Published online Aug 16, 2022. doi: 10.4253/wjge.v14.i8.474
Peer-review started: February 15, 2022
First decision: April 12, 2022
Revised: May 14, 2022
Accepted: July 22, 2022
Article in press: July 22, 2022
Published online: August 16, 2022
Processing time: 180 Days and 16.7 Hours
Lower gastrointestinal bleeds (LGIB) is a very common inpatient condition in the United States. Gastrointestinal bleeds have a variety of presentations, from minor bleeding to severe hemorrhage and shock. Although previous studies investigated the efficacy of colonoscopy in hospitalized patients with LGIB, there is limited research that discusses disparities in colonoscopy utilization in patients with LGIB in urban and rural settings.
To investigate the difference in utilization of colonoscopy in lower gastrointestinal bleeding between patients hospitalized in urban and rural hospitals.
This is a retrospective cohort study of 157748 patients using National Inpatient Sample data and the Healthcare Cost and Utilization Project provided by the Agency for Healthcare Research and Quality. It includes patients 18 years and older hospitalized with LGIB admitted between 2010 and 2016. This study does not differentiate between acute and chronic LGIB and both are included in this study. The primary outcome measure of this study was the utilization of colonoscopy among patients in rural and urban hospitals admitted for lower gastrointestinal bleeds; the secondary outcome measures were in-hospital mortality, length of stay, and costs involved in those receiving colonoscopy for LGIB. Statistical analyses were all performed using STATA software. Logistic regression was used to analyze the utilization of colonoscopy and mortality, and a generalized linear model was used to analyze the length of stay and cost.
Our study found that 37.9% of LGIB patients at rural hospitals compared to approximately 45.1% at urban hospitals received colonoscopy, (OR = 0.730, 95%CI: 0.705-0.7, P > 0.0001). After controlling for covariates, colonoscopies were found to have a protective association with lower in-hospital mortality (OR = 0.498, 95%CI: 0.446-0.557, P < 0.0001), but a longer length of stay by 0.72 d (95%CI: 0.677-0.759 d, P < 0.0001) and approximately $2199 in increased costs.
Although there was a lower percentage of LGIB patients that received colonoscopies in rural hospitals compared to urban hospitals, patients in both urban and rural hospitals with LGIB undergoing colonoscopy had decreased in-hospital mortality. In both settings, benefit came at a cost of extended stay, and higher total costs.
Core Tip: Colonoscopy utilization is lower in rural hospitals than in urban hospitals in the United States for all acute and chronic lower gastrointestinal bleeding. Patients in both rural and urban hospitals who present with lower gastrointestinal bleeds that undergo colonoscopy have decreased in-hospital mortality, an extended length of hospital stay, and higher total costs.
- Citation: Ganta N, Aknouk M, Alnabwani D, Nikiforov I, Bommu VJL, Patel V, Cheriyath P, Hollenbeak CS, Hamza A. Disparities in colonoscopy utilization for lower gastrointestinal bleeding in rural vs urban settings in the United States. World J Gastrointest Endosc 2022; 14(8): 474-486
- URL: https://www.wjgnet.com/1948-5190/full/v14/i8/474.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i8.474
Gastrointestinal (GI) bleeding is the most common cause of hospitalization due to gastrointestinal disease in the United States and is responsible for 2%-4% of hospital mortality[1]. Approximately 30% to 40% of all cases of GI bleeding are from a lower GI source[2]. Over the past decade, there has been a progressive change in GI bleeding patterns that lead to hospitalization, with a clear decreasing trend in upper GI events and a significant increase in lower GI events[3]. Unfortunately, even though lower gastrointestinal bleeding (LGIB) is a common indication for admission to the hospital, it has received relatively little attention in the literature[4]. The estimated hospitalization rate for LGIB is 33-87 per 100000 population[3] with mortality rates of 2%-4% during hospitalization and rebleeding rates of 13%-19% after one year[4] . Diverticular bleeds are the leading cause of LGIB and account for approximately 30%-50% of all cases[5]. In patients 50 years or younger, the leading cause of LGIB is hemorrhoids, which often present as minor bleeding. Increased incidence of LGIB with age is likely secondary to increased diverticulosis and angiodysplasia[1]. Other conditions that are commonly associated with LGIB include angiodysplasia, ischemic colitis, colon cancer/polyps, post-polypectomy bleeding, inflammatory bowel disease, solitary rectal ulcer, radiation colitis/proctitis, and rectal varices[6]. Colonoscopy is a minimally invasive procedure that improves clinical outcomes which include- decreased rebleeding, decreased duration of hospital stay, and decreased need for major surgery[7].
Primary intervention in diagnosing LGIB is receiving a colonoscopy and it is important that the procedure is performed with minimal delay[8]. Currently the large majority of diagnostic and therapeutic procedures in Gastroenterology is the colonoscopy. In 2015, approximately 11.5 million colonoscopies were performed compared to 6.1 million upper endoscopies and a significantly lower rate of flex sigmoidoscopies at 313000 annually[2]. Urgent Golytely preparation and colonoscopy is the most direct and cost effective approach to diagnose hematochezia[7].
Several factors might contribute to rural-urban disparities in utilizing colonoscopy. Major factors may be rural provider distribution and scarcity, challenges that have persisted despite significant attempts by federal and state governments to address them over the last three decades[9]. The increased disparity is also linked to fewer specialist visits and a greater reliance on generalists in rural regions. Therefore, examining differences in rural hospitals and the benefits of colonoscopy among patients with lower gastrointestinal bleeds can lead to better patient outcomes.
This study is aimed to determine whether there were rural disparities in colonoscopy utilization in hospitalized patients with lower GI bleeding (LGIB) and the benefits of receiving a colonoscopy.
This is a retrospective cohort study.
Data used in this study were from the National Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), provided by the Agency for Healthcare Research and Quality (AHRQ). The NIS is the most extensive all-payer administrative discharge data set in the US and contains information on discharges from community hospitals[10]. Cohorts of hospitalized patients can be identified in the NIS using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9) codes for the third quarter of 2015 and earlier, and International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) codes for the fourth quarter of 2015 and later.
This study examined 157748 patients from the United States aged 18 and older in the NIS hospitalized with a principal diagnosis of LGIB between 2010 and 2016. There is no differentiation between acute or chronic bleeding. The algorithm described by Strate et al[4] was used to define the cohort. While Strate et al[4] defines a cohort of patients with LGIB ICD-9 diagnosis and procedure codes, the general equivalence mappings (GEM) from the Centers for Medicare and Medicaid Services (CMS) were used to extend their algorithm to ICD-10 diagnosis and procedural classification system (PCS) codes[11-13].
Patients with a principal ICD-9 diagnosis code indicating lower gastrointestinal bleeding were included in the cohort, including 562.12 (Diverticulosis of colon with hemorrhage), 562.13 (Diverticulitis of colon with hemorrhage), 569.85 (Angiodysplasia of the intestine with bleeding), 569.3 (Hemorrhage of rectum and anus), 455.2 (Internal hemorrhoids with other complication), 455.5 (External hemorrhoids with further complication) and 455.8 (Unspecified hemorrhoids with other complication). We also included patients with a secondary ICD-9 code that indicated a source of bleeding in the lower gastrointestinal tract (Supplementary material). Furthermore, patients were excluded if the source of bleeding appeared to be in the upper gastrointestinal tract or if they had an ICD-9 procedure code or ICD-10 PCS code suggestive of a surgical procedure in the upper gastrointestinal tract or small intestine. ICD-9 diagnosis and procedure codes were used for inclusion or exclusion criteria, and comparable ICD-10 codes are listed in Supplementary material. Since we have based our study on administrative data obtained from NIS, which is further based purely on ICD codes, we cannot comment with certainty as to the clinical details on why colonoscopy was not done in some patients with LGIB and if any other diagnostics were used. A study based on a medical chart review would be able to better answer the questions related to the final diagnosis or cause of LGIB or why colonoscopy was not done in some patients, and we would definitely want to conduct a study in the future to analyze these details.
The primary outcome of this study was the utilization of colonoscopy. This was identified using a principle or secondary ICD-9 procedure code of 45.23 (colonoscopy) or a principle or secondary ICD-10 PCS code of 0DJD8ZZ (Inspection of Lower Intestinal Tract, Via Natural or Artificial Opening Endoscopic). In addition, three secondary outcomes were studied, including in-hospital mortality, length of stay, and costs. Length of stay was defined as total days from admission to discharge or death. Costs were estimated from the hospital perspective from hospital-level ratios of costs-to-charges. All charges were adjusted to the year 2018 US dollars using the medical care component of the consumer price index.
All multivariable analyses controlled for the patient and hospital characteristics. Models controlled for age (18-64, 65-74, 75-84, 85+), sex (male, female), race (white, black, Hispanic, Asian, other), and primary payer (Medicare, Medicaid, commercial, other). We controlled the size of the hospital (small, medium, large) and the teaching status of the hospital. Teaching hospitals have at least one Accreditation Council for Graduate Medical Education (ACGME) approved residency program or are members of the Council of Teaching Hospitals (COTH). Comorbidities were controlled using the Charlson Comorbidity Index, a weighted index of 17 comorbidities[14,15]. Finally, we controlled for the geography of the hospital (rural, urban). Geography was based on the county where the hospital is located. Rural hospitals were identified as those located in counties with a core-based statistical area designated as micropolitan or non-core. This classification of rural-urban is based on the site’s zip code.
Statistical analyses were designed to determine whether there was a significant association between rural hospital designation and utilization of colonoscopy among patients admitted for gastrointestinal bleeding. In addition, we tested whether patients who received colonoscopy had significantly different rates of in-hospital mortality, length of hospital stay, and hospital costs. Characteristics of patients were compared between those who received care at rural vs urban hospitals using t-tests for continuous variables and chi-square tests for binary and categorical variables. Utilization of colonoscopy was modeled using logistic regression, controlling for patient and hospital characteristics. Mortality was also modeled using logistic regression. Length of stay and costs were modeled using linear regression, controlling for patient and hospital characteristics. A propensity score analysis matched patients who received care at a rural hospital to those at an urban hospital. Matching was performed using a 1:1 nearest neighbor approach and a caliper restriction of 0.2 times the standard deviation. Statistical analyses were performed using STATA software (version 15, College Station, TX, United States). Statistical significance was defined as P < 0.05.
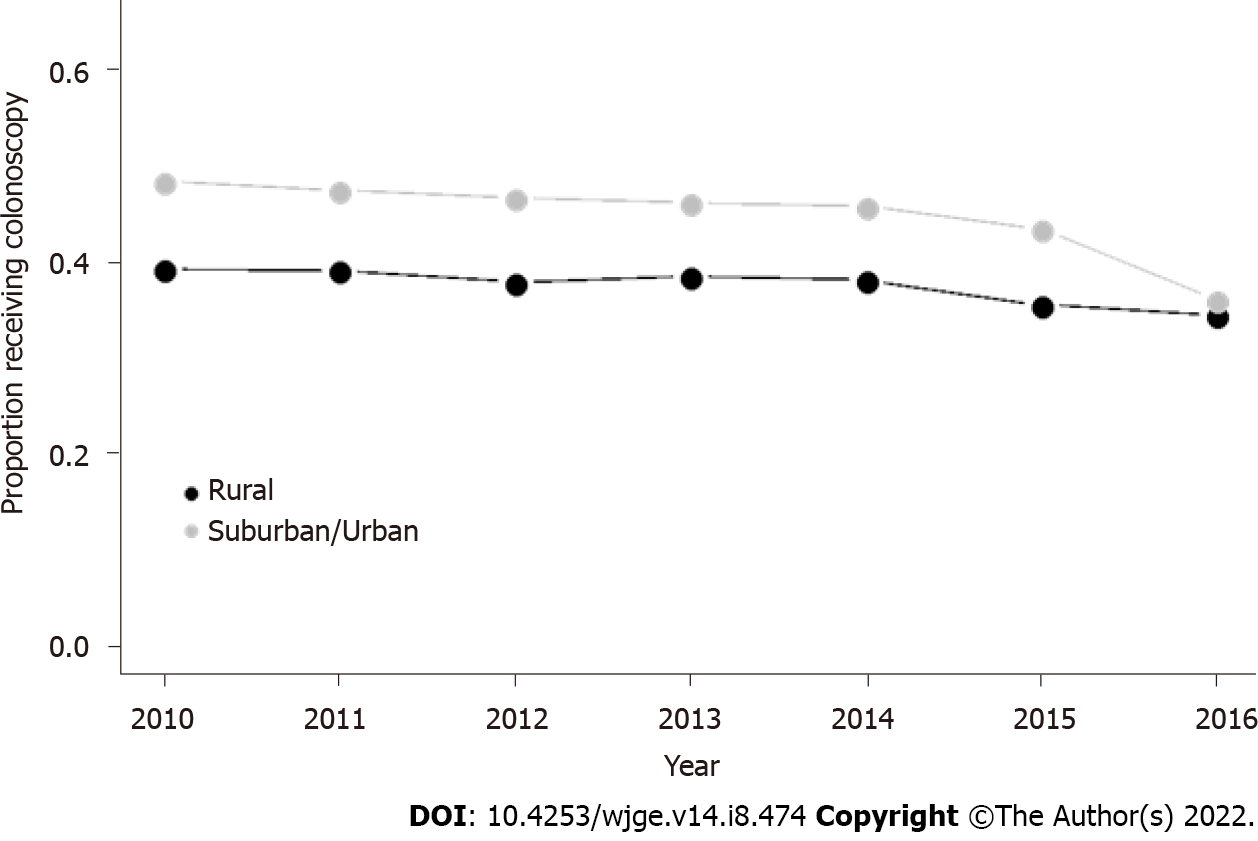
Rates of colonoscopy utilization stratified by rurality are presented in Figure 1. Approximately 37.9% of patients with lower gastrointestinal bleeding received colonoscopy at rural hospitals compared to 45.1% at urban hospitals. Rural hospitals had a consistently lower rate of colonoscopy utilization relative to urban hospitals from 2010 through 2015. The difference was mediated to a large degree in 2016. Also, there was a trend for decreasing colonoscopy utilization in both settings.
As seen in Table 1, patients differed significantly in demographics and comorbidities. However, much of the significance was due to the considerable sample size. For example, patients treated at rural hospitals tended to be slightly older (74.4 years vs 73.0 years, P < 0.0001), more likely to be female (53.7% vs 51.9%, P < 0.0001), and significantly more likely to be white (74.6% vs 63.9%). Instead of other payers, they were more likely to be insured by Medicare (78.8% vs 74.3%). Hospital characteristics also differed significantly. For example, all rural hospitals are non-teaching hospitals, and bed size varies by region and rurality in the NIS[10]. A large hospital in a rural area in the Northeast has 100 or more beds, while a large, urban teaching hospital has 425 or more beds. A large hospital in a rural area in the West has 45 or more beds, while a large, urban teaching hospital has 325 or more beds.
| Variable | Urban (n = 141571) | Rural (n = 16177) | P value |
| Age | 73.01 | 74.35 | < 0.0001 |
| 18-64 | 24.2% | 20.3% | |
| 65-74 | 22.2% | 22.3% | |
| 75-84 | 27.6% | 29.6% | |
| 85+ | 22.9% | 24.5% | |
| Sex | < 0.0001 | ||
| Male | 48.1% | 46.3% | |
| Female | 51.9% | 53.7% | |
| Race | < 0.0001 | ||
| White | 63.9% | 74.6% | |
| Black | 18.5% | 10.8% | |
| Hispanic | 8.2% | 2.3% | |
| Asian | 2.7% | 1.9% | |
| Other | 2.1% | 1.0% | |
| Missing | 4.6% | 9.4% | |
| Payer | < 0.0001 | ||
| Medicare | 74.3% | 78.8% | |
| Medicaid | 5.4% | 4.3% | |
| Commercial | 16.0% | 12.4% | |
| Other | 4.3% | 4.4% | |
| Missing | 0.1% | 0.3% | |
| Comorbidities | |||
| Number | 1.38 | 1.32 | < 0.0001 |
| Charlson index | 1.89 | 1.77 | < 0.0001 |
| Colonoscopy | < 0.0001 | ||
| Yes | 45.1% | 37.9% | |
| No | 54.9% | 62.1% | |
| Hospital bed size | < 0.0001 | ||
| Small | 15.5% | 10.8% | |
| Medium | 29.5% | 18.9% | |
| Large | 54.9% | 70.2% | |
| Region | < 0.0001 | ||
| Northeast | 33.2% | 21.8% | |
| Midwest | 44.2% | 20.8% | |
| South | 50.0% | 39.9% | |
| West | 28.4% | 17.4% | |
| Teaching | < 0.0001 | ||
| No | 45.5% | 100.0% | |
| Yes | 54.5% | 0.0% |
After controlling for other factors, patients treated at rural hospitals had 27% lower odds of receiving colonoscopy relative to patients treated at urban hospitals (OR = 0.73, P < 0.0001) (Table 2). There were several other factors associated with receiving a colonoscopy. For example, women had 4.4% lower odds of receiving colonoscopy (OR = 0.96, P < 0.0001), and non-white patients were more likely to receive a colonoscopy. Patients with more comorbidities were less likely to receive colonoscopy; each additional one-point increase in the Charlson comorbidity index was associated with 5.1% lower odds of colonoscopy. Patients who were receiving care at small (OR = 0.90, P < 0.0001) and medium (OR = 0.92) sized hospitals were less likely to receive colonoscopy relative to patients receiving care at large hospitals.
| Variable | OR | 95%CI | P value | |
| Lower | Upper | |||
| Rural | 0.730 | 0.705 | 0.757 | < 0.0001 |
| Age | ||||
| 18-64 | Reference | |||
| 65-74 | 0.978 | 0.946 | 1.010 | 0.177 |
| 75-84 | 0.986 | 0.954 | 1.018 | 0.384 |
| 85+ | 0.826 | 0.798 | 0.855 | < 0.0001 |
| Sex | ||||
| Male | Reference | |||
| Female | 0.956 | 0.937 | 0.976 | < 0.0001 |
| Race | ||||
| White | Reference | |||
| Black | 1.224 | 1.191 | 1.258 | < 0.0001 |
| Hispanic | 1.206 | 1.160 | 1.253 | < 0.0001 |
| Asian | 1.222 | 1.148 | 1.301 | < 0.0001 |
| Other | 1.158 | 1.078 | 1.244 | < 0.0001 |
| Missing | 1.107 | 1.057 | 1.159 | < 0.0001 |
| Payer | ||||
| Medicare | Reference | |||
| Medicaid | 0.986 | 0.938 | 1.037 | 0.590 |
| Commercial | 1.068 | 1.034 | 1.103 | < 0.0001 |
| Other | 1.076 | 1.020 | 1.135 | 0.007 |
| Missing | 0.763 | 0.579 | 1.004 | 0.053 |
| Hospital bed size | ||||
| Small | 0.899 | 0.873 | 0.925 | < 0.0001 |
| Medium | 0.919 | 0.898 | 0.940 | < 0.0001 |
| Large | Reference | |||
| Teaching | ||||
| No | Reference | |||
| Yes | 0.951 | 0.931 | 0.972 | < 0.0001 |
| Charlson comorbidity index | 0.949 | 0.944 | 0.955 | < 0.0001 |
Patients who received colonoscopy had a significantly lower likelihood of in-hospital mortality (Table 3). After controlling for other factors, colonoscopy was associated with a 50% lower odds of mortality (OR = 0.50, P < 0.0001). In addition, patients treated at rural hospitals had a 5% greater odds of mortality (OR = 1.05, P = 0.58), but this association was not statistically significant after controlling for colonoscopy utilization. Several other factors were associated with more significant in-hospital mortality, including age and comorbidities. Other factors were protective for mortality, including the female sex, which was associated with 17% lower odds of mortality (OR = 0.83, P < 0.0001).
| Variable | OR | 95%CI | P value | |
| Lower | Upper | |||
| Rural | 1.050 | 0.888 | 1.242 | 0.567 |
| Colonoscopy | ||||
| Yes | 0.498 | 0.446 | 0.557 | < 0.0001 |
| No | Reference | |||
| Age | ||||
| 18-64 | Reference | |||
| 65-74 | 0.939 | 0.780 | 1.130 | 0.504 |
| 75-84 | 1.333 | 1.121 | 1.584 | 0.001 |
| 85+ | 2.132 | 1.797 | 2.530 | < 0.0001 |
| Sex | ||||
| Male | Reference | |||
| Female | 0.828 | 0.749 | 0.915 | < 0.0001 |
| Race | ||||
| White | Reference | |||
| Black | 0.961 | 0.835 | 1.106 | 0.579 |
| Hispanic | 0.694 | 0.556 | 0.867 | 0.001 |
| Asian | 1.063 | 0.784 | 1.443 | 0.693 |
| Other | 0.960 | 0.665 | 1.385 | 0.826 |
| Missing | 0.944 | 0.750 | 1.187 | 0.621 |
| Payer | ||||
| Medicare | Reference | |||
| Medicaid | 0.941 | 0.718 | 1.235 | 0.662 |
| Commercial | 0.834 | 0.695 | 1.002 | 0.052 |
| Other | 0.774 | 0.556 | 1.077 | 0.129 |
| Missing | 0.538 | 0.074 | 3.905 | 0.540 |
| Hospital bed size | ||||
| Small | 0.911 | 0.786 | 1.057 | 0.218 |
| Medium | 0.966 | 0.862 | 1.083 | 0.552 |
| Large | Reference | |||
| Teaching | ||||
| No | Reference | |||
| Yes | 0.987 | 0.887 | 1.099 | 0.813 |
| Charlson comorbidity index | 1.239 | 1.215 | 1.263 | < 0.0001 |
Utilization of colonoscopy was associated with a longer length of hospital stay of 0.72 days (P < 0.0001) (Table 4). In addition, patients treated at rural hospitals had a shorter stay of 0.37 d (P < 0.0001). Colonoscopy was also associated with higher hospital costs. Patients treated at rural hospitals incurred lower costs of $853 (P < 0.001) independent of colonoscopy. Patients admitted for lower gastrointestinal bleeding who received colonoscopy incurred an additional $2,199 in costs (P < 0.0001) (Table 5).
| Variable | Coefficient | 95%CI | P value | |
| Lower | Upper | |||
| Rural | -0.372 | -0.444 | -0.300 | < 0.0001 |
| Colonoscopy | ||||
| Yes | 0.718 | 0.677 | 0.759 | < 0.0001 |
| No | Reference | |||
| Age | ||||
| 18-64 | Reference | |||
| 65-74 | 0.133 | 0.066 | 0.201 | < 0.0001 |
| 75-84 | 0.382 | 0.315 | 0.449 | < 0.0001 |
| 85+ | 0.518 | 0.448 | 0.588 | < 0.0001 |
| Sex | ||||
| Male | Reference | |||
| Female | 0.067 | 0.026 | 0.109 | 0.001 |
| Race | ||||
| White | Reference | |||
| Black | 0.590 | 0.534 | 0.646 | < 0.0001 |
| Hispanic | 0.016 | -0.064 | 0.095 | 0.699 |
| Asian | -0.041 | -0.169 | 0.088 | 0.534 |
| Other | 0.091 | -0.057 | 0.238 | 0.227 |
| Missing | -0.183 | -0.277 | -0.089 | < 0.0001 |
| Payer | ||||
| Medicare | Reference | |||
| Medicaid | -0.047 | -0.150 | 0.055 | 0.367 |
| Commercial | -0.386 | -0.453 | -0.319 | < 0.0001 |
| Other | -0.403 | -0.513 | -0.292 | < 0.0001 |
| Missing | -0.079 | -0.631 | 0.473 | 0.779 |
| Hospital bed size | ||||
| Small | -0.451 | -0.511 | -0.391 | < 0.0001 |
| Medium | -0.235 | -0.283 | -0.188 | < 0.0001 |
| Large | Reference | |||
| Teaching | ||||
| No | Reference | |||
| Yes | 0.297 | 0.253 | 0.341 | < 0.0001 |
| Charlson comorbidity index | 0.232 | 0.221 | 0.243 | < 0.0001 |
| Intercept | 3.173 | 3.097 | 3.249 | < 0.0001 |
| Variable | Coefficient | 95%CI | P value | |
| Lower | Upper | |||
| Rural | -$853.03 | -$1059.62 | -$646.44 | < 0.0001 |
| Colonoscopy | ||||
| Yes | $2198.68 | $2080.08 | $2317.27 | < 0.0001 |
| No | Reference | |||
| Age | ||||
| 18-64 | Reference | |||
| 65-74 | $353.75 | $159.71 | $547.79 | < 0.0001 |
| 75-84 | $569.47 | $377.06 | $761.87 | < 0.0001 |
| 85+ | $184.80 | -$16.82 | $386.42 | 0.072 |
| Sex | ||||
| Male | Reference | |||
| Female | -$487.40 | -$606.30 | -$368.49 | < 0.0001 |
| Race | ||||
| White | Reference | |||
| Black | $1065.28 | $903.76 | $1226.81 | < 0.0001 |
| Hispanic | $571.60 | $343.11 | $800.10 | < 0.0001 |
| Asian | $2228.13 | $1858.86 | $2597.39 | < 0.0001 |
| Other | $938.42 | $514.93 | $1361.92 | < 0.0001 |
| Missing | -$223.19 | -$492.88 | $46.49 | 0.105 |
| Payer | ||||
| Medicare | Reference | |||
| Medicaid | $209.94 | -$85.38 | $505.27 | 0.164 |
| Commercial | -$432.66 | -$624.55 | -$240.77 | < 0.0001 |
| Other | -$788.60 | -$1105.57 | -$471.62 | < 0.0001 |
| Missing | -1065.893 | -2652.626 | 520.839 | 0.188 |
| Hospital bed size | ||||
| Small | -$418.08 | -$590.47 | -$245.70 | < 0.0001 |
| Medium | -$305.15 | -$440.76 | -$169.54 | < 0.0001 |
| Large | Reference | |||
| Teaching | ||||
| No | Reference | |||
| Yes | $604.62 | $477.91 | $731.33 | < 0.0001 |
| Charlson comorbidity index | $601.63 | $570.19 | $633.06 | < 0.0001 |
| Intercept | $7859.86 | $7642.30 | $8077.41 | < 0.0001 |
To control for potential selection bias in patients receiving treatment at rural hospitals, a propensity score matching analysis was used to match 16177 patients treated at rural hospitals with 16177 similar patients treated at urban hospitals. After matching, there were no significant differences in inpatient or hospital characteristics. Results of the propensity score analysis confirmed the multi-variable model. In the overall (unmatched) cohort, 37.9% of patients treated at rural hospitals received a colonoscopy, while 46% of patients treated at urban hospitals received a colonoscopy (P < 0.0001). After matching, 44.7% of patients treated at urban hospitals received colonoscopy (P < 0.0001), suggesting that the utilization of colonoscopy between urban and rural hospitals is not related to patient characteristics.
Patients who present with gastrointestinal bleeds should undergo a thorough history, physical examination, lab work, and diagnostic procedure to determine the source of bleeding (upper GI tract, colon, or small bowel) and identify the pathology of the bleed. Colonoscopy is the most popular procedure for diagnosing, risk stratifying, and treating colonic bleeding[16]. It is often challenging to manage lower GI bleeding because of the wide variety of pathology that can lead to a lower gastrointestinal bleed. With advancements in endoscopic technology it is modality of choice for lower gastrointestinal bleeds as it allows for diagnosis and treatment simultaneously[17]. Approximately 15% of patients with presumed LGIB are ultimately found to have an upper GI source for their bleeding, highlighting the importance of receiving a timely colonoscopy[18].
Our study demonstrates that patients with LGIB admitted to rural hospitals are less likely to receive colonoscopy for the diagnosis and management, with an odds ratio of 0.73 (95%CI: 0.71-0.76, P < 0.0001). Results also showed that the disparity gap has narrowed over the past few years, but we should continue to improve availability of colonoscopy in rural hospitals.
Colonoscopy utilization in rural vs. urban LGIB patients could be due to several factors. One of the major factors is the lack of specialists, such as gastroenterologists, in rural hospitals. For this reason, colonoscopies in hospitals that are short on subspecialists are often performed by family medicine physicians that are trained in the procedure. Despite the lower rate of colonoscopies, the safety and quality of family physicians performing colonoscopies are highly comparable to specialists performing the same procedure[19]. These findings suggest that increasing the training opportunities for family physicians in performing colonoscopies could potentially alleviate the scarcity of subspecialists in rural hospitals. Rural provider distribution and scarcity challenges have persisted despite significant attempts by federal and state governments to address them over the last three decades[9].
Lack of insurance and the barrier of financial hardship in rural populations may also partly explain the lower rate of colonoscopies performed in rural hospitals. The disproportion of colonoscopies performed in rural vs urban hospitals does however show a downward trend after implementing the Affordable Care Act (ACA)[20]. Insufficient public transportation and increased distance and time to travel to urban hospitals to get colonoscopy and specialist health care can also explain the lower rates of colonoscopy utilization in rural patients. Access to primary care is one of the most significant determinants of up-to-date screening status. However, cost barriers and other factors such as poor broadband internet services limit rural residents' access to finding a primary provider[21].
According to the United States census bureau, in 2017, rural counties continued to have higher uninsured residents than urban areas. In entirely rural counties, 12.3% of the population lacked health insurance, compared to 11.3 percent in primarily rural counties (more than half of the people in rural areas) and 10.1 percent in most urban counties (less than half of the population in rural areas)[22]. According to the Medical Expenditure Panel Survey (MEPS), in 2014-2015, 37.0% of rural people and 33.6% of urban people aged 65 years and older were covered by medicare[23].
In a cross-sectional analysis of Center for Disease Control (CDC) data by Cole et al[24], rural residents had lower colorectal cancer screening rates (48%; 95%CI: 48%-49%) than urban residents (54%; 95 %CI: 53%- 55%) from 1998 to 2005 after accounting for demographic and health factors. However, the total number of colonoscopy or flexible sigmoidoscopy screenings increased in urban and rural populations from 1998 to 2005[24]. The rural disparity is also shown in a systematic review by Castellanos et al[21], who examined studies of patients suffering from cardiovascular diseases between 1990 and 2017. Most published clinical trials showed that patients from rural communities had significantly lower cardiac rehabilitation referral and participation rates than the general population[21].
Our study also showed that older people aged 85 years and above with LGIB were less likely to receive a colonoscopy, perhaps because current guidelines do not recommend routine screening after 75 years. Women with LGIB are less likely to receive a colonoscopy, most likely because lower GI bleeding is more common in men than in women, and men are more likely to undergo colonoscopy[25]. A study by Devani et al[26] showed that women were more likely to delay colonoscopy than males, and women were more likely to ignore bleeding than men (Table 2).
The odds of mortality were reduced in all patients who received a colonoscopy, irrespective of rural or urban location, and the mortality was not significantly different in rural and urban hospitals for patients who received a colonoscopy. This supports our observation that colonoscopy utilization is associated with decreased mortality in all patients, and thus it should be offered to all LGIB patients. As shown in our study, there is, however, a statistically significant difference in colonoscopy utilization between rural and urban hospitals. Thus, by increasing colonoscopy availability in rural hospitals, we anticipate a reduction in mortality in rural hospitals. In general, rural populations in the United States are, on average, older and sicker than their urban counterparts[27]. Our study demonstrates that patients with lower gastrointestinal bleeds who underwent colonoscopy had significantly lower mortality than those with LGIB who did not undergo colonoscopy. This effect was observed after controlling for meaningful patient and hospital characteristics (Table 3). This highlights the significant impact colonoscopy can play in patients with LGIB.
Patients aged 85 years and above with LGIB had higher mortality rates than patients aged 18-64 years. This may partly be explained by the fact that current guidelines do not recommend routine screening after the age of 75 years, and also, they have confounding prognostic factors compared to younger patients (Table 3). Other research has shown that independent predictors of in-hospital mortality include age, intestinal ischemia, comorbid illness, bleeding while hospitalized for a separate process, coagulation defects, hypovolemia, transfusion of packed red blood cells, and male gender[4].
Women with LGIB had lower mortality rates than men regardless of the treatment setting. These results were comparative to a retrospective observational study by Devani et al[26], who found that the odds of mortality were almost 17% lower in women with LGIB than in men.
Our study showed that patients with LGIB admitted to rural hospitals had 8 to 9 h (0.37 d) shorter length of hospital stay than patients admitted to urban hospitals. This can be due to the likelihood that rural populations were less likely to undergo colonoscopy, which extends admissions, as rural hospitals have fewer resources and specialists to perform colonoscopies. Rural populations may also get discharged earlier due to poor insurance benefits and higher inpatient admission costs. Most rural patients (37.01% of patients aged 65 years and older) have Medicare insurance[25] that has a prospective payment system, which pays a predetermined, fixed reimbursement to the hospital for a diagnosis irrespective of the length of stay. This payment system might prompt an earlier discharge for rural patients[28].
Patients with LGIB undergoing colonoscopy had a longer length of hospital stay by 17 h (0.72 d) than those who did not (Table 4). The length of time it takes to perform a colonoscopy is determined by the patients’ and endoscopists’ characteristics. Even though not all colonoscopies are the same, there is no distinction in the time permitted for each colonoscopy when arranging the procedure in the endoscopy suite. As a result, patient wait times vary, impacting the overall length of stay. Factors determining the length of stay (LOS) include overall time spent preparing for an operation, procedure time, insurance reimbursement, and out-of-pocket expenses, influencing hospital and patient decision-making[29].
Our study showed that rural patients with LGIB incur $853 less in costs than patients treated at urban hospitals which could be due to the fact that rural patients are less likely to undergo colonoscopy, which can be contributory to the reduction of the total inpatient admission cost.
Our study showed that patients with LGIB who undergo colonoscopy incur $2199 in higher costs than those who do not. Procedural costs and longer duration of stay for patients undergoing colonoscopy may be part of the higher costs. A cost-effectiveness analysis study comparing four diagnostic strategies in the evaluation of rectal bleeding in adults by Allen et al[30] using a Markov model showed that in addition to being associated with lower mortality, colonoscopy was also cost-effective when compared to flexible sigmoidoscopy, flexible sigmoidoscopy followed by air contrast barium enema (FS+ACBE), and simple observation. Additional research is needed to understand the value proposition of colonoscopy for LGIB other than rectal bleeding. This is perhaps because patients undergoing colonoscopy are more likely to stay longer in the hospital and spend higher costs than those who do not undergo colonoscopy. Increases in LOS per day were linked to a 47% increase in Inpatient admission costs[26]. The total cost of a colonoscopy depends on whether costs are assessed from a societal or a health system perspective[31].
One strength of the study is that we used data from NIS, HCUP, provided by the AHRQ. This is a nationally representative sample, which enhances the generalizability of our findings.
We could not account for the severity of LGIB or the screening status of patients. Also, we studied admissions between 2010 and 2016 which is the most recent database and there is not currently more recent data. A limitation is that the NIS data set is based solely on ICD-9 and ICD-10 diagnoses. Specific colonoscopy findings are not reported in the NIS data set.
Our study results demonstrated that the rate of utilization of colonoscopy was significantly lower in rural hospitals compared to urban hospitals. This study also showed that patients with lower gastrointestinal bleeds undergoing colonoscopy had significantly lower in-hospital mortality than those who did not. The study results emphasize the importance of counseling rural patients and educating them about the life-threatening complications of LGIB, which colonoscopy can avoid. Furthermore we would benefit from more access to colonoscopies in rural settings. Internal medicine and family physicians should be trained to perform colonoscopies in rural settings to increase the availability of colonoscopy in these areas. Physicians should be encouraged to improve rural population outreach, hospital resources, and reimbursement. Despite differences in colonoscopy utilization, this study did not show any significant difference in mortality between rural and urban patients with LGIB. Further studies are needed to give more insights into rural-urban disparities in mortality.
Disparities in colonoscopy access in rural and urban hospitals is an understudied topic. The significance of this study is to demonstrate whether or not improved access improves patient mortality.
To improve access to colonoscopies in the United States. We are also interested in the availability of colonoscopy and how it effects patients length of stay and costs.
To discover whether or not there is a disparity in colonoscopy utilization for lower gastrointestinal bleeds between rural and urban hospital areas in the United States. Also to determine whether there is a benefit for mortality in patients with lower gastrointestinal bleeds when they receive colonoscopies.
Retrospective cohort study and data analysis of National Inpatient Sample, Healthcare Cost and Utilization Project, provided by the Agency for Healthcare Research and Quality.
Approximately 37.9% of patients with lower gastrointestinal bleeding received colonoscopy at rural hospitals compared to 45.1% at urban hospitals. Patients treated at rural hospitals had 27% lower odds of receiving colonoscopy relative to patients treated at urban hospitals (OR = 0.73, P < 0.0001) After controlling for other factors, colonoscopy was associated with a 50% lower odds of mortality (OR = 0.50, P < 0.0001). The problem that remains to be solved is providing patients in rural hospitals access to colonoscopy so more patients can have a mortality benefit when they present with a lower gastrointestinal bleed.
This study proposes that because there is a decrease in mortality when patients receive a colonoscopy, we should improve access to colonoscopies in rural hospitals. New methods proposed are increased access to specialists and increased training opportunities for primary care providers for colonoscopies.
Future research should be aimed at determining mortality differences in patients with lower gastrointestinal bleeds that receive colonoscopy between urban and rural hospitals.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Nakeep S, Egypt; Govindarajan KK, India; Thomopoulos K, Greece S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Qayed E, Dagar G, Nanchal RS. Lower Gastrointestinal Hemorrhage. Crit Care Clin. 2016;32:241-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Peery AF, Crockett SD, Barritt AS, Dellon ES, Eluri S, Gangarosa LM, Jensen ET, Lund JL, Pasricha S, Runge T, Schmidt M, Shaheen NJ, Sandler RS. Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States. Gastroenterology. 2015;149:1731-1741.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 697] [Cited by in RCA: 704] [Article Influence: 70.4] [Reference Citation Analysis (0)] |
| 3. | Lanas A, García-Rodríguez LA, Polo-Tomás M, Ponce M, Alonso-Abreu I, Perez-Aisa MA, Perez-Gisbert J, Bujanda L, Castro M, Muñoz M, Rodrigo L, Calvet X, Del-Pino D, Garcia S. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Am J Gastroenterol. 2009;104:1633-1641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 415] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 4. | Strate LL, Ayanian JZ, Kotler G, Syngal S. Risk factors for mortality in lower intestinal bleeding. Clin Gastroenterol Hepatol. 2008;6:1004-10; quiz 955. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 166] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 5. | Cirocchi R, Grassi V, Cavaliere D, Renzi C, Tabola R, Poli G, Avenia S, Farinella E, Arezzo A, Vettoretto N, D'Andrea V, Binda GA, Fingerhut A. New Trends in Acute Management of Colonic Diverticular Bleeding: A Systematic Review. Medicine (Baltimore). 2015;94:e1710. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Strate LL, Gralnek IM. ACG Clinical Guideline: Management of Patients With Acute Lower Gastrointestinal Bleeding. Am J Gastroenterol. 2016;111:459-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 300] [Article Influence: 33.3] [Reference Citation Analysis (2)] |
| 7. | Caos A, Benner KG, Manier J, McCarthy DM, Blessing LD, Katon RM, Gogel HK. Colonoscopy after Golytely preparation in acute rectal bleeding. J Clin Gastroenterol. 1986;8:46-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 63] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Almadi MA, Barkun AN. Patient Presentation, Risk Stratification, and Initial Management in Acute Lower Gastrointestinal Bleeding. Gastrointest Endosc Clin N Am. 2018;28:363-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Hart LG, Salsberg E, Phillips DM, Lishner DM. Rural health care providers in the United States. J Rural Health. 2002;18 Suppl:211-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 99] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Hoffman RD, Danos DM, Lau FH. National health disparities in incisional hernia repair outcomes: An analysis of the Healthcare Cost and Utilization Project National Inpatient Sample (HCUP-NIS) 2012-2014. Surgery. 2021;169:1393-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 11. | Centers for Medicare and Medicaid Services. ICD-10. 2021. Available from: https://www.cms.gov/Medicare/Coding/ICD10. |
| 12. | Centers for Medicare and Medicaid Services. General Equivalence Mappings Frequently Asked Questions. 2014. Available from: https://www.cms.gov/search/cms?keys=General+Equivalence+Mappings+Frequently+Asked+Questions. |
| 13. | Rihanek T, DeVault K. Converting data to ICD-10 with GEMs: reference mapping tools will aid in system transition. J AHIMA. 2012;83:42-43. [PubMed] |
| 14. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32099] [Cited by in RCA: 38307] [Article Influence: 1008.1] [Reference Citation Analysis (0)] |
| 15. | Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7532] [Cited by in RCA: 8646] [Article Influence: 262.0] [Reference Citation Analysis (0)] |
| 16. | Ghassemi KA, Jensen DM. Lower GI bleeding: epidemiology and management. Curr Gastroenterol Rep. 2013;15:333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 17. | Strate LL. Lower GI bleeding: epidemiology and diagnosis. Gastroenterol Clin North Am. 2005;34:643-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 144] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 18. | Laine L, Shah A. Randomized trial of urgent vs. elective colonoscopy in patients hospitalized with lower GI bleeding. Am J Gastroenterol. 2010;105:2636-41; quiz 2642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 140] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 19. | Edwards JK, Norris TE. Colonoscopy in rural communities: can family physicians perform the procedure with safe and efficacious results? J Am Board Fam Pract. 2004;17:353-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Haakenstad A, Hawkins SS, Pace LE, Cohen J. Rural-urban disparities in colonoscopies after the elimination of patient cost-sharing by the Affordable Care Act. Prev Med. 2019;129:105877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Castellanos LR, Viramontes O, Bains NK, Zepeda IA. Disparities in Cardiac Rehabilitation Among Individuals from Racial and Ethnic Groups and Rural Communities-A Systematic Review. J Racial Ethn Health Disparities. 2019;6:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 22. | United States Census Bureau. Available from: https://www.census.gov/Library/stories/2019/04/health-insurance-rural-america.html. |
| 23. | Medical Expenditure Panel Survey. Insurance and Access to Care in Urban and Rural Areas, 2014-2015. Available from: https://meps.ahrq.gov/data_files/publications/st512/stat512.shtml. |
| 24. | Cole AM, Jackson JE, Doescher M. Urban-rural disparities in colorectal cancer screening: cross-sectional analysis of 1998-2005 data from the Centers for Disease Control's Behavioral Risk Factor Surveillance Study. Cancer Med. 2012;1:350-356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 114] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 25. | DiGregorio AM, Alvey H. Gastrointestinal Bleeding. [Updated July 25, 2021]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. |
| 26. | Devani K, Radadiya D, Charilaou P, Aasen T, Reddy CM, Young M, Brahmbhatt B, Rockey DC. Trends in hospitalization, mortality, and timing of colonoscopy in patients with acute lower gastrointestinal bleeding. Endosc Int Open. 2021;9:E777-E789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Centers for Disease Control and Prevention. About Rural Health. [cited November 22, 2021]. Available from: https://www.cdc.gov/ruralhealth/about.html. |
| 28. | Centers for Medicare and Medicaid Services. Prospective Payment Systems - General Information. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ProspMedicareFeeSvcPmtGen. |
| 29. | Jain D, Goyal A, Zavala S. Predicting Colonoscopy Time: A Quality Improvement Initiative. Clin Endosc. 2016;49:555-559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Allen E, Nicolaidis C, Helfand M. The evaluation of rectal bleeding in adults. A cost-effectiveness analysis comparing four diagnostic strategies. J Gen Intern Med. 2005;20:81-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Henry SG, Ness RM, Stiles RA, Shintani AK, Dittus RS. A cost analysis of colonoscopy using microcosting and time-and-motion techniques. J Gen Intern Med. 2007;22:1415-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |