Published online Aug 16, 2025. doi: 10.4253/wjge.v17.i8.102787
Revised: March 20, 2025
Accepted: July 29, 2025
Published online: August 16, 2025
Processing time: 287 Days and 12.1 Hours
In postsurgical upper gastrointestinal anatomy, motorized spiral enteroscopy (MSE) assisted endoscopic retrograde cholangiopancreaticography (ERCP) was shown feasible and has the advantage that standard ERCP instruments can be used. Therefore, MSE-ERCP appears to be the optimal solution for postsurgical patients, especially with Roux-en-Y anatomy.
To show feasibility and safety of MSE-ERCP in patients with Roux-en-Y anatomy.
We retrospectively analyzed all consecutive MSE-ERCP procedures in patients with Roux-en-Y anatomy between September 2021 and May 2023 in an endo
We identified 26 MSE-ERCPs: (1) 18 MSE-ERCPs in 13 patients with Roux-en-Y anatomy after liver transplantation (n = 11) or gastrectomy (n = 2); and (2) An
MSE-ERCP has been a promising technique for patients with Roux-en-Y reconstruction requiring biliary in
Core Tip: Motorized spiral enteroscopy assisted endoscopic retrograde cholangiopancreaticography is a promising technique for performing biliary interventions in postsurgical patients with Roux-en-Y anatomy, achieving an 88% success rate for accessing the biliary entry and demonstrating feasibility in outpatient settings. Despite recent safety concerns leading to its market withdrawal, this study found no severe adverse events associated with the procedure.
- Citation: Nennstiel S, Fried R, Herner A, Schlag C. Motorized spiral enteroscopy assisted endoscopic retrograde cholangiography in patients with Roux-en-Y-anatomy. World J Gastrointest Endosc 2025; 17(8): 102787
- URL: https://www.wjgnet.com/1948-5190/full/v17/i8/102787.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i8.102787
Altered upper gastrointestinal (GI) anatomy impedes performance of standard endoscopic retrograde cholangiopancreaticography (ERCP)[1,2]. In these patients, referral to specialized centers is suggested[3], where enteroscopy-assisted, percutaneous or endoscopic ultrasound (EUS)-guided biliary interventions are available. However, in Roux-en-Y alimentary limb situations, success of enteroscopy-assisted ERCP with long colonoscopes, single-balloon-enteroscopes (SBE) or double-balloon-enteroscopes (DBE) can be limited[4]. Motorized spiral enteroscopy (MSE) was shown to be feasible in patients with altered anatomy, without a significant increase in sepsis-associated encephalopathy rates[5-7]. Furthermore, feasibility of MSE-assisted ERCP was first reported in 2020[8] and successful use of spiral-enteroscopy-assisted ERCPs in patients with altered anatomy were described recently[7,9]. Particularly in Roux-en-Y anatomy potential advantages of the MSE over standard SBE or DBE are a shorter scope length and the compatibility with a variety of standard ERCP tools. Aim of our study was to show feasibility and safety of MSE-ERCP in patients with Roux-en-Y anatomy.
We retrospectively analyzed all MSE-assisted ERCP procedures in patients with Roux-en-Y anatomy conducted at Endoscopic Department of the University Hospital Zurich, between September 2021 and May 2023. Procedural success was defined as: (1) Reaching the papilla/the hepatico-jejunostomy (“biliary entry”); and (2) Cannulation of the biliary tract with intervention of any type (e.g. cholangiography, stenting, stone removal, etc.). Durations of the procedures were recorded as well as patient specific characteristics, like age, gender, upper GI anatomy and indication for the procedure. Additionally, procedure and non-procedure related adverse events (AE) were assessed.
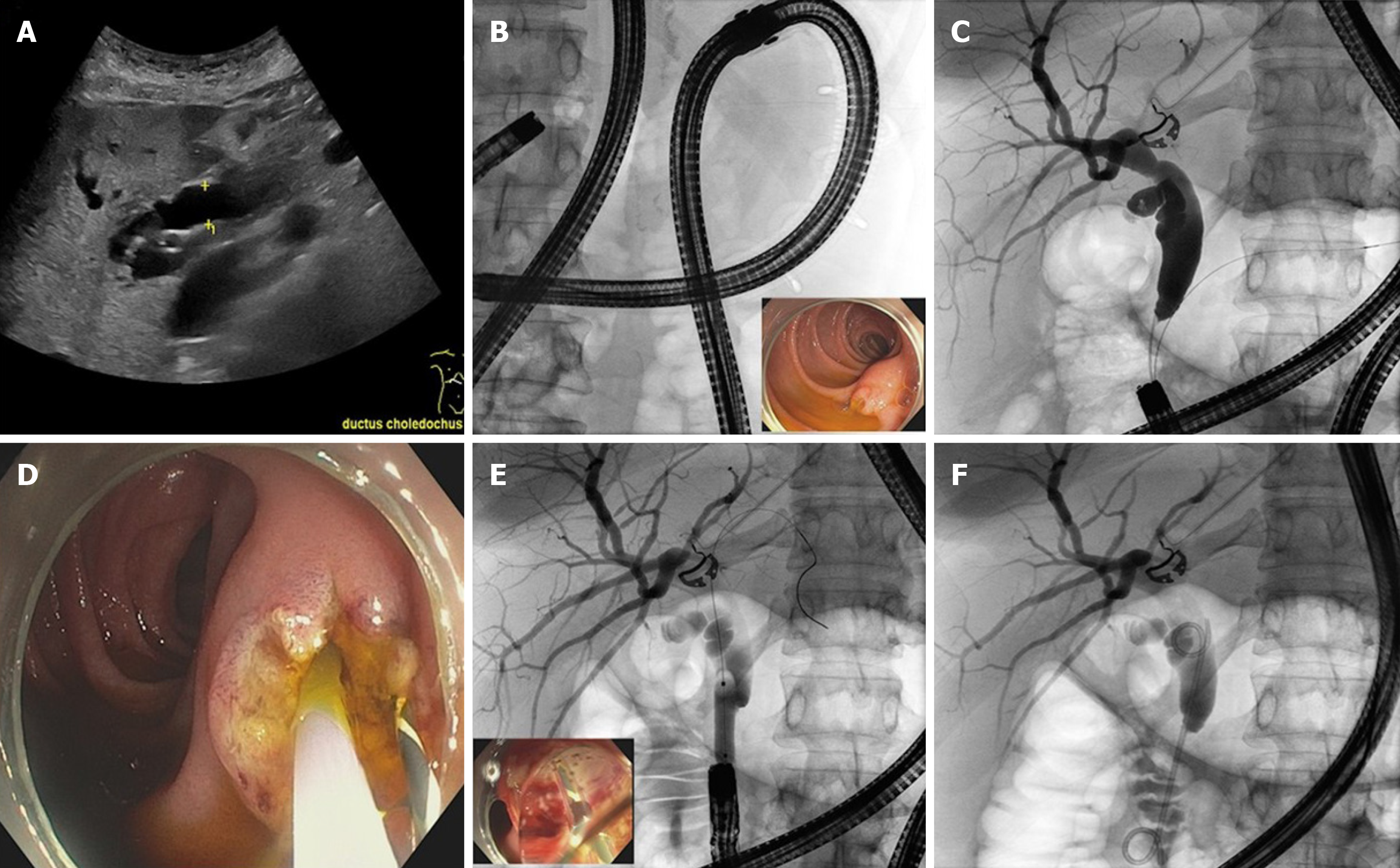
The PowerSpiral enteroscope (PSF-1; Olympus Medical Systems Corporation, Tokyo, Japan) with a mounted transparent distal hood was used in all examinations. The first step of the MSE-ERCP procedure is to reach the afferent/hepatobiliary limb and to advance the endoscope to the biliary entry. For this part external abdominal compression/massage may be used for adequate advancement of the scope. Second step is to cannulate the biliary system for cholangiography and further interventions like dilation, stone-removal and stent-insertion. Due to the PowerSpiral enteroscopes short length (168 cm), and its working channel size of 3.2 mm, ERCP instruments with a minimal length of 180 cm can be used for biliary interventions[8]. All procedures were performed under general anesthesia by two interventional endoscopists (Nennstiel S and Schlag C) with dedicated training and great experience in MSE and biliary interventions.
For qualitative data, absolute and relative frequencies are shown. Quantitative data are presented by means ± SD. To compare means between two independent groups, the Mann-Whitney U test was used. Fishers’ exact tests were performed for the comparison of qualitative data between patient groups. All statistical tests were performed two-sided using a level of significance of α = 5%.
During the specified time, 26 MSE-ERCPs were performed in a total of 18 patients with Roux-en-Y-Anatomy. Results are displayed in detail in Table 1.
| n | Female | Age (years) (mean) | Success: Reaching the biliary entry | Success: Intervention | Outpatient | Duration (minutes) (mean) | Complications | |
| Patients, overall | 18 | 10 (53) | 64 | |||||
| Examinations | 26 | 15 (58) | 23/26 (88%) | 19/23 (83%) | 15/26 (61%) | 105 | ||
| Patients with gastric bypass (very long alimentary limb) | 5 | 3 (60) | 65 | Laceration of gastrojejunostomy (n = 1) and post-endoscopic retrograde cholangiopancreaticography pancreatitis (n = 1) | ||||
| Examinations | 8 | 6 (75) | 6/8 (75%) | 5/6 (83%) | 5/8 (63%) | 133 | ||
| Patients with “standard” Roux-en-Y | 13 | 5 (50) | 59 | Complication of anesthesia with reanimation (n = 1) | ||||
| Examinations | 18 | 7 (47) | 17/18 (94%) | 14/17 (82%) | 10/18 (56%) | 91 |
Overall, the biliary entrance could be reached in 23 of 26 cases (88%). In patients after Roux-en-Y situation after gastric bypass (RYGB) with a very long alimentary limb anatomy, enteroscopy success was not-significantly lower compared to patients with long limb anatomy (75% vs 94%, P = 0.215).
Biliary interventions (including cholangiography, endoscopic papillotomy, needle knife precut sphincterotomy, stricture-dilation, stone-removal, brush-cytology, biopsies and insertion of plastic as well as self-expanding metals stents, devices listed in Table 2) were successful in 19/23 cases (83%). Interventional success rates were not-significantly lower in cases with a preserved papilla compared to patients with hepaticojejunostomy (67% vs 93%, P = 0.103).
| Device | Manufacturer | Length (cm) |
| “Standard”-devices | ||
| Glo-tip ERCP-catheter | Cook medical | 200 |
| Huibregtse catheter | Cook medical | 220 |
| self-expanding metals stents: WallFlex™ Biliary (Rx Fully Covered; 8/10 mm × 40/60/80 mm) | Boston scientific | 194 |
| RX needle knife XL | Boston scientific | 200 |
| RX cytology brush | Boston scientific | 200 |
| Devices designed for Balloon-enteroscopy-assisted ERCP | ||
| Pushing catheter | Cook medical | 320 |
| Dilation balloon catheter (Ø 6-7-8 mm) | Micro-Tech™ Endoscopy | 230 |
| Stone removal balloon Multi-3V Plus | Olympus | 240 |
| Papillotome AXS_tome PAP1-D2-30-21-OL | Fujifilm medwork | 260 |
The overall mean procedure time was 105 ± 41 minutes. However, in patients with a very long alimentary limb anatomy, mean procedure times were longer compared to patients with simple Roux-en-Y reconstruction (133 minutes vs 91 minutes; P = 0.032).
Overall, three AE (11.5%) were observed: (1) One enteroscopy associated AE: A superficial laceration of the gastrojejunostomy in a RYGB-patient was treated by endoscopic clip application; (2) One ERCP-associated complication: A post ERCP-pancreatitis was treated conservatively; and (3) In one hepaticojejunostomy-patient with cholestasis due to recurrence of a cholangicarcinoma after liver transplantation: A circulatory arrest occurred after a sudden drop of oxygen saturation just at the time when the biliary entry was reached and first cholangiography was achieved. The patient was stabilized after return of spontaneous circulation and MSE-ERCP was successfully performed one week later. A total of 17/26 procedures (65%) were performed in an outpatient-setting.
For patients with biliary disease and altered upper GI anatomy, MSE could offer a beneficial combination for deep enteric intubation[10] as well as biliary interventions. Given the 3.2 mm working channel and the 168 cm working length of the PowerSpiral enteroscope, nearly all interventions feasible during conventional ERCP — including the deployment of self-expanding biliary metal stents — can also be performed during MSE-ERCP. Our data shows that MSE-ERCP has good enteroscopy success (88%) as well as cannulation/interventional-success (83%) in patients with Roux-en-Y reconstruction. These results are comparable to those recently reported by Schneider et al[9], with an enteroscopy-to-target success of 86% and a cannulation-success of 84% in a total of 36 patients including not only Roux-en-Y but also billroth-II surgery patients. In another study by Buchholz et al[7], including 15 patients with Roux-en-Y anatomy, successful passage to the biliary entry was achieved in 9 patients (60%), and biliary intervention was successful in 7 of these patients (78%). Although these results are really encouraging, it has always to be considered that MSE-ERCP procedures are quite time-consuming, mostly caused by the often times cumbersome passage to the biliary entry. Consequently, our data shows that the longer the route to the biliary entry, as in gastric-bypass patients, the more time is required for the examination (Figure 1). However, as a limitation, only total examination times without distinction of time needed for enteroscopy and for the biliary intervention were regarded in this retrospective study. Additionally, the likelihood of reaching the biliary entry is lower in patients with a very long alimentary limb, for the biliary entry could be reached in 94% of patients after hepaticojejunostomy, compared to 75% of patients with gastric bypass. When being compared to enteroscopy assisted ERCP in Roux-en-Y situations using balloon-enteroscopes or push-enteroscopy with enteroscopy-to-target-success-rates around 60%-85% for “standard” Roux-en-Y and 72%-87% for RYGB patients[4,11-13], we feel that utilization of the motorized spiral enteroscope adds a beneficial technique with a good enteroscopy-to-biliary-entry success rates. Appropriate prospective studies with direct comparison of balloon- and the motorized spiral enteroscopes however are lacking[10,14]. At least, there’s available data, comparing rotational overtube (RO)–assisted enteroscopy ERCP with balloon-enteroscopy (SBE, DBE) assisted ERCP in surgically altered anatomy. Enteroscopy success rates of the different devices were similar in RYGB anatomy (RO: 73%, SBE: 73%, DBE: 87%) vs non-RYGB anatomy (RO: 71%, SBE: 65%, DBE: 58%), however many patients without Roux-en-Y alimentary limb situation were included in the latter group[12].
Enteroscopy with the aim of reaching the biliary entry however is not the only challenge of MSE-ERCP, for also biliary cannulation and interventions need to be done. In patients with bilioenteric anastomoses, cannulation/intervention success is high (> 90%). However, in patients with a naïve papilla, gaining access to the biliary system can be challenging or even impossible, as the papilla is approached from its reverse side.. In our data, cannulation/intervention success decreased to 62.5% in patients with naïve papilla (compared to 93% in patients with hepaticojejunostomy). Similar numbers were published by Schneider et al[9] with cannulation success of 60% in naïve papilla (bilioenteric anastomoses 88.5%).
In our data, the majority of examinations were performed on an outpatient basis, although all of the presented procedures were carried out under general anesthesia. We chose general anesthesia to ensure stable patient conditions for the duration of the examination and for safety reasons, since the PowerSpiral enteroscope cannot be removed promptly in case of an upper airway emergency. Other endoscopic centers started nurse-assisted deep sedation for MSE-procedures, without a relevant increase in sedation-related complications[5,9]. However, in our cohort, a serious adverse event of a cardiac arrest in a septic patient occurred, which resulted in successful reanimation of the patient and the MSE-ERCP was repeated one week later without any further complications. This rare case shows that caution must always be exercised during sedation/anesthesia for complex endoscopic interventions.
In general, MSE-ERCP carries the risk of complications caused by the enteroscopy as well as the ERCP. In our data, both types of complications occurred. In one patient superficial laceration of gastrojejunostomy caused by the spiral enteroscope was noted and was resolved by clipping without any further problems (minor complication). In another patient post-ERCP pancreatitis was treated conservatively, but resulted in a longer hospital stay (major complication). Thus, the overall complication rate in our collective was 10.7% (minor: 3.5%, major: 7.1%) and 7.1% (minor and major 3.5%; 3.5% for enteroscopy 3.5% for ERCP) only regarding complications by the MSE-ERCP itself. Regarding the literature concerning complications during enteroscopy with the motorized spiral enteroscope, a recent systematic review and meta-analysis reported overall complication rates of 17% (major: 1%) for all patients (with normal and postsurgical anatomy)[10]. In a prospective study including patients with normal anatomy as well as altered anatomy, adverse event rates were 2% compared to 4% for the latter group[5]. For MSE-ERCP specifically, Schneider et al[9], reported an adverse event rate of 5.6% (major 2.8%). All AEs were bleedings after sphincterotomy or balloon-dilation of the bilioenteric anastomosis. In the study of Buchholz et al[7] 2/15 MSE-ERCP patients (13%) suffered of minor bleeding after balloon-dilation of the bilioenteric anastomosis. In summary, complications of biliary interventions during MSE-ERCP do not seem to exceed the known adverse event rates of conventional ERCP (5%-28%)[15]. It must be taken into consideration that patients with Roux-en-Y and naïve papilla could carry a higher risk due to the altered and more difficult access to the papilla orifice and on the other hand there is practically no risk for post-ERCP pancreatitis in patients with hepaticojejunostomy.
However, there has been rare reports of severe AE[16] and most recently MSE has been withdrawn from the market after a case where the withdrawal of the PowerSpiral enteroscope from a patient was unsuccessful and had to be removed surgically leading to catastrophic injury and death to the patient[17].
Main advantage of MSE-assisted ERCP is that the underlying, altered anatomy is respected during the examination. Alternative, more invasive procedures like EUS-guided interventions usually do not respect these given anatomic circumstances. Complication rates for these procedures can be quite high, even when performed by expert hands[1]. Also, an altered anatomy can render EUS-guided biliary drainage impossible. Especially in patients after gastric bypass, EUS-directed transgastric ERCP is a valuable approach. With this technique, a fully covered metal stent is placed from the gastric pouch into the excluded stomach, and a duodenoscope is then advanced through the stent to the papilla. High technical (100%) and clinical (60%-100%) success rates with low adverse event rates (1.5%-7.6%) have been reported for this technique, however there is a considerable risk of dislodgement of the gastro-gastric stent in up to 20%[18]. Percutaneous transhepatic biliary drainage (PTBD) on the other hand, offers high success rates, irrespective of the underlying anatomy, however it comes along with substantial complication rates in the short as well as the long term[4,19]. In addition, PTBD is associated with reduced quality of life as well as lower levels of patients’ acceptance.
The main limitations of this study are its retrospective design and relatively small sample size, which may affect the robustness of the statistical analysis. However, to the best of our knowledge it is the first study particularly focusing on the feasibility of MSE-ERCP in patients with Roux-en-Y anatomy.
In conclusion, MSE-ERCP is a valuable procedure with high success rates for patients with postsurgical upper GI anatomy which often can be done in an outpatient setting. Further prospective trials would have been most desirable to further implement the role of MSE-ERCP in patients with altered anatomy. Unfortunately, MSE was recently withdrawn from the market due to substantial safety concerns, which were not seen in our study.
| 1. | Krutsri C, Kida M, Yamauchi H, Iwai T, Imaizumi H, Koizumi W. Current status of endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy. World J Gastroenterol. 2019;25:3313-3333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 61] [Article Influence: 10.2] [Reference Citation Analysis (3)] |
| 2. | Zhang LY, Irani S, Khashab MA. Biliary Endoscopy in Altered Anatomy. Gastrointest Endosc Clin N Am. 2022;32:563-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 3. | Dumonceau JM, Tringali A, Papanikolaou IS, Blero D, Mangiavillano B, Schmidt A, Vanbiervliet G, Costamagna G, Devière J, García-Cano J, Gyökeres T, Hassan C, Prat F, Siersema PD, van Hooft JE. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy. 2018;50:910-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 529] [Cited by in RCA: 480] [Article Influence: 68.6] [Reference Citation Analysis (0)] |
| 4. | Nennstiel S, Freivogel K, Faber A, Schlag C, Haller B, Blöchinger M, Dollhopf M, Lewerenz B, Schepp W, Schirra J, Schmid RM, Neu B. Endoscopic and percutaneous biliary interventions in patients with altered upper gastrointestinal anatomy-the Munich Multicenter Experience. Surg Endosc. 2021;35:6853-6864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 5. | Beyna T, Moreels T, Arvanitakis M, Pioche M, Saurin JC, May A, Knabe M, Agnholt JS, Bjerregaard NC, Puustinen L, Schlag C, Aabakken L, Paulsen V, Schneider M, Neurath MF, Rath T, Devière J, Neuhaus H. Motorized spiral enteroscopy: results of an international multicenter prospective observational clinical study in patients with normal and altered gastrointestinal anatomy. Endoscopy. 2022;54:1147-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 6. | Al-Toma A, Beaumont H, Koornstra JJ, van Boeckel P, Hergelink DO, van der Kraan J, Inderson A, de Ridder R, Jacobs M. The performance and safety of motorized spiral enteroscopy, including in patients with surgically altered gastrointestinal anatomy: a multicenter prospective study. Endoscopy. 2022;54:1034-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 7. | Buchholz H, Mende M, Hornoff S, Faiss S. [Results of motorized spiral enteroscopy in 83 consecutive patients]. Z Gastroenterol. 2022;60:1635-1643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Beyna T, Schneider M, Höllerich J, Neuhaus H. Motorized spiral enteroscopy-assisted ERCP after Roux-en-Y reconstructive surgery and bilioenteric anastomosis: first clinical case. VideoGIE. 2020;5:311-313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Schneider M, Höllerich J, Gerges C, Balasus N, Neuhaus H, Beyna T. Motorized spiral enteroscopy-assisted ERCP in surgically altered anatomy: early experience from a retrospective cohort study. Endoscopy. 2023;55:476-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 10. | Papaefthymiou A, Ramai D, Maida M, Tziatzios G, Viesca MFY, Papanikolaou I, Paraskeva K, Triantafyllou K, Repici A, Hassan C, Binda C, Beyna T, Facciorusso A, Arvanitakis M, Gkolfakis P. Performance and safety of motorized spiral enteroscopy: a systematic review and meta-analysis. Gastrointest Endosc. 2023;97:849-858.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 11. | Schreiner MA, Chang L, Gluck M, Irani S, Gan SI, Brandabur JJ, Thirlby R, Moonka R, Kozarek RA, Ross AS. Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP in bariatric post-Roux-en-Y gastric bypass patients. Gastrointest Endosc. 2012;75:748-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 168] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 12. | Shah RJ, Smolkin M, Yen R, Ross A, Kozarek RA, Howell DA, Bakis G, Jonnalagadda SS, Al-Lehibi AA, Hardy A, Morgan DR, Sethi A, Stevens PD, Akerman PA, Thakkar SJ, Brauer BC. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc. 2013;77:593-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 200] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 13. | Skinner M, Popa D, Neumann H, Wilcox CM, Mönkemüller K. ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 2014;46:560-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 153] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 14. | Chan W, Wei LK, Tan T, Hsiang LG, Kong C, Salazar E, Koay D, Khor C, Asokkumar R. Motorized spiral enteroscopy versus double-balloon enteroscopy: a case-matched study. Gastrointest Endosc. 2023;97:314-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 15. | Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro M, Hritz I, Mariani A, Paspatis G, Radaelli F, Lakhtakia S, Veitch AM, van Hooft JE. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52:127-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 496] [Article Influence: 99.2] [Reference Citation Analysis (1)] |
| 16. | Wiedbrauck D, Wiedbrauck F, Freund U, Rodenberg F, Prenzel J, Hollerbach S. Spontaneous detachment of the spiral overtube from the endoscope in the upper esophagus: a case report and literature review of a rare complication during motorized spiral enteroscopy. Z Gastroenterol. 2024;62:407-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Olympus Medical. Urgent field safety notice QIL FY24-EMEA-10-FY24-OMSC-05 2023. Available from: https://www.igj.nl/binaries/igj/documenten/waarschuwingen/2023/07/11/fsn-qil-fy24-emea-10-fy24-omsc-05-olympus-medical-systems-corporation-powerspiral-intestinal-videoscope-psf-1/IT2081382+FSN-QIL+FY24-EMEA-10-FY24-OMSC-05+Olympus+Medical+Systems+Corporation+PowerSpiral+Intestinal+Videoscope+PSF-1.pdf. |
| 18. | Khara HS, Parvataneni S, Park S, Choi J, Kothari TH, Kothari ST. Review of ERCP Techniques in Roux-en-Y Gastric Bypass Patients: Highlight on the Novel EUS-Directed Transgastric ERCP (EGDE) Technique. Curr Gastroenterol Rep. 2021;23:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 19. | Nennstiel S, Weber A, Frick G, Haller B, Meining A, Schmid RM, Neu B. Drainage-related Complications in Percutaneous Transhepatic Biliary Drainage: An Analysis Over 10 Years. J Clin Gastroenterol. 2015;49:764-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 137] [Article Influence: 13.7] [Reference Citation Analysis (0)] |