh J, Ryan B, Siau K, Nayar M. UK and Ireland Joint Advisory Group (JAG) consensus statements for training and certification in diagnostic endoscopic ultrasound (EUS). Gut. 2023;73:118-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Meenan J, Harris K, Oppong K, McKay C, Penman I, Carroll N, Norton S. Service provision and training for endoscopic ultrasound in the UK. Frontline Gastroenterol. 2011;2:188-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Johnson G, Webster G, Boškoski I, Campos S, Gölder SK, Schlag C, Anderloni A, Arnelo U, Badaoui A, Bekkali N, Christodoulou D, Czakó L, Fernandez Y Viesca M, Hritz I, Hucl T, Kalaitzakis E, Kylänpää L, Nedoluzhko I, Petrone MC, Poley JW, Seicean A, Vila J, Arvanitakis M, Dinis-Ribeiro M, Ponchon T, Bisschops R. Curriculum for ERCP and endoscopic ultrasound training in Europe: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2021;53:1071-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 78] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 9. | De Angelis CG. Training in Interventional EUS. In: Kalaitzakis E, Vilmann P, Bhutani M, (editors). Therapeutic Endoscopic Ultrasound. Cham: Springer, 2020. [DOI] [Full Text] |
| 10. | Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65:S63-S67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2527] [Cited by in RCA: 2286] [Article Influence: 65.3] [Reference Citation Analysis (0)] |
| 11. | Silva Mendes S, Areia M, Dinis Ribeiro M, Rolanda C. The Impact of a Structured Virtual Reality Simulation Training Curriculum for Novice Endoscopists. GE Port J Gastroenterol. 2022;29:385-392. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 12. | Miutescu B, Dhir V. Training and quality indicators in interventional endoscopic ultrasound. Dig Endosc. 2025;37:40-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Dhir V, Udawat P, Shah R, Alahari A. Feasibility of an EUS e-training course with live cases. Endosc Int Open. 2021;9:E1291-E1296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 14. | Bar-Meir S. A new endoscopic simulator. Endoscopy. 2000;32:898-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 56] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Götzberger M, Kaiser C, Jenssen C, Dollhopf M, Faiss S, Burmester E, Schöppe F, Gülberg V, Fischer MR. A structured Endoscopic Ultrasound training program in Germany improves knowledge and competence. Med Ultrason. 2021;23:396-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 16. | Finocchiaro M, Cortegoso Valdivia P, Hernansanz A, Marino N, Amram D, Casals A, Menciassi A, Marlicz W, Ciuti G, Koulaouzidis A. Training Simulators for Gastrointestinal Endoscopy: Current and Future Perspectives. Cancers (Basel). 2021;13:1427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 17. | Seitzinger M, Gnatzy F, Kern S, Steinhausen R, Klammer J, Schlosser T, Blank V, Karlas T. Development, evaluation, and overview of standardized training phantoms for abdominal ultrasound-guided interventions. Ultraschall Med. 2024;45:176-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Farjad Sultan S, Shorten G, Iohom G. Simulators for training in ultrasound guided procedures. Med Ultrason. 2013;15:125-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Neumann M, Mayer G, Ell C, Felzmann T, Reingruber B, Horbach T, Hohenberger W. The Erlangen Endo-Trainer: life-like simulation for diagnostic and interventional endoscopic retrograde cholangiography. Endoscopy. 2000;32:906-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 62] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Hochberger J, Maiss J, Magdeburg B, Cohen J, Hahn EG. Training simulators and education in gastrointestinal endoscopy: current status and perspectives in 2001. Endoscopy. 2001;33:541-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Hochberger J, Neumann M, Hohenberger W, Hahn EG. [EASIE-Erlangen Education Simulation Model for Interventional Endoscopy--a new bio-training model for surgical endoscopy]. Biomed Tech (Berl). 1997;42 Suppl:334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Desilets DJ, Banerjee S, Barth BA, Kaul V, Kethu SR, Pedrosa MC, Pfau PR, Tokar JL, Varadarajulu S, Wang A, Wong Kee Song LM, Rodriguez SA; ASGE Technology Committee. Endoscopic simulators. Gastrointest Endosc. 2011;73:861-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 23. | Matsuda K, Tajiri H, Hawes RH. How shall we experience EUS and EUS‐FNA before the first procedure?: The development of learning tools. Digeste Endosc. 2004;16. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Raizner A, Matthes K, Goodman AJ, Ho S, Robbins DH, Stavropoulos SN, Gress FG, Guthrie W, Lee Y. T1511: Evaluation of Novel Endoscopic Ultrasound (EUS) Training Simulator (the EASIE-R Simulator) for Teaching Basic and Advanced EUS: A Prospective Assessment of EUS Skills Using Objective Performance Criteria. Gastrointest Endosc. 2010;71:AB296. [DOI] [Full Text] |
| 25. | Hochberger J, Matthes K, Maiss J, Koebnick C, Hahn EG, Cohen J. Training with the compactEASIE biologic endoscopy simulator significantly improves hemostatic technical skill of gastroenterology fellows: a randomized controlled comparison with clinical endoscopy training alone. Gastrointest Endosc. 2005;61:204-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 104] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 26. | Dhir V, Itoi T, Pausawasdi N, Khashab MA, Perez-Miranda M, Sun S, Park DH, Iwashita T, Teoh AYB, Maydeo AP, Ho KY. Evaluation of a novel, hybrid model (Mumbai EUS II) for stepwise teaching and training in EUS-guided biliary drainage and rendezvous procedures. Endosc Int Open. 2017;5:E1087-E1095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Dhir V, Udawat P, Shah R, Alahari A. Evaluation of an all-in-one hybrid model (EUS Magic Box) for stepwise teaching and training in multiple interventional EUS procedures. Endosc Int Open. 2022;10:E634-E643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 28. | Chantarojanasiri T, Siripun A, Kongkam P, Pausawasdi N, Ratanachu-Ek T. Three-year evaluation of a novel, nonfluoroscopic, all-artificial model for EUS-guided biliary drainage training for the impact to practice: A prospective observational study (with videos). Endosc Ultrasound. 2023;12:96-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Bhutani MS, Hoffman BJ, Hawes RH. A swine model for teaching endoscopic ultrasound (EUS) imaging and intervention under EUS guidance. Endoscopy. 1998;30:605-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Bhutani MS, Aveyard M, Stills HF Jr. Improved model for teaching interventional EUS. Gastrointest Endosc. 2000;52:400-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Bhutani MS, Wong RF, Hoffman BJ. Training facilities in gastrointestinal endoscopy: an animal model as an aid to learning endoscopic ultrasound. Endoscopy. 2006;38:932-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Giovannini M. Learning in therapeutic EUS. Endosc Ultrasound. 2021;10:317-318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 33. | Barthet M. Endoscopic ultrasound teaching and learning. Minerva Med. 2007;98:247-251. [PubMed] |
| 34. | Barthet M, Gasmi M. Teaching and credentialing in France. Endoscopy. 2006;38 Suppl 1:S60-S61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 35. | Ligresti D, Kuo YT, Baraldo S, Chavan R, Keane MG, Seleem S, Seo DW. EUS anatomy of the pancreatobiliary system in a swine model: The WISE experience. Endosc Ultrasound. 2019;8:249-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Omoto S, Takenaka M, Maluf-Filho F, Kudo M. A novel and effective EUS training program that enables visualization of the learning curve: Educational Program of Kindai system (EPOK). VideoGIE. 2022;7:165-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 37. | Leong Ang T, De Angelis CG, Alvarez-Sanchez M, Chak A, Chang KJ, Chen R, Eloubeidi M, Herth FJ, Hirooka K, Irisawa A, Jin Z, Kida M, Kitano M, Levy MJ, Maguchi H, Napoleon BV, Penman I, Seewald S, Wang G, Wallace M, Yamao K, Yasuda I, Yasuda K, Yasufuku K. EUS 2010 in Shanghai - Highlights and Scientific Abstracts. Endoscopy. 2011;43 Suppl 3:S1-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 38. | Wong JYY, Kongkam P, Ho KY. Training in endoscopic ultrasonography: An Asian perspective. Dig Endosc. 2017;29:512-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 39. | Domagk D, Oppong KW, Aabakken L, Czakó L, Gyökeres T, Manes G, Meier P, Poley JW, Ponchon T, Tringali A, Bellisario C, Minozzi S, Senore C, Bennett C, Bretthauer M, Hassan C, Kaminski MF, Dinis-Ribeiro M, Rees CJ, Spada C, Valori R, Bisschops R, Rutter MD. Performance measures for ERCP and endoscopic ultrasound: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2018;50:1116-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 40. | Hedenström P, Sadik R. The assessment of endosonographers in training. World J Clin Cases. 2018;6:735-744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 41. | 41 Cassani L, Aihara H, Anand GS, Chahal P, Dacha S, Duloy A, Ghassemi S, Huang C, Kowalski TE, Kushnir V, Qayed E, Sheth SG, Simons-Linares CR, Taylor JR, Umar SB, Vela SAF, Walsh CM, Williams RL, Wagh MS; American Society for Gastrointestinal Endoscopy Training Committee. Core curriculum for EUS. Gastrointest Endosc. 2020;92:469-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Zhang D, Wu C, Yang Z, Yin H, Liu Y, Li W, Huang H, Jin Z. The application of artificial intelligence in EUS. Endosc Ultrasound. 2024;13:65-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 43. | Mahajan S, Siyu S, Bhutani MS. What can artificial intelligence do for EUS? Endosc Ultrasound. 2025;14:1-3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 44. | Khalaf K, Terrin M, Jovani M, Rizkala T, Spadaccini M, Pawlak KM, Colombo M, Andreozzi M, Fugazza A, Facciorusso A, Grizzi F, Hassan C, Repici A, Carrara S. A Comprehensive Guide to Artificial Intelligence in Endoscopic Ultrasound. J Clin Med. 2023;12:3757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 6.0] [Reference Citation Analysis (0)] |