Published online Jul 16, 2022. doi: 10.4253/wjge.v14.i7.424
Peer-review started: January 21, 2022
First decision: April 19, 2022
Revised: May 10, 2022
Accepted: June 24, 2022
Article in press: June 24, 2022
Published online: July 16, 2022
Processing time: 174 Days and 6.8 Hours
Current guidelines recommend not performing papillary large balloon dilation in patients with nondilated distal bile ducts.
To assess the feasibility of balloon dilation to remove difficult stones in patients with nondilated distal bile ducts.
Data from 1289 endoscopic retrograde cholangiopancreatography (ERCP) procedures were obtained from two prospective studies. While 258 cases had difficult stones (> 1 cm, multiple > 8, impacted, or having a thin distal duct), 191 underwent biliary dilation up to 15 mm after endoscopic sphincterotomy. Cholangiographies of these cases were retrospectively reviewed in order to classify the distal bile duct and both the stone size and number. Primary outcomes were clearance rate at first ERCP and complications.
Of the 191 patients (122 women and 69 men; mean age: 60 years) who underwent biliary dilation for difficult stones, 113 (59%) had a nondilated or tapered distal duct. Patients with a dilated distal duct were older than those with nondilated distal ducts (mean 68 and 52 years of age, respectively; P < 0.05), had more stones (median 4 and 2 stones per patient, respectively; P < 0.05), and had less need for additional mechanical lithotripsy (6.4% vs 25%, respectively; P < 0.05). Clearance rate at first ERCP was comparable between patients with a dilated (73/78; 94%) and nondilated distal ducts (103/113; 91%). Procedures were faster in patients with a dilated distal duct (mean 17 vs 24 min, respectively; P < 0.005). Complications were similar in both groups (6.4% vs 7.1%, respectively).
Large balloon dilation for difficult stones is feasible in patients with a nondilated or even tapered distal duct.
Core Tip: Endoscopic papillary large balloon dilation is increasingly being used in treating difficult bile duct stones, since it is faster and less laborious than mechanical lithotripsy, with comparable results in terms of safety and effectiveness. However, this method is not recommended in patients with nondilated distal ducts, due to a higher complication rate, especially perforation. This study evaluated a large cohort of difficult duct stones patients submitted to large balloon dilation and found that patients with dilated and nondilated distal ducts had similar complication rates. This study suggests that large balloon dilation may be feasible in the latter group of patients.
- Citation: Pereira Lima JC, Moresco GS, Sanmartin IDA, Contin I, Pereira-Lima G, Watte G, Altmayer S, Oliveira dos Santos CE. Feasibility of endoscopic papillary large balloon dilation to remove difficult stones in patients with nondilated distal bile ducts. World J Gastrointest Endosc 2022; 14(7): 424-433
- URL: https://www.wjgnet.com/1948-5190/full/v14/i7/424.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i7.424
Endoscopic sphincterotomy with stone extraction by balloon and/or basket is the method of choice for treating bile duct stones[1]. However, in patients with difficult bile duct stones (impacted, multiple or > 1 cm, or having a tapered distal duct), additional methods such as mechanical lithotripsy, intracorporeal lithotripsy, or papillary large balloon dilation are needed. Lithotripsy techniques, especially intracorporeal lithotripsy, which need to be guided by cholangioscopy, increase procedure time, cost, and the number of endoscopic retrograde cholangiopancreatography (ERCP) sessions required to clear the biliary tree[2]. Ersoz et al[3] pioneered the use of large balloon dilation of the distal bile duct in order to widen the pre-papillary portion of the common duct and facilitate stone retrieval.
The American Society for Gastrointestinal Endoscopy (ASGE) does not recommend papillary large balloon dilation for nondilated distal ducts because of the “increased risk of perforation”[4]. However, two Japanese studies[5,6] and another by the original technique description by Ersoz et al[3] successfully and safely employed endoscopic papillary or biliary large balloon dilation in patients with a nondilated or tapered distal bile duct. The current study analyzes the feasibility of using large balloon dilation of the distal biliary tree to remove difficult stones from patients with a nondilated distal bile duct.
Data were retrieved and analyzed from 1289 ERCPs conducted in two prospective trials during 2014-2019 that assessed post-ERCP pancreatitis (PEP) prevention[7,8]. Eligible subjects were all adults scheduled to undergo ERCP at our institution, and whose cannulation target was the biliary tree. Patients were excluded if they had non-naïve papilla, a previous ERCP at other institutions, failed bile duct cannulation, patients who primarily underwent an infundibulotomy due to an impacted stone at the papilla or papillary neoplasia, Billroth II gastrectomy, or were lost to follow up or refused to enter the studies. All patients gave signed informed consent to the procedure and inclusion in the study. Both study protocols were approved by the Research Ethics Commission of our Institution and registered in the Brazilian Protocol Registry under UTN codes U1111-1207-7823 (http://www.ensaiosclinicos
In the two randomized trials assessing post-ERCP pancreatitis prevention, 258 cases had difficult bile duct stones (≥ 8 stones, > 1 cm or impacted)[7,8]. Of these, 67 patients had the duct cleared by endoscopic sphincterotomy with or without mechanical lithotripsy and without the need for an endoscopic biliary large balloon dilation (EBLBD) since their distal ducts were wide enough to allow stone passage without balloon dilation. The remaining 191 patients underwent an EBLBD up to 15 mm after a full-length endoscopic sphincterotomy. The operator filled out a procedure evaluation form immediately after the ERCP. The research team, which was blinded to patient randomization, contacted the patients personally or by phone 48-72 h after ERCP and 15-30 d after the procedure to complete the follow-up forms. Patients who experienced post-ERCP pain or bleeding received laboratory and abdominal imaging, or endoscopic evaluation.
A nondilated or tapered distal bile duct was defined when the lower part of the biliary tract was < 8 mm in diameter and > 15 mm in length measured by cholangiography. The number of stones and the maximum diameter of each patient’s largest stone were independently verified by three of the authors of the present study. Radiographs of the 191 cases who received an EBLBD are stored in our hospital’s computer system and were retrospectively evaluated.
ERCP was performed by one of the authors who performs more than 700 ERCPs annually or by a fellow under supervision. All procedures were performed under sedation with propofol, midazolam, and fentanyl which was supervised by an anesthesiologist. Hyoscine was administered to abolish duodenal peristalsis. After the cholangiographic diagnosis of a difficult stone, a complete sphincterotomy was performed via the papillary ostium or the access obtained after pre-cut papillotomy (Jag Wire straight tip, Ultratome XL short nose 20 mm, Microknife XL, Boston Scientific Marlborough, Massachusetts, United States or Tritome triple lumen sphincterotome 25 mm, Tracer Metro Direct wire guide, Huibregtse Triple lumen needle knife 4 mm, Cook Endoscopy, Winston-Salem, NC, United States). A large dilation esophageal/pyloric balloon (CRE PRO Wireguided – esophageal, pyloric, colonic, biliary Balloon Dilatation Catheter 12-15 mm, Boston Scientific, Marlborough, Massachusetts, United States)was inserted into the bile duct and gradually inflated across the papilla at 12-15 mm (3.5-8 ATM according to the manufacturer’s recommendations), in order to try and obliterate its waist regardless of the presence of a distal situated stone, a peri-papillary diverticulum, or a nondilated distal duct. Additional upstream dilations in the duct were performed at the endoscopists’ discretion if the bile duct distal to the stone was considered not dilated enough to facilitate stone retrieval. For each dilation, the balloon was left inflated in place for 10-30 s. After the EBLBD, a retrieval balloon and/or a basket were used to remove the stones. If stone removal was incomplete, a plastic stent was left in place. Procedure time was measured in minutes from the insertion of the duodenoscope into the patient’s oral cavity to its retrieval.
The primary outcome was ERCP complications, notably perforation and pancreatitis (PEP). Secondary outcomes were clearance rate at first ERCP, procedure time, and need for mechanical lithotripsy. Procedure-related complications and severity were determined using definitions from a previously published guideline[9].
Data were presented as the frequency (percentage) or mean ± SD. The Shapiro-Wilk test was used to assess the normality of the data distribution. The Mann–Whitney test was used to compare continuous variables and a chi-square was used to compare associations between variables. Statistical significance was accepted at a two-sided significance level of 0.05. Statistical analyses were performed using STATA v.15 (STATA Corporation, College Station, Texas, United States).
Of the 191 cases with difficult bile duct stones who received an EBLBD, 122 were women (63.8%) and 69 were men, the mean age was 60 years (range, 26-93 years), and 185 were Caucasians (European-derived) and 6 were black. While 113 of the 191 cases had a nondilated or tapered distal bile duct, 78 had a large distal duct. Cases with a nondilated distal duct had fewer duct stones (mean and median = 2, range, 1-5) than patients with dilated distal ducts (mean = 4.1, median = 4, range, 1-15; P < 0.01). The main bile duct stone size was smaller in patients with nondilated than dilated distal ducts (mean 1.1 cm (range, 0.7-1.5 cm) vs 1.7 cm (range, 1.3-2.5 cm), respectively; P < 0.01). Patients with a nondilated distal duct were also significantly younger and more likely to have received mechanical lithotripsy (Table 1).
| Non-dilated DD (n = 113) | Dilated DD (n = 78) | P value | |
| Mean age (SD) | 52 ± 8 | 68 ± 11 | < 0.001 |
| Female/Male | 75/38 | 47/31 | 0.387 |
| Number of MBD stones (SD) | 2 ± 0.7 | 4.1 ± 2.9 | < 0.001 |
| Biggest MBD stone size (SD) | 1.1 ± 0.1 | 1.7 ± 0.2 | < 0.001 |
| Additional ML | 28 (25%) | 5 (6.4%) | 0.001 |
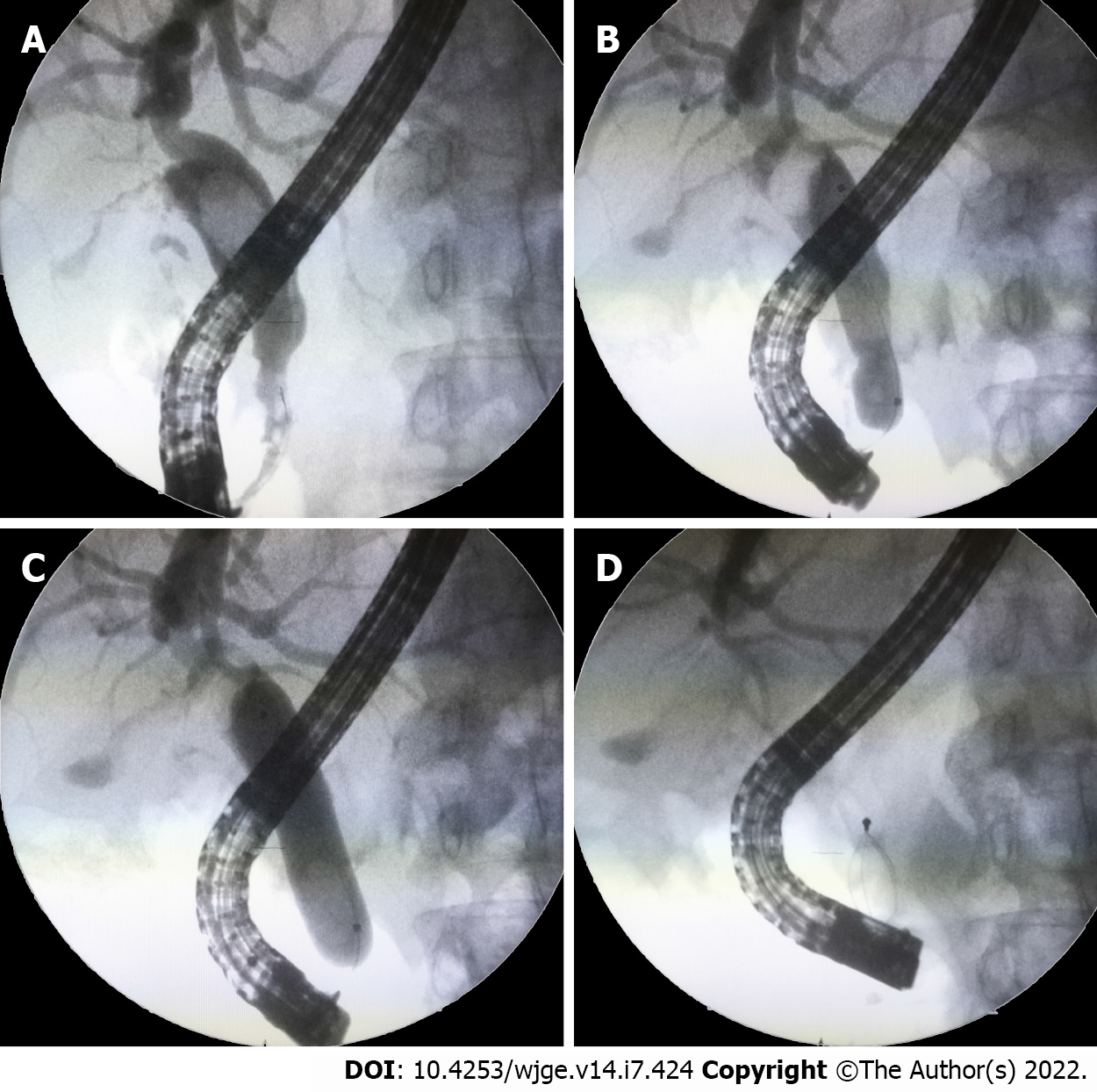
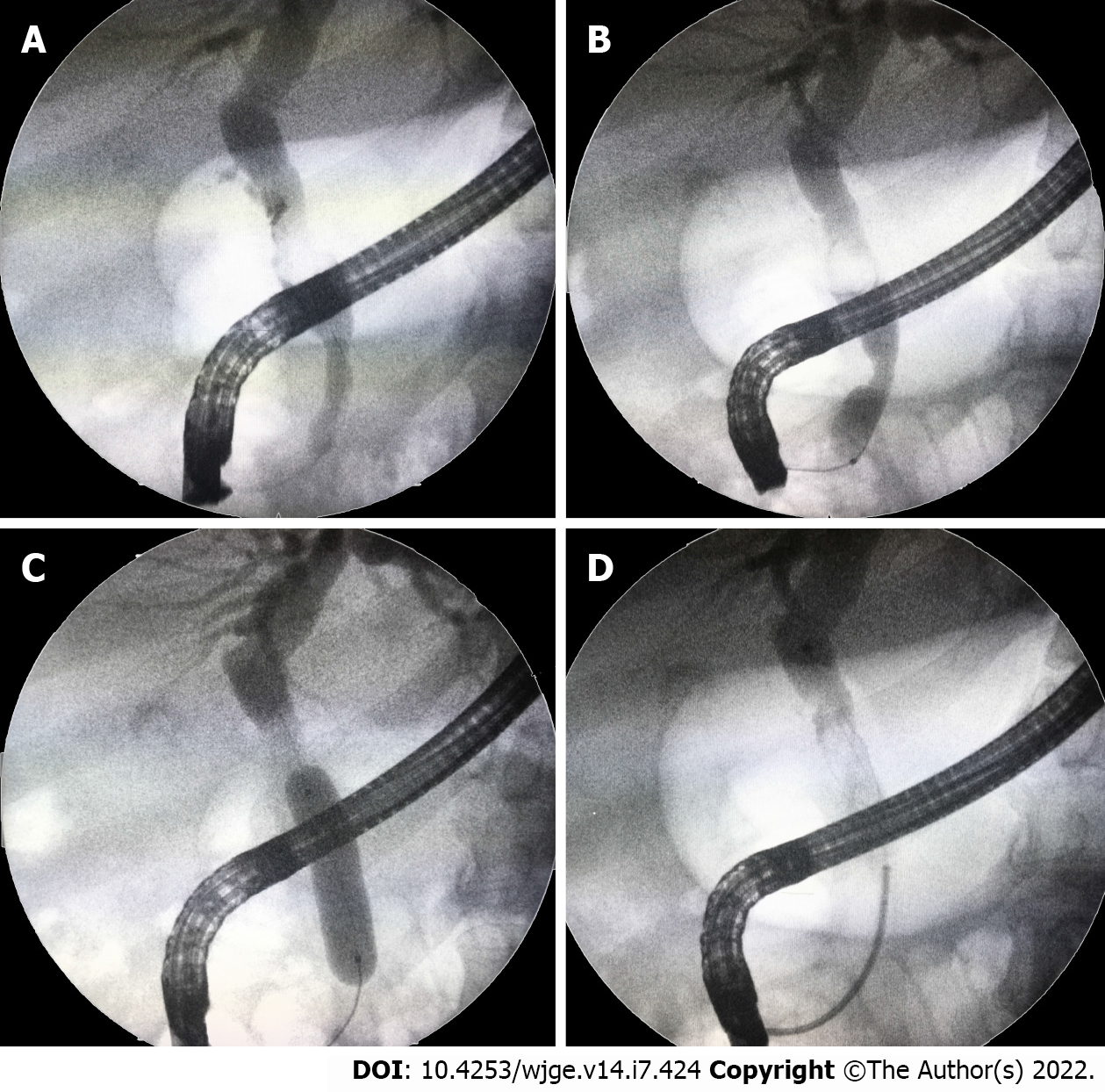
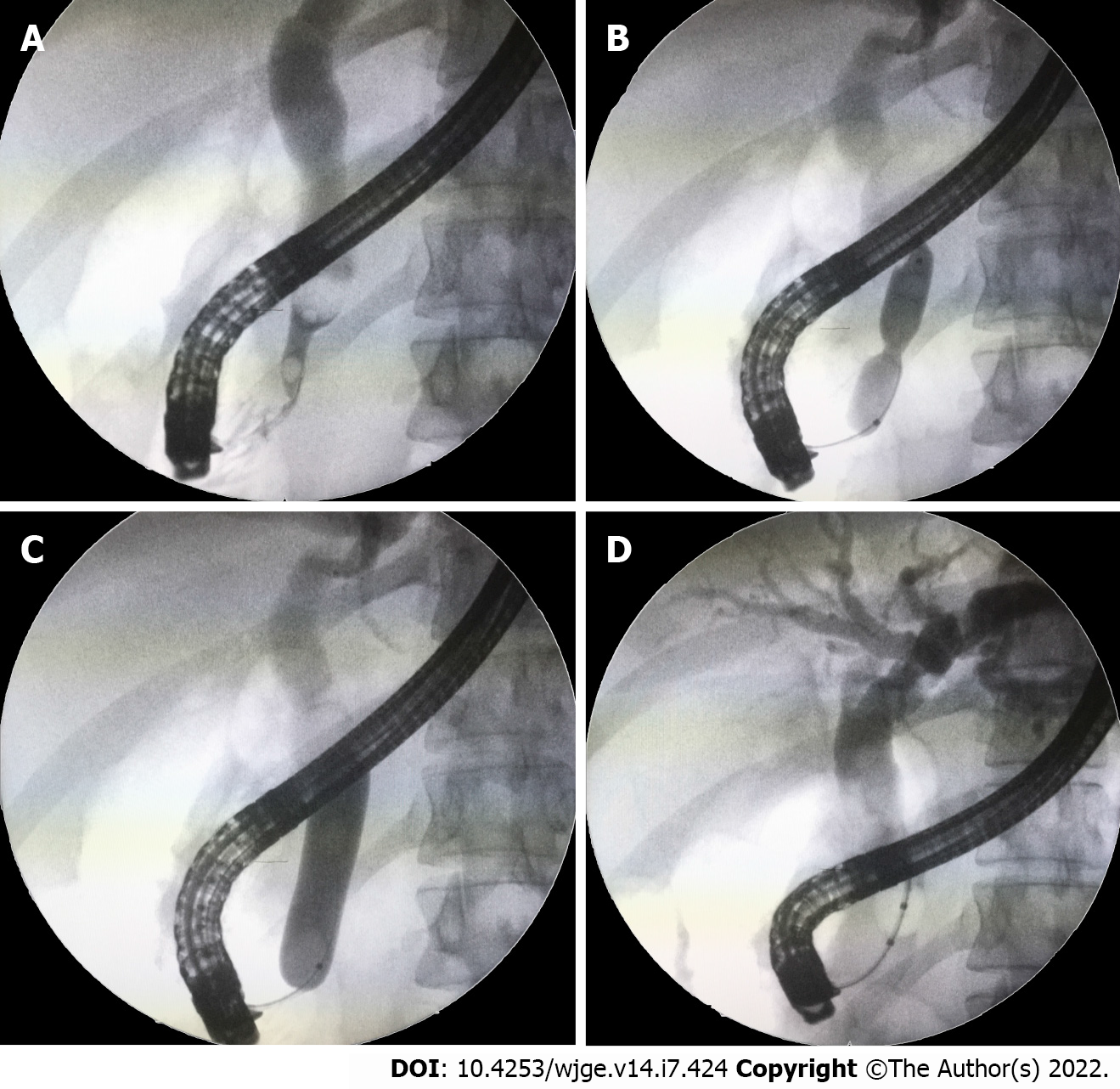
The ERCP technique is described in Figures 1-3. Figure 1 shows a patient with a long intrapancreatic choledochal segment, which was balloon dilated to widen the distal biliary tree and allow easier stone removal after lithotripsy. Figures 2 and 3 show the results from patients with long-segment nondilated distal ducts and impacted stones in the middle common duct. These individuals had large balloon dilation until waist disappearance, resulting in a faster and easier stone extraction in the same sitting.
The clearance rate at first ERCP was comparable between the two groups. Patients with a dilated distal duct had a 94% stone clearance rate (73/78 patients) and those with a nondilated distal duct had a 91% clearance rate (103/113 patients). Procedures were also faster in patients with a dilated than nondilated distal duct (mean = 17 vs 24 min, respectively; P < 0.05).
The complication rate was similar in both groups. Eight of 113 (7.1%) patients with a nondilated distal duct had complications (two had perforations, three had overt bleedings, and three had PEP), while five of the 78 (6.4%) patients with a large distal duct who received an EBLBD had complications (two had bleeding, one experienced cholangitis, and two had PEP) (Table 2). All complications were treated conservatively and no patients died from the procedure. Of five cases with a dilated distal duct and no bile duct clearance at first ERCP (with a plastic stent left in place), two underwent surgery, and three had their ducts cleared during a second ERCP using lithotripsy techniques. One of these three cases developed fever (mild cholangitis) after the second procedure. In all ten cases with a narrow distal duct for whom the first ERCP attempt failed to complete stone extraction, a second ERCP successfully achieved bile duct clearance. Ductal clearance was accomplished using another EBLBD after stent removal and lithotripsy techniques. Two patients experienced overt bleeding without the need for transfusion and two had mild cholangitis at the second ERCP.
| Non-dilated DD (n = 113) | Dilated DD (n = 78) | |
| Complication rate, n (%) | 8 (7.1) | 5 (6.4) |
| Post-ERCP pancreatitis | 3 | 2 |
| Overt bleeding | 3 | 2 |
| Perforations | 2 | - |
| Cholangitis | - | 1 |
| Death | - | - |
In this study, EBLBD up to 15 mm was shown to be feasible and safe for patients with nondilated distal ducts though there were two cases of perforation in this group. Patients with nondilated ducts had the same complication rate of those with dilated distal ducts. An ex vivo porcine model showed that biliary duct tears are caused by overdistention of narrow ducts after large balloon dilation[10]. However, studies indicate that a tear in a nondilated distal bile duct in humans does not necessarily result in a retroperitoneum or peritoneal cavity rupture because this thinner portion is located within the pancreas[10]. This is one explanation for why only two of 113 (< 2%) patients with nondilated distal bile ducts who received EBLBD experienced overt perforations. Despite physical compression resulting from balloon dilation inside the pancreatic head, PEP rates were relatively low and similar in both groups (2.7% vs 2.6% for patients with non-dilated and dilated distal bile ducts, respectively). Another possible explanation for our findings was the fact that we always dilate the bile duct and the ampullary region with balloons up to 15 mm. In a Korean study analyzing 672 EBLBD for difficult stones, perforations and fatal complications only occurred in patients dilated > 15-20 mm. No perforation was observed in patients dilated 12-15 mm[11].
ASGE guideline C level recommendation that EBLBD should not be performed in patients with a nondilated distal duct is based on one study in which three deaths occurred as a result of perforation following EBLBD and, in two of the three cases, a full incision sphincterotomy was also performed[4,12]. The guideline used the same study to recommend at evidence level of III that the maximum diameter of the balloon should not exceed that of the distal common bile duct[4,12]. Fujita et al[5] analyzed 209 cases submitted to EBLBD and found no differences in the incidence of PEP, bleeding, or perforation when comparing EBLBD in patients with and without a nondilated distal bile duct. Ersoz et al[3], the first endoscopists who employed large balloon dilation for difficult stones, evaluated 18 cases with a nondilated distal duct and 40 with a dilated distal duct in their original report. There were no cases of perforations in either group, but bleeding occurred more often in patients with a nondilated distal duct.
In patients with large stones and no distal duct dilation, a common finding in our experience, it can be more difficult and labor-intensive to clear the common duct. As a result of stone impaction in the pre-papillary portion of the bile duct, this process usually requires multiple mechanical lithotripsies and stone retrieval with baskets until extraction balloons can be used. EBLBD has been avoided and contraindicated in these cases[4]. Based on the original report by Ersoz et al[3] and two additional series[5,6], we hypothesized that EBLBD could be extended to patients with a nondilated distal bile duct. In our technique, we perform additional dilations in the proximal part of the duct and found that the full balloon length could frequently be inserted into the bile duct. As a result, we named this technique “endoscopic biliary large balloon dilation” and not papillary dilation as usually described. The goal of EBLBD is to create a wide opening in the distal biliary tree and papillary orifice to facilitate stone removal using extraction balloons or baskets. Importantly, this patient population is more difficult to manage even with the help of EBLBD in those with a nondilated distal duct. In the current study, patients with a nondilated distal duct were more likely to require mechanical lithotripsy (25% vs 6.4% for those with a nondilated and dilated distal duct, respectively) despite having significantly smaller stones and a lower number of stones than those with a dilated distal duct. This may be because even dilating the distal duct to 8 ATM (according to the manufacturer’s instructions, this pressure should theoretically dilate the duct to 15 mm), the promised duct width of more than 1 cm is not actually reached, as we observed in our practice. An explanation for this phenomenon is that the distal portion of the bile duct is located within the pancreas.
The use of sphincterotomy plus EBLBD significantly reduces the use of mechanical lithotripsy and procedural time in comparison to sphincterotomy alone, as demonstrated by a French multicenter study only evaluating patients with wide distal ducts, since these authors excluded patients with “stenotic” distal ducts[13]. In 150 difficult stone cases, the use of sphincterotomy plus EBLBD had the same complication rate as sphincterotomy alone and presented a higher clearance rate at the initial ERCP[13]. A meta-analysis of six other studies reached similar conclusions[14]. Of note, patients with nondilated distal ducts are more difficult to manage and were not included in these studies[13,14]. The use of EBLBD in patients with nondilated distal bile ducts would reduce the use of lithotripsy, shorten procedure time, and—in a cost containment reality such as ours—would significantly reduce costs by avoiding the employment of cholangioscopy-guided lithotripsy. In a general population of difficult stone patients, EBLBD is demonstrated to be as safe and as effective as single operator cholangioscopy-guided lithotripsy[15].
There are limitations to the current study. Data were extracted from two prospective randomized controlled trials evaluating PEP prevention and not difficult stone management. Data were retrospectively collected by reviewing the cholangiographies of the 191 patients who underwent EBLBD. The indications for EBLBD may not have been standardized in the sample, despite its single-center nature, since treatment for difficult choledocholithiasis was not the aim of the study. On the other hand, this study analyzed a significant sample of large biliary balloon dilated patients with nondilated distal ducts and we ensured that they were prospectively evaluated for complications given their involvement in two prospective trials.
EBLBD for stone removal may be feasible and effective option for patients with a nondilated or tapered distal bile duct and may be a significantly less costly and time-saving alternative to cholangioscopy-guided intracorporeal lithotripsy. Our technique, in which proximal parts of the duct and not just the pre-papillary region are dilated, may explain the success of EBLBD. This method requires prospective validation by future studies.
Endoscopic papillary large balloon dilation is increasingly being used in treating difficult bile duct stones, since it is faster and less laborious than performing multiple mechanical lithotripsies, with comparable results in terms of safety and effectiveness. However, this method is not recommended in patients with nondilated distal bile ducts, due to a theoretically higher complication rate, especially perforation.
Papillary large balloon dilation is an important tool to extract difficult duct stones and very few studies examined this technique in patients with nondilated distal ducts, although in its original report, this method was used in this setting.
To analyze the feasibility of papillary large balloon dilation in patients with difficult bile duct stones and nondilated distal bile ducts, as well as the complication rate and effectiveness of this method in this subset of stone patients. To investigate the demographic characteristics of this patient group. Data on these issues may stimulate future research and assist endoscopists in choosing the best endoscopic modality to treat difficult bile duct stones.
We retrieved data from 1289endoscopic retrograde cholangiopancreatography (ERCP) procedures from 2 prospective randomized controlled trials dealing with post-ERCP pancreatitis (PEP). Of these, 258 cases had difficult stones (> 1 cm, multiple > 8, impacted, or having a thin distal duct) and 191 underwent papillary large balloon dilation up to 15 mm after endoscopic sphincterotomy for stone retrieval. Cholangiographies of these cases were retrospectively reviewed by the authors in order to classify the distal bile duct as dilated or nondilated, as well as stone size and number. Primary outcomes were clearance rate at first ERCP and complications.
Of the 191 patients, 113 (59%) had a nondilated or tapered distal duct (75 F/38 M, mean age: 52 years) and 78 (47 F/31 M mean age: 68 years) a dilated distal duct. Cases with a nondilated distal duct had fewer (mean = 2 vs 4.1, P < 0.05) and smaller (mean 1.1 cm vs 1.7 cm, P < 0.05) stones than those with a dilated distal duct and were significantly younger than patients with dilated distal). Patients with a nondilated distal duct were also significantly younger and more likely to receive mechanical lithotripsy (25% vs 6.4%, P < 0.05). Clearance rate at first ERCP was comparable between patients with a dilated (73/78; 94%) and nondilated distal ducts (103/113; 91%). Procedures were faster in patients with a dilated distal duct (mean 17 vs 24 min, P < 0.005). Complications were similar in both groups: 8/113 (7.1%) vs 5/78 (6.4%), however the 2 perforations occurred in patients with nondilated ducts. There was no mortality.
Large balloon dilation for difficult stones is feasible in patients with a nondilated or even tapered distal duct. Although the latter patients had smaller stones, they are more difficult to remove, since ERCP procedures in these patients require mechanical lithotripsy more often and last longer.
Future prospective multicenter studies should evaluate the feasibility of large balloon dilation in patients with nondilated distal bile ducts and difficult stones, since current guidelines do not recommend the procedure in this group of patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Dong SH, South Korea; Goenka MK, India S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Pereira Lima JC, Arciniegas Sanmartin ID, Latrônico Palma B, Oliveira Dos Santos CE. Risk Factors for Success, Complications, and Death after Endoscopic Sphincterotomy for Bile Duct Stones: A 17-Year Experience with 2,137 Cases. Dig Dis. 2020;38:534-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 2. | Bokemeyer A, Gerges C, Lang D, Bettenworth D, Kabar I, Schmidt H, Neuhaus H, Ullerich H, Lenze F, Beyna T. Digital single-operator video cholangioscopy in treating refractory biliary stones: a multicenter observational study. Surg Endosc. 2020;34:1914-1922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 256] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 4. | Kim TH, Kim JH, Seo DW, Lee DK, Reddy ND, Rerknimitr R, Ratanachu-Ek T, Khor CJ, Itoi T, Yasuda I, Isayama H, Lau JY, Wang HP, Chan HH, Hu B, Kozarek RA, Baron TH. International consensus guidelines for endoscopic papillary large-balloon dilation. Gastrointest Endosc. 2016;83:37-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 62] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 5. | Fujita Y, Iwasaki A, Sato T, Fujisawa T, Sekino Y, Hosono K, Matsuhashi N, Sakamaki K, Nakajima A, Kubota K. Feasibility of Endoscopic Papillary Large Balloon Dilation in Patients with Difficult Bile Duct Stones without Dilatation of the Lower Part of the Extrahepatic Bile Duct. Gut Liver. 2017;11:149-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (1)] |
| 7. | de Quadros Onófrio F, Lima JCP, Watte G, Lehmen RL, Oba D, Camargo G, Dos Santos CEO. Prophylaxis of pancreatitis with intravenous ketoprofen in a consecutive population of ERCP patients: a randomized double-blind placebo-controlled trial. Surg Endosc. 2017;31:2317-2324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Pereira-Lima J, Arciniegas Sanmartin ID, Watte G, Contin I, Pereira-Lima G, Quadros Onófrio F, Altmayer S, Oliveira Dos Santos CE. Biliary cannulation with contrast and guide-wire vs exclusive guide-wire: A prospective, randomized, double-blind trial. Pancreatology. 2021;21:459-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro M, Hritz I, Mariani A, Paspatis G, Radaelli F, Lakhtakia S, Veitch AM, van Hooft JE. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52:127-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 495] [Article Influence: 99.0] [Reference Citation Analysis (1)] |
| 10. | Hisatomi K, Ohno A, Tabei K, Kubota K, Matsuhashi N. Effects of large-balloon dilation on the major duodenal papilla and the lower bile duct: histological evaluation by using an ex vivo adult porcine model. Gastrointest Endosc. 2010;72:366-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Lee GH, Yang MJ, Kim JH, Hwang JC, Yoo BM, Lee DK, Jang SI, Lee TH, Park SH, Park JS, Jeong S, Lee DH. Balloons larger than 15 mm can increase the risk of adverse events following endoscopic papillary large balloon dilation. J Gastroenterol Hepatol. 2019;34:1450-1453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Park SJ, Kim JH, Hwang JC, Kim HG, Lee DH, Jeong S, Cha SW, Cho YD, Kim HJ, Moon JH, Park SH, Itoi T, Isayama H, Kogure H, Lee SJ, Jung KT, Lee HS, Baron TH, Lee DK. Factors predictive of adverse events following endoscopic papillary large balloon dilation: results from a multicenter series. Dig Dis Sci. 2013;58:1100-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 13. | Karsenti D, Coron E, Vanbiervliet G, Privat J, Kull E, Bichard P, Perrot B, Quentin V, Duriez A, Cholet F, Subtil C, Duchmann JC, Lefort C, Hudziak H, Koch S, Granval P, Lecleire S, Charachon A, Barange K, Cesbron EM, De Widerspach A, Le Baleur Y, Barthet M, Poincloux L. Complete endoscopic sphincterotomy with vs. without large-balloon dilation for the removal of large bile duct stones: randomized multicenter study. Endoscopy. 2017;49:968-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Yang XM, Hu B. Endoscopic sphincterotomy plus large-balloon dilation vs endoscopic sphincterotomy for choledocholithiasis: a meta-analysis. World J Gastroenterol. 2013;19:9453-9460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Franzini T, Moura RN, Bonifácio P, Luz GO, de Souza TF, Dos Santos MEL, Rodela GL, Ide E, Herman P, Montagnini AL, D'Albuquerque LAC, Sakai P, de Moura EGH. Complex biliary stones management: cholangioscopy vs papillary large balloon dilation - a randomized controlled trial. Endosc Int Open. 2018;6:E131-E138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |