Published online Nov 16, 2023. doi: 10.4253/wjge.v15.i11.634
Peer-review started: August 9, 2023
First decision: September 4, 2023
Revised: September 12, 2023
Accepted: October 23, 2023
Article in press: October 23, 2023
Published online: November 16, 2023
Processing time: 92 Days and 17.3 Hours
Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) has been tran
Core Tip: Endoscopic ultrasound guided gastroenterostomy (EUS-GE) is still a technically challenging procedure. In order to improve EUS-GE, several techniques have been reported to improve the technical details. With EUS-GE widely performed, more data about EUS-GE’s clinical outcomes have been reported. Knowledge of complications during performing EUS-GE is essential to perform it well. The aim of the current review is to describe technical details updates, clinical outcomes, and adverse events of EUS-GE.
- Citation: Wang J, Hu JL, Sun SY. Endoscopic ultrasound guided gastroenterostomy: Technical details updates, clinical outcomes, and adverse events. World J Gastrointest Endosc 2023; 15(11): 634-640
- URL: https://www.wjgnet.com/1948-5190/full/v15/i11/634.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i11.634
Based on the development of accessory devices, such as lumen-apposing metal stents (LAMS)[1], more interventional endoscopic ultrasound (EUS) procedures could be performed[2-4], including EUS-guided gastroenterostomy (EUS-GE)[5,6]. The first EUS-GE was reported in an animal study by Binmoeller et al[7] in 2012, demonstrating that EUS-GE was a technically feasible procedure. The indication of EUS-GE was initially for the treatment of malignant gastric outlet obstruction (GOO). With EUS-GE developing rapidly in the last five years, EUS-GE could be used to treat malignant GOO and benign GOO[8], as well as afferent loop syndrome[9-11]. Even EUS-GE assisted ERCP could be performed in patients with Roux-en-Y gastric bypass[12-15]. However, EUS-GE is a technically challenging procedure, because the intestinal cavity is small and small bowel is free. Adverse events, such as misplacement of metal stent, could occur during the procedure. In order to simply EUS-GE, several techniques have been reported[16-18].
The aim of the current review is to describe technical details updates, clinical outcomes, and adverse events of EUS-GE.
The direct EUS-GE is usually performed as follows: puncturing a small bowel loop adjacent to the stomach with a 22-gauge needle to dilate the target small bowel with saline. After puncture with a 19-gauge FNA needle, an enterogram is obtained and a wire is inserted through the needle into the small bowel. The tract is then dilated along the wire and the LAMS is placed. Based on direct EUS-GE, several techniques have been used to distend the jejunum, stabilize the target jejuna loop and simply the procedure.
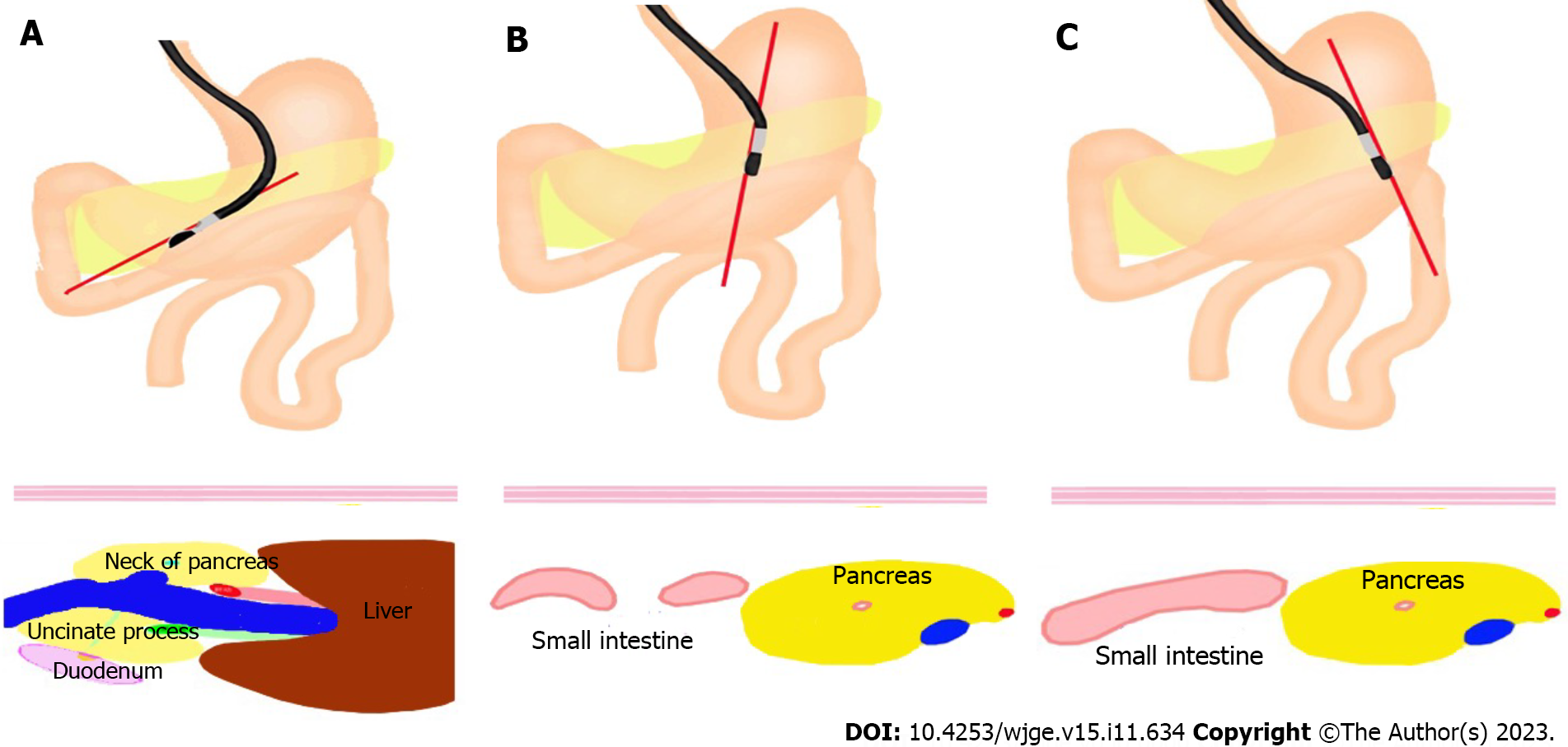
It is of importance to know how to scan the suitable bowel to do EUS-GE. At first, when we scan the confluence of splenic vein and superior mesenteric vein, we can see the neck of pancreas, uncinate process and the second part of duodenum behind the uncinate process. We slightly rotate the endoscope, then we can see the bowel near to stomach and below the pancreas, which is a good place to perform EUS-GE (Figure 1).
To distend the jejunum, water-filling technique[19] and water-inflated balloon technique[20-22] have been used. For water-filling technique, before the performance of EUS-GE, a nasobiliary drain tube was usually inserted into jejunum over guidewire, through the stenosis, connected to a syringe. The saline with blue dye was injected into jejunum to distend intestinal lumen. The advantage of colored saline than only saline is that the pullback of blue saline by the needle can help confirm the successful puncture of jejunum, avoiding mispuncture of colon[23]. Instead of syringe, a waterjet system was used to constantly inject saline, which could be performed by the operator. For water-inflated balloon technique including single-balloon-occluded gastroenterostomy and double-balloon-occluded gastrojejunostomy bypass (EPASS), Itoi et al[24] first reported EPASS and it was widely used in clinical practice. In the EPASS technique, a guidewire and/or an overtube was used to facilitate passage of the double-balloon enteric tube into the jejunum beyond the ligament of Itoi et al[25] reported that a 0.89-inch large diameter guidewire was used to assist passage of the double-balloon enteric tube into the jejunum and a large diameter guidewire can avoid the looping of the balloon tube in the stomach fornix. The saline solution is only filled between two balloons over this area, making it easy to locate the distended jejunum under EUS guidance and allowing easy and safe access to the jejunum.
Because this device is not, however, available everywhere, an occlusive double-balloon device, using a widely available vascular balloon catheter, for EUS-GE has been reported[26].
To stabilize the target jejuna loop, the anchor wire[7] and retrievable anchor[27-29] was used to appose small bowel against the gastric wall. Small intestine is free in the abdominal cavity, which made EUS-GE difficult to perform. Any device to access small intestine might push small intestine away from the stomach, which made EUS-GE failed. Even with EPASS, two unsuccessful stent deployment cases occurred, due to guidewire pushing the distended jejunum to move away from the stomach[25]. So it is important to fix the small intestine. The distal end of the 0.035-inch wire has three triangular anchor components. The retrievable anchor is similar to T-tag anchor with a retrievable wire. When performing EUS-GE, the small bowel was punctured with a 19-G FNA needle, the anchor wire or retrievable anchor was inserted through a standard 19-G FNA needle to appose the small bowel against the gastric wall. Both the anchor wire and retrievable anchor could be retrieved after EUS-GE.
To simply the EUS-GE, electrocautery-enhanced LAMS[30,31] was used, even wireless EUS-GE[32-35] was performed. As mentioned above, any device to access small intestine might push small intestine away from the stomach. Electrocautery-enhanced LAMS can combine the tract dilation with stent insertion, which reduces tract dilation step of EUS-GE. For wireless EUS-GE, after confirmation of the target loop, the electrocautery-enhanced LAMS was inserted directly into the targeted jejunal loop without using a guidewire. In their opinion, if we can observe the distended small bowel and nasojejunal catheter adequately under EUS, confirmatory puncture by a 19-gauge needle and guidewire cannulation is an unnecessary step; it increases costs and procedure duration and may provide a false sense of security. During this procedure, the power should be set to enable LAMS entering small intestine quickly, otherwise LAMS might push the small intestinal away.
With more articles about EUS-GE published in recent 5 years, systematic reviews and meta-analysis suggested that EUS-GE has good overall technical and clinical success, as well as acceptable complication rates, despite EUS-GE technique[36-38].
For success rate between different techniques of EUS-GE, only one study evaluated the direct and balloon-assisted techniques[39]. The two groups had similar technical success rate, clinical success rate, rate of complications, postoperative length of stay, need for re-intervention and survival, but the direct technique may be the preferred method, due to mean procedure time shorter with the direct technique (P < 0.001). All the medical centers included in this study were from United States and Europe and the single balloon-assisted EUS-GE was performed in this study. Further studies are expected to confirm the results.
The size of LAMS has been the subject of debate. The 15-mm LAMS has always been used to perform EUS-GE and it has been proven to be technically feasible, clinically effective, and safe. Madanat et al[40] first reported the use of the 20-mm LAMS for an EUS-GE. Theoretically, better clinical outcomes may be achieved with the 20 mm LAMS with a wider lumen. But it is concerned that 20-mm LAMS’s wider luminal diameter and larger flange size may lead to difficulty in deploying. Sobani et al[41] reported EUS-GE with 20mm-LAMS is a technically feasible and safe option for patients with GOO allowing for tolerability of regular diet. A recent study compared 20-mm LAMS with 15-mm LAMS in performing EUS-GE. The type of diet tolerated at follow-up differed between the two groups, although clinical success was similar. A higher proportion of patients in the 20 mm LAMS group tolerated a soft/full diet compared to those in the 15 mm group (P = 0.04)[42]. The 20-mm LAMS is, thus, the preferred LAMS during EUS-GE.
Through maturation of the EUS-GE technique, EUS-GE was compared with surgical gastroenterostomy (SGE)[43-45] and enteral stenting for the treatment of GOO[46-48]. In several retrospective studies, EUS-GE has been proposed as an alternative to enteral stenting with similar safety and surgical range-efficacy. The most recent systematic review, including 625 patients, comparing EUS-GE with SGE showed that the pooled odds of technical success were lower for EUS-GE compared to SGE. Among the technically successful cases, EUS-GE was superior in terms of clinical success, lower overall AE and shorter procedure time. There was no significant difference about rates of severe AE and GOO recurrence between EUS-GE and SGE. The results suggested EUS-GE is a promising alternative to SGE because of its superior clinical success, overall safety, and efficiency[49].
Compared with enteral stent (ES), a recent systematic review including 659 patients demonstrated that EUS-GE and ES has a similar technical and clinical success rate, but the pooled re-intervention rate was significantly lower for EUS-GE than ES[50].
Knowledge of adverse events encountered with EUS-GE is essential to perform it well. The EUS-GE-related complications included LAMS misdeployment, abdominal pain, bleeding , infection , leakage at the site of the LAMS, gastric leak , stent ingrowth, stent failure, and LAMS mesh erosion[43,45,48,51,52].
LAMS displacement is the most typical adverse event evaluated in the largest multicenter cohort to date, and the different types of stent displacement were classified into four types[53]. Type I was defined as distal flange of stent displaced in the abdominal cavity without enterotomy. Type II was defined as distal flange of stent displaced in the abdominal cavity with concomitant enterotomy. Type III was defined as distal flange of stent into the small bowel and proximal flange of stent in the abdominal cavity. Type IV was defined as gastrocolonic anastomosis. Type I stent displacement was the most common among four types. For both type I and type II stent displacements, the majority of patients can be successfully managed by endoscopic methods or conservative treatment. Type I stent displacements were more frequently rated as mild than type II stent displacements. Depending on the type of stent displacement, it is important for endoscopists to have a better understanding of the implications and possible consequences of stent displacement. Depending on the subtype, the majority of stent displacement can be successfully managed by endoscopic salvage. Several rescue options have been previously reported for gastroenterostomy[54-59]. The rescue method was usually based on the status of guidewire. If the guidewire could not enter the target loop again, LAMS misdeployment can require natural orifice transluminal endoscopic surgery. For the most common situation, distal LAMS flange misplacement, we could enter peritoneal cavity through transgastric LAMS using a therapeutic gastroscope or double-channel gastroscope and put a second stent to form LAMS-in-LAMS salvage. If the guidewire kept in the target loop, a second stent can be deployed safely under peritonoscopy and fluoroscopy guidance[60].
Delayed intestinal perforation, caused by LAMS, were reported which was related with indwelling time[61,62]. Although the manufacturer recommends removal of the LAMS within 60 d of placement, this period is theoretical as no study has evaluated the optimal indwelling time. The stent indwelling time was different, depending on causes of GOO. For malignant GOO, palliative stents should be left in place for as long as possible. For diseases that may be reversible, such as GOO due to acute pancreatitis, where the pancreatitis may resolve after treatment, these stents should be removed as soon as the GOO resolves. For patients with nonreversible benign GOO, there is still no data to confirm the safety of long-term use and we should be cautious.
EUS-GE is an effective method to treat GOO, even for afferent loop syndrome and EUS-GE guided interventional procedure. An increasing data has demonstrated that EUS-GE may be a more effective alternative to enteral stenting and surgical gastroenterostomy. No standardized technique of EUS-GE has been confirmed and endoscopists perform it based on their habit. Randomized controlled studies are needed to confirm the standardized technique. Because EUS-GE is initially for the treatment of malignant GOO, most of studies focused on short outcomes. With EUS-GE performed for benign GOO, the ideal indwelling time of LAMS and long-term outcomes should be studied by large-volume prospective studies. Now almost all the EUS-GE procedures are performed in the tertiary medical centers. The training model should be studied to make EUS-GE more widely used.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: El-Shabrawi MHF, Egypt; Fiori E, Italy; Martino A, Italy; Zharikov YO, Russia S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Elmeligui AM, Deshmukh A, Okasha HH, Parsa N, Tejedor-Tejada J, Nieto J. EUS-guided splenic abscess drainage using lumen apposing metal stent. Endosc Ultrasound. 2021;10:219-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Mann R, Goyal H, Perisetti A, Chandan S, Inamdar S, Tharian B. Endoscopic ultrasound-guided vascular interventions: Current insights and emerging techniques. World J Gastroenterol. 2021;27:6874-6887. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (43)] |
| 3. | Han CQ, Tang XL, Zhang Q, Nie C, Liu J, Ding Z. Predictors of pain response after endoscopic ultrasound-guided celiac plexus neurolysis for abdominal pain caused by pancreatic malignancy. World J Gastroenterol. 2021;27:69-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Flynn DJ, Memel Z, Hernandez-Barco Y, Visrodia KH, Casey BW, Krishnan K. Outcomes of EUS-guided transluminal gallbladder drainage in patients without cholecystitis. Endosc Ultrasound. 2021;10:381-386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Ramai D, Facciorusso A, Crinò SF, Adler DG. EUS-guided gastroenteric anastomosis: A first-line approach for gastric outlet obstruction? Endosc Ultrasound. 2021;10:404-405. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Anderloni A, Fugazza A, Spadaccini M, Colombo M, Gabbiadini R, Siracusano LV, Pressiani T, Repici A. Single-session EUS-guided gastroenterostomy and hepaticogastrostomy using dedicated metal stents (with videos). Endosc Ultrasound. 2021;10:214-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Binmoeller KF, Shah JN. Endoscopic ultrasound-guided gastroenterostomy using novel tools designed for transluminal therapy: a porcine study. Endoscopy. 2012;44:499-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (16)] |
| 8. | Chen YI, James TW, Agarwal A, Baron TH, Itoi T, Kunda R, Nieto J, Bukhari M, Gutierrez OB, Sanaei O, Moran R, Fayad L, Khashab MA. EUS-guided gastroenterostomy in management of benign gastric outlet obstruction. Endosc Int Open. 2018;6:E363-E368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (1)] |
| 9. | Shiomi H, Sakai A, Nakano R, Ota S, Kobayashi T, Masuda A, Iijima H. Endoscopic Ultrasound-Guided Gastroenterostomy for Afferent Loop Syndrome. Clin Endosc. 2021;54:810-817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Sakamoto Y, Hijioka S, Maruki Y, Ohba A, Nagashio Y, Okusaka T, Saito Y. Endoscopic ultrasound-guided gastroenterostomy using a metal stent for the treatment of afferent loop syndrome. Endoscopy. 2019;51:E153-E155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Taunk P, Cosgrove N, Loren DE, Kowalski T, Siddiqui AA. Endoscopic ultrasound-guided gastroenterostomy using a lumen-apposing self-expanding metal stent for decompression of afferent loop obstruction. Endoscopy. 2015;47 Suppl 1:E395-E396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Barakat MT, Adler DG. EUS-directed transgastric ERCP: A first-line option for ERCP following Roux-en-Y gastric bypass. Endosc Ultrasound. 2021;10:151-153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Ghandour B, Bejjani M, Zhang L, Khashab MA. EUS-directed transgastric ERCP in Roux-en-Y gastric bypass revision of sleeve gastrectomy. VideoGIE. 2022;7:247-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Kedia P, Tarnasky PR, Nieto J, Steele SL, Siddiqui A, Xu MM, Tyberg A, Gaidhane M, Kahaleh M. EUS-directed Transgastric ERCP (EDGE) Versus Laparoscopy-assisted ERCP (LA-ERCP) for Roux-en-Y Gastric Bypass (RYGB) Anatomy: A Multicenter Early Comparative Experience of Clinical Outcomes. J Clin Gastroenterol. 2019;53:304-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 101] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 15. | Ghandour B, Shinn B, Dawod QM, Fansa S, El Chafic AH, Irani SS, Pawa R, Gutta A, Ichkhanian Y, Paranandi B, Pawa S, Al-Haddad MA, Zuchelli T, Huggett MT, Bejjani M, Sharaiha RZ, Kowalski TE, Khashab MA; EDGI study group. EUS-directed transgastric interventions in Roux-en-Y gastric bypass anatomy: a multicenter experience. Gastrointest Endosc. 2022;96:630-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 16. | Nguyen NQ, Hamerski CM, Nett A, Watson RR, Rigopoulos M, Binmoeller KF. Endoscopic ultrasound-guided gastroenterostomy using an oroenteric catheter-assisted technique: a retrospective analysis. Endoscopy. 2021;53:1246-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Collin A, Brahmia S, Rostain F, Lupu A, Calavas L, Jacques J, Pioche M. Endoscopic ultrasound-guided gastroenterostomy with water-jet filling technique through a 19G needle to treat complete malignant duodenal obstruction. Endoscopy. 2021;53:E7-E8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Miller CS, Chen YI, Haito Chavez Y, Alghamdi A, Zogopoulos G, Bessissow A. Double-balloon endoscopic ultrasound-guided gastroenterostomy: simplifying a complex technique towards widespread use. Endoscopy. 2020;52:151-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Consiglieri CF, Luna-Rodriguez D, Garcia-Sumalla A, Maisterra S, Velasquez-Rodriguez JG, Gornals JB. Direct endoscopic ultrasound-guided gastroenterostomy using a feeding-tube waterjet system: a teaching video to facilitate understanding of the technique. Endoscopy. 2022;54:E447-E448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Xu G, Shen Y, Lv Y, Zhou X, Li W, Wang Y, Hassan S, Wang L, Zou X. Safety and efficacy of endoscopic ultrasound-guided gastroenterostomy using double balloon occlusion methods: a clinical retrospective study in 36 patients with malignant gastric outlet obstruction. Endosc Int Open. 2020;8:E1690-E1697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Guacho JAL, Flor MM, Ferreira MTGB, Perez CA, Martins BDC, Maluf-Filho F. Endoscopic ultrasonography-guided double-balloon-occluded gastrojejunostomy bypass (EPASS) for malignant gastric outlet obstruction. Endoscopy. 2022;54:E441-E442. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Tarantino I, Ligresti D, Barresi L, Curcio G, Granata A, Traina M. One-step, exchange-free, single-balloon-assisted endoscopic ultrasound-guided gastroenterostomy with lumen-apposing metal stent in malignant gastric outlet obstruction. Endoscopy. 2017;49:E92-E94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Wang G, Liu X, Wang S, Ge N, Guo J, Sun S. Saline with methylene blue-assisted endoscopic ultrasound-guided gastrojejunostomy using a double-flared fully covered metal stent. Endoscopy. 2018;50:E17-E19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Itoi T, Itokawa F, Uraoka T, Gotoda T, Horii J, Goto O, Moriyasu F, Moon JH, Kitagawa Y, Yahagi N. Novel EUS-guided gastrojejunostomy technique using a new double-balloon enteric tube and lumen-apposing metal stent (with videos). Gastrointest Endosc. 2013;78:934-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 25. | Itoi T, Ishii K, Ikeuchi N, Sofuni A, Gotoda T, Moriyasu F, Dhir V, Teoh AY, Binmoeller KF. Prospective evaluation of endoscopic ultrasonography-guided double-balloon-occluded gastrojejunostomy bypass (EPASS) for malignant gastric outlet obstruction. Gut. 2016;65:193-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 166] [Article Influence: 18.4] [Reference Citation Analysis (1)] |
| 26. | Marino A, Bessissow A, Miller C, Valenti D, Boucher L, Chaudhury P, Barkun J, Forbes N, Khashab MA, Martel M, Chen YI. Modified endoscopic ultrasound-guided double-balloon-occluded gastroenterostomy bypass (M-EPASS): a pilot study. Endoscopy. 2022;54:170-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Hu J, Wang G, Zhang K, Ge N, Wang S, Guo J, Liu X, Sun S. Retrieval anchor-assisted endoscopic ultrasound-guided gastroenterostomy for gastric outlet obstruction. Scand J Gastroenterol. 2020;55:865-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 28. | Hu J, Zhang K, Sun S. Endoscopic ultrasound-guided retrievable puncture anchor-assisted gastroenterostomy. Dig Endosc. 2019;31:e11-e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Wang GX, Zhang K, Sun SY. Retrievable puncture anchor traction method for endoscopic ultrasound-guided gastroenterostomy: A porcine study. World J Gastroenterol. 2020;26:3603-3610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | van Wanrooij RLJ, Bronswijk M, Kunda R, Everett SM, Lakhtakia S, Rimbas M, Hucl T, Badaoui A, Law R, Arcidiacono PG, Larghi A, Giovannini M, Khashab MA, Binmoeller KF, Barthet M, Pérez-Miranda M, van Hooft JE, van der Merwe SW. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy. 2022;54:310-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 104] [Article Influence: 34.7] [Reference Citation Analysis (1)] |
| 31. | Fabbri C, Binda C, Fugazzola P, Sbrancia M, Tomasoni M, Coluccio C, Jung CFM, Prosperi E, Agnoletti V, Ansaloni L. Hybrid gastroenterostomy using a lumen-apposing metal stent: a case report focusing on misdeployment and systematic review of the current literature. World J Emerg Surg. 2022;17:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 32. | Bronswijk M, van Malenstein H, Laleman W, Van der Merwe S, Vanella G, Petrone MC, Arcidiacono PG. EUS-guided gastroenterostomy: Less is more! The wireless EUS-guided gastroenterostomy simplified technique. VideoGIE. 2020;5:442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (1)] |
| 33. | Fischer H, Rüther K, Abdelhafez M, Götzberger M, Dollhopf M, Schlag C. Technical feasibility and clinical success of direct "free hand" EUS-guided gastroenterostomy in patients with gastric outlet obstruction. Endosc Int Open. 2022;10:E1358-E1363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 34. | Basha J, Lakhtakia S, Yarlagadda R, Nabi Z, Gupta R, Ramchandani M, Chavan R, Jagtap N, Asif S, Rao GV, Reddy N. Gastric outlet obstruction with ascites: EUS-guided gastro-enterostomy is feasible. Endosc Int Open. 2021;9:E1918-E1923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 35. | Bronswijk M, Fransen L, Vanella G, Hiele M, van der Merwe S. Successful treatment of superior mesenteric artery syndrome by endoscopic ultrasound-guided gastrojejunostomy. Endoscopy. 2021;53:204-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 36. | Iqbal U, Khara HS, Hu Y, Kumar V, Tufail K, Confer B, Diehl DL. EUS-guided gastroenterostomy for the management of gastric outlet obstruction: A systematic review and meta-analysis. Endosc Ultrasound. 2020;9:16-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 105] [Article Influence: 21.0] [Reference Citation Analysis (1)] |
| 37. | McCarty TR, Garg R, Thompson CC, Rustagi T. Efficacy and safety of EUS-guided gastroenterostomy for benign and malignant gastric outlet obstruction: a systematic review and meta-analysis. Endosc Int Open. 2019;7:E1474-E1482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 72] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 38. | Fan W, Tan S, Wang J, Wang C, Xu H, Zhang L, Liu L, Fan Z, Tang X. Clinical outcomes of endoscopic ultrasound-guided gastroenterostomy for gastric outlet obstruction: a systematic review and meta-analysis. Minim Invasive Ther Allied Technol. 2022;31:159-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 39. | Chen YI, Kunda R, Storm AC, Aridi HD, Thompson CC, Nieto J, James T, Irani S, Bukhari M, Gutierrez OB, Agarwal A, Fayad L, Moran R, Alammar N, Sanaei O, Canto MI, Singh VK, Baron TH, Khashab MA. EUS-guided gastroenterostomy: a multicenter study comparing the direct and balloon-assisted techniques. Gastrointest Endosc. 2018;87:1215-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 40. | Madanat L, Saumoy M, Sharaiha RZ. Endoscopic gastrojejunostomy - bigger is better. Endoscopy. 2018;50:E331-E332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 41. | Sobani ZA, Paleti S, Rustagi T. Endoscopic ultrasound-guided gastroenterostomy using large-diameter (20 mm) lumen apposing metal stent (LLAMS). Endosc Int Open. 2021;9:E895-E900. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 42. | Bejjani M, Ghandour B, Subtil JC, Martínez-Moreno B, Sharaiha RZ, Watson RR, Kowalski TE, Benias PC, Huggett MT, Weber T, D'Souza LS, Anderloni A, Lajin M, Khara HS, Pham KD, Pleskow D, Fabbri C, Nieto JM, Kumta NA, Pawa R, Jovani M, Khashab MA; EUS-GE Study Group. Clinical and technical outcomes of patients undergoing endoscopic ultrasound-guided gastroenterostomy using 20-mm vs. 15-mm lumen-apposing metal stents. Endoscopy. 2022;54:680-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 43. | Khashab MA, Bukhari M, Baron TH, Nieto J, El Zein M, Chen YI, Chavez YH, Ngamruengphong S, Alawad AS, Kumbhari V, Itoi T. International multicenter comparative trial of endoscopic ultrasonography-guided gastroenterostomy versus surgical gastrojejunostomy for the treatment of malignant gastric outlet obstruction. Endosc Int Open. 2017;5:E275-E281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 168] [Article Influence: 21.0] [Reference Citation Analysis (2)] |
| 44. | Bronswijk M, Vanella G, van Malenstein H, Laleman W, Jaekers J, Topal B, Daams F, Besselink MG, Arcidiacono PG, Voermans RP, Fockens P, Larghi A, van Wanrooij RLJ, Van der Merwe SW. Laparoscopic versus EUS-guided gastroenterostomy for gastric outlet obstruction: an international multicenter propensity score-matched comparison (with video). Gastrointest Endosc. 2021;94:526-536.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 83] [Article Influence: 20.8] [Reference Citation Analysis (5)] |
| 45. | Perez-Miranda M, Tyberg A, Poletto D, Toscano E, Gaidhane M, Desai AP, Kumta NA, Fayad L, Nieto J, Barthet M, Shah R, Brauer BC, Sharaiha RZ, Kahaleh M. EUS-guided Gastrojejunostomy Versus Laparoscopic Gastrojejunostomy: An International Collaborative Study. J Clin Gastroenterol. 2017;51:896-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 170] [Article Influence: 21.3] [Reference Citation Analysis (1)] |
| 46. | van Wanrooij RLJ, Vanella G, Bronswijk M, de Gooyer P, Laleman W, van Malenstein H, Mandarino FV, Dell'Anna G, Fockens P, Arcidiacono PG, van der Merwe SW, Voermans RP. Endoscopic ultrasound-guided gastroenterostomy versus duodenal stenting for malignant gastric outlet obstruction: an international, multicenter, propensity score-matched comparison. Endoscopy. 2022;54:1023-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 69] [Article Influence: 23.0] [Reference Citation Analysis (2)] |
| 47. | Ge PS, Young JY, Dong W, Thompson CC. EUS-guided gastroenterostomy versus enteral stent placement for palliation of malignant gastric outlet obstruction. Surg Endosc. 2019;33:3404-3411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 161] [Article Influence: 26.8] [Reference Citation Analysis (1)] |
| 48. | Chen YI, Itoi T, Baron TH, Nieto J, Haito-Chavez Y, Grimm IS, Ismail A, Ngamruengphong S, Bukhari M, Hajiyeva G, Alawad AS, Kumbhari V, Khashab MA. EUS-guided gastroenterostomy is comparable to enteral stenting with fewer re-interventions in malignant gastric outlet obstruction. Surg Endosc. 2017;31:2946-2952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 49. | Kumar A, Chandan S, Mohan BP, Atla PR, McCabe EJ, Robbins DH, Trindade AJ, Benias PC. EUS-guided gastroenterostomy versus surgical gastroenterostomy for the management of gastric outlet obstruction: a systematic review and meta-analysis. Endosc Int Open. 2022;10:E448-E458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 50. | Chandan S, Khan SR, Mohan BP, Shah AR, Bilal M, Ramai D, Bhogal N, Dhindsa B, Kassab LL, Singh S, Ponnada S, Nguyen AK, McDonough S, Adler DG. EUS-guided gastroenterostomy versus enteral stenting for gastric outlet obstruction: Systematic review and meta-analysis. Endosc Int Open. 2021;9:E496-E504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (1)] |
| 51. | Kerdsirichairat T, Irani S, Yang J, Brewer Gutierrez OI, Moran R, Sanaei O, Dbouk M, Kumbhari V, Singh VK, Kalloo AN, Khashab MA. Durability and long-term outcomes of direct EUS-guided gastroenterostomy using lumen-apposing metal stents for gastric outlet obstruction. Endosc Int Open. 2019;7:E144-E150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 79] [Article Influence: 13.2] [Reference Citation Analysis (1)] |
| 52. | Pausawasdi N, Rugivarodom M, Swangsri J, Ratanachu-Ek T. Pitfalls in stent deployment during EUS-guided gastrojejunostomy using Hot Axios™ (with videos). Endosc Ultrasound. 2021;10:393-395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 53. | Ghandour B, Bejjani M, Irani SS, Sharaiha RZ, Kowalski TE, Pleskow DK, Do-Cong Pham K, Anderloni AA, Martinez-Moreno B, Khara HS, D'Souza LS, Lajin M, Paranandi B, Subtil JC, Fabbri C, Weber T, Barthet M, Khashab MA; EUS-GE Study Group. Classification, outcomes, and management of misdeployed stents during EUS-guided gastroenterostomy. Gastrointest Endosc. 2022;95:80-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 76] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 54. | Tyberg A, Zerbo S, Barthet M, Sharaiha RZ, Kahaleh M. A novel technique for salvaging a dislodged lumen-apposing metal stent during creation of an endoscopic gastrojejunostomy. Gastrointest Endosc. 2016;83:254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 55. | Sanchez-Ocana R, Penas-Herrero I, Gil-Simon P, de la Serna-Higuera C, Perez-Miranda M. Natural orifice transluminal endoscopic surgery salvage of direct EUS-guided gastrojejunostomy. VideoGIE. 2017;2:346-348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 56. | Ligresti D, Amata M, Barresi L, Granata A, Traina M, Tarantino I. The lumen-apposing metal stent (LAMS)-in-LAMS technique as an intraprocedural rescue treatment during endoscopic ultrasound-guided gastroenterostomy. Endoscopy. 2019;51:E331-E332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 57. | James TW, Grimm IS, Baron TH. Intraperitoneal echoendoscopy for rescue of a gastrojejunal anastomosis. VideoGIE. 2019;4:528-529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 58. | Abdelqader A, Nasr J. Natural Orifice Transluminal Endoscopic Salvage of Dislodged Endoscopic Ultrasound-Guided Jejunogastrostomy Stent After Endoscopic Retrograde in Roux-en-Y Anatomy. Am J Gastroenterol. 2019;114:1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 59. | Rizzo GEM, Carrozza L, Tammaro S, Ligresti D, Traina M, Tarantino I. Complete intraperitoneal maldeployment of a lumen-apposing metal stent during EUS-guided gastroenteroanastomosis for malignant gastric outlet obstruction: rescue retrieval with peritoneoscopy through natural orifice transluminal endoscopic surgery. VideoGIE. 2023;8:310-312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 60. | Bazaga S, Garcia-Sumalla A, Laquente B, Gornals JB. Intraperitoneal endoscopic salvage using an enteral stent for a misdeployed lumen-apposing metal stent during endoscopic ultrasound-guided gastroenterostomy. Endoscopy. 2022;54:E232-E233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 61. | McKinley W, Ayoub F, Prakash P, Shammugarajah K, Siddiqui UD. Delayed small-bowel perforation after EUS-guided gastroenterostomy. Gastrointest Endosc. 2022;95:806-807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 62. | Taibi A, Durand Fontanier S, Derbal S, Lepetit H, Christou N, Fredon F, Mathonnet M, Jacques J. What is the ideal indwelling time for metal stents after endoscopic ultrasound-guided gastrojejunostomy? Case report of delayed iatrogenic perforation with a review of the literature. Dig Endosc. 2020;32:816-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |