Published online Mar 16, 2022. doi: 10.4253/wjge.v14.i3.176
Peer-review started: July 31, 2021
First decision: September 29, 2021
Revised: October 5, 2021
Accepted: February 10, 2022
Article in press: February 10, 2022
Published online: March 16, 2022
Processing time: 227 Days and 18 Hours
The lymphoma of the mucosa-associated lymphoid tissue (MALT) is predominantly found in the stomach. The few cases reported in the literature of MALT lymphomas affecting the ileum are in patients who are already symptomatic and with clear advanced endoscopic findings. We present the first case of an asymptomatic female patient who underwent colonoscopy as a routine examination with the findings of an ulcer in the distal ileum region, which histopathological examination and associated immunohistochemistry revealed the diagnosis of MALT lymphoma.
A 57-year-old asymptomatic female patient underwent a colonoscopy exam for screening. The examination revealed an ulcer of medium depth with well-defined borders covered by a thin layer of fibrin and a halo of hyperemia in the distal ileum portion. Findings are nonspecific but may signal infections by viruses, protozoa, and parasites or inflammatory diseases such as Crohn's disease. Biopsies of the ulcer were taken. The anatomopathological result revealed an atypical diffuse lymphocytic infiltrate of small cells with a characteristic cytoplasmic halo of marginal zone cells. The immunohistochemical study was performed and the results demonstrated a negative neoplastic infiltrate for the expression of cyclin D1 and cytokeratin AE1/AE3 and a positive for BCL60 in the germinal center. The test also revealed CD10 positivity in the glandular epithelium and germinal center of a reactive follicle with dual-labeling of CD20 and CD3 demonstrating the B lymphocyte nature of the neoplastic infiltrate. In BCL2 protein labeling, the neoplastic infiltrate is strongly positive with a negative germinal center. The findings are consistent with immunophenotype B non-Hodgkin's lymphoma, better classified as extranodal MALT. The patient was treated with chemotherapy and showed complete regression of the disease, as evidenced by colonoscopy performed after treatment.
MALT lymphomas in the terminal ileum are extremely rare and only 4 cases have been reported in the literature. Given the low sensitivity and specificity of endoscopic images in these cases, the pathology can be confused with other important differential diagnoses such as inflammatory diseases or infectious diseases and which makes the biopsy important, even in asymptomatic patients, paired with anatomopathological analysis and immunohistochemistry which is the gold standard for correct diagnosis.
Core Tip: Mucosa-associated lymphoid tissue (MALT) lymphoma is predominantly found in the stomach. Only a few cases of MALT lymphomas affecting the ileum have been published in the literature and these patients already had clear symptoms and endoscopic findings. We present a rare case of MALT lymphoma in the terminal ileum in an asymptomatic patient who underwent the examination for age screening.
- Citation: de Figueiredo VLP, Ribeiro IB, de Moura DTH, Oliveira CC, de Moura EGH. Mucosa-associated lymphoid tissue lymphoma in the terminal ileum: A case report. World J Gastrointest Endosc 2022; 14(3): 176-182
- URL: https://www.wjgnet.com/1948-5190/full/v14/i3/176.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i3.176
Mucosa-associated lymphoid tissue (MALT) lymphoma is a low-grade B-cell neoplasm of the extranodal marginal zone characterized by a lymphoid infiltrate in the mucous layer of hollow organs and glandular tissues[1,2]. The gastrointestinal tract is involved in about 50% of the cases[2,3] with the stomach accounting for 85% of all cases and strongly related to the presence and infection by Helicobacter pylori (H. pylori)[1,4]. Other, less usual regions can also be affected, such as salivary glands, lungs (14%), head and neck (15%), ocular attachments (12%) and skin (11%)[5].
MALT lymphomas in the ileum are extremely rare and few cases have been reported in the literature[5-9]. In these, all patients had already presented with an advanced degree of involvement with notable symptoms and with lesions dispersed throughout the ileocecal region[5,6].
This is the first reported case of a terminal ileum MALT lymphoma in an asymptomatic patient reported in the literature.
Asymptomatic.
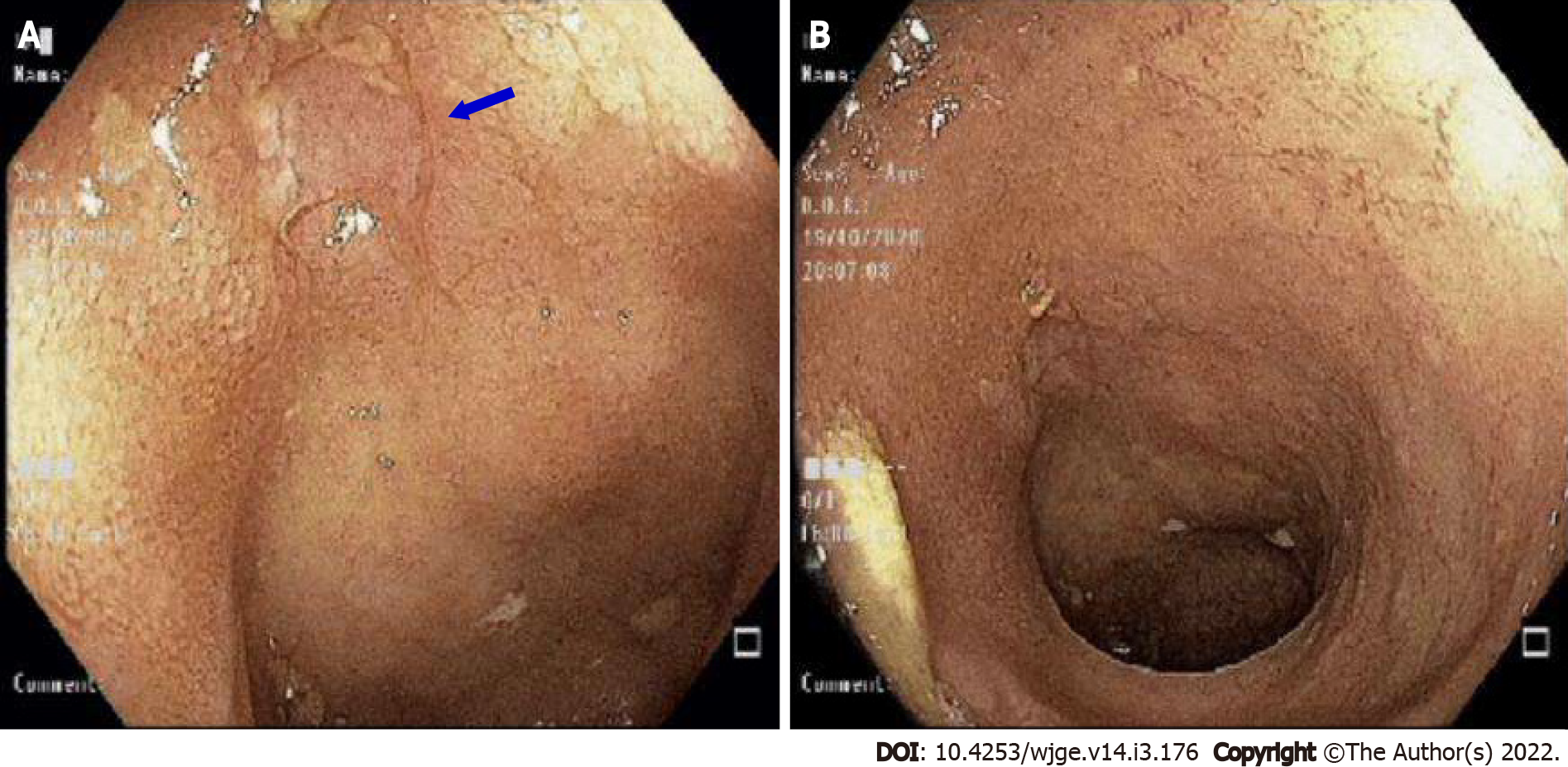
A 57-year-old asymptomatic female patient underwent a colonoscopy exam for screening. The examination revealed an ulcer of medium depth with well-defined borders covered by a thin layer of fibrin and a halo of hyperemia in the distal ileum portion (Figure 1). Findings are nonspecific but may signal infections by viruses, protozoa and parasites or inflammatory diseases such as Crohn's disease. Biopsies of the ulcer were taken.
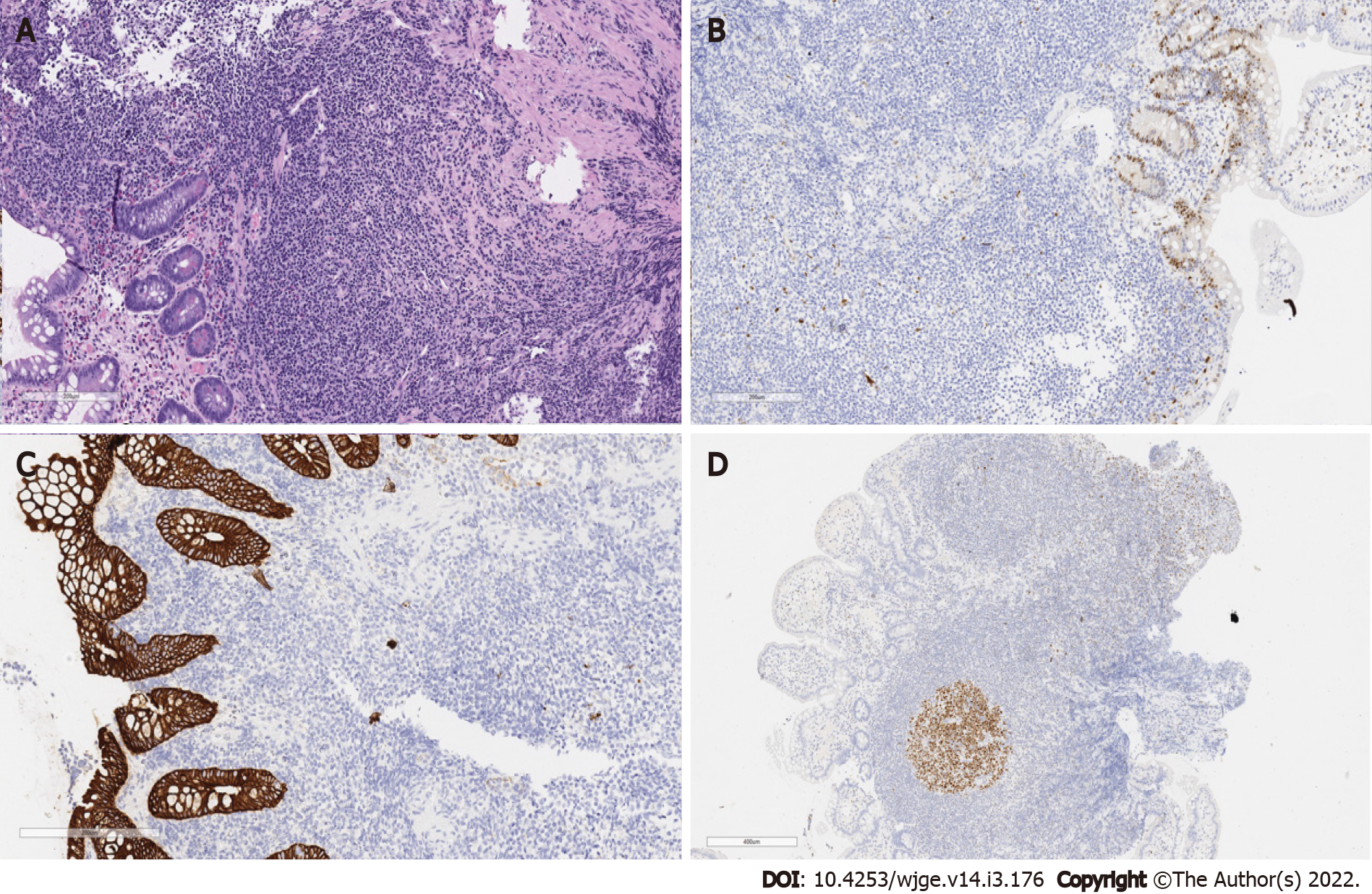
The anatomopathological result revealed an atypical diffuse lymphocytic infiltrate of small cells with a characteristic cytoplasmic halo of marginal zone cells. The infiltrate presented with nodular and poorly delimited areas with dissection of collagen fibers and the muscular layer of the mucosa. There was no clear distinction regarding germinal centers. Signs of cellular atypia were also observed with enlarged nuclei. In the most superficial portion there was focal erosion, epithelial reactivity and eosinophilia (above 15 per high-power field) (Figure 2). No granulomas were found and there were no signs of infection by parasitic agents. An immunohistochemical study was requested to investigate lymphoproliferative disease.
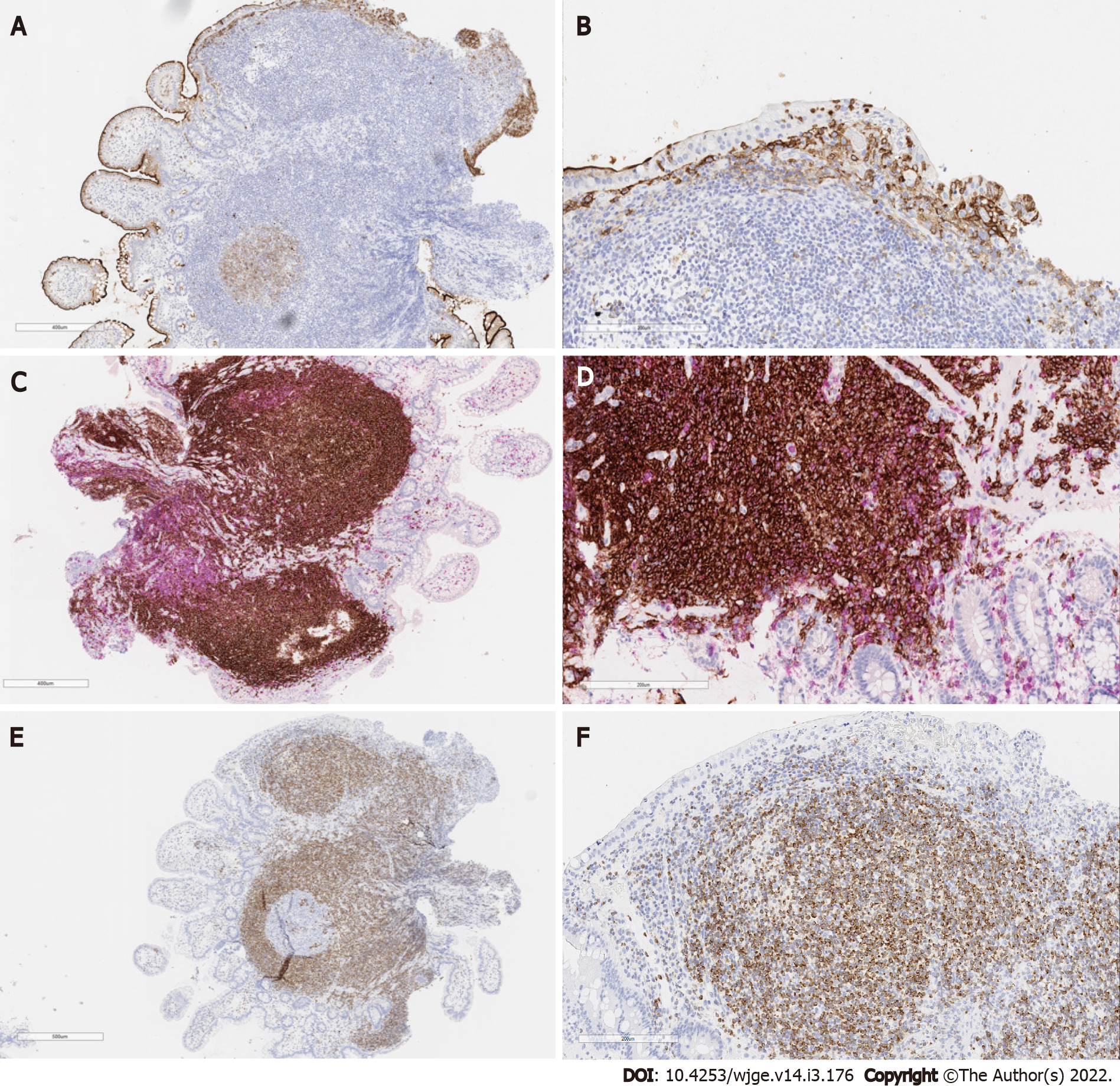
The immunohistochemical study was performed by the EnVision FLEX Visualization System kit AGILENT (DAKO) method, which the results demonstrated a negative neoplastic infiltrate for the expression of cyclin D1 (Figure 2B) and cytokeratin AE1/AE3 (Figure 2C) and positive for BCL60 in the germinal center (Figure 2D). The test also revealed CD10 positivity in the glandular epithelium and germinal center of a reactive follicle (Figure 3A and B) with dual labeling of CD20 and CD3 demonstrating the B lymphocyte nature of the neoplastic infiltrate (Figure 3C and D). In BCL2 protein labeling, the neoplastic infiltrate is strongly positive with a negative germinal center (Figure 3E and F).
The findings are consistent with immunophenotype B non-Hodgkin's lymphoma, better classified as extranodal MALT. The identification of lymphoid proliferation with atypical limits in a nodular and infiltrative pattern with foci of epithelial aggression was crucial for the diagnosis. Since MALT lymphomas are always negative for BCL6 and CD10 and positive for BCL2 with a negative germinal center, it was possible to rule out the differential diagnosis of follicular lymphoma.
The patient was referred to the oncology team and treated with chemotherapy.
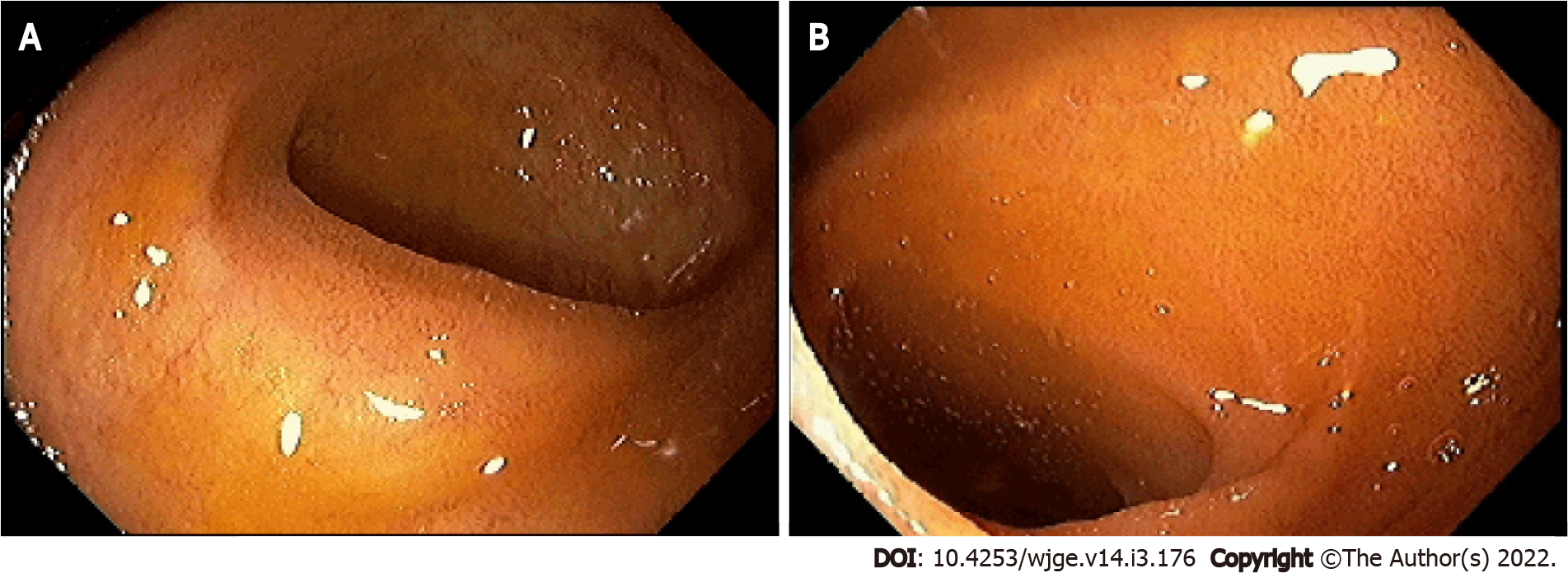
Upon completion of treatment, the patient showed complete regression of the disease as evidenced by colonoscopy performed after treatment (Figure 4).
Extranodal marginal zone lymphoma (MALT lymphoma) is characterized by the proliferation of small B lymphocytes[10]. The stomach is the most common site of involvement where the main etiology is H. pylori infection[1]. In these cases, the endoscopic findings are varied and involve polyps, ulcerations, erythematous lesions, nodules and other non-specific findings[11]. Extranodal marginal zone lymphomas that affect the ileum region are extremely rare and only a few cases have been reported in the literature[5-9]. None of the previous studies showed H. pylori infections so the etiology of the disease remains unknown.
Endoscopic findings of primary small bowel lymphoma can be classified into 5 patterns: Mucosal fold thickening; nodular pattern, defined by the presence of nodules and micronodules of variable sizes; infiltrative pattern, where the bowel wall is immobile, not distended by insufflation, and firm over forceps; ulcerative pattern with ulcers of variable sizes and depths, and mosaic pattern[12].
Among the four cases published in the literature on ileum MALT lymphomas, all presented endoscopic findings with multiple protuberances: Two[5,7] cases with ulcerations and two[6,8] cases with smooth mucosa. In one case, the presence of a single mass in the intestine was demonstrated without erosions in the mucosa[6].
The treatment of MALT lymphoma is initially made with the eradication of H. pylori, in cases with involvement of the bacteria. If there is no concomitant H. pylori infection or no tumor remission after H. pylori treatment, radiotherapy, chemotherapy, or immunotherapy with anti-CD20 monoclonal antibodies should be considered. Radiotherapy has an excellent prognosis when used in cases where the disease is localized. In the presence of disseminated or more advanced disease, the use of radiotherapy or immunotherapy is indicated. Treatment must be individualized according to the stage of the disease and symptoms, as well as the patient's preference[13]. Although MALT lymphoma has a favorable prognosis and is responsive to systematic therapy, especially when identified early, when patients are symptomatic, unfortunately they already have a more advanced degree of involvement.
Terada[5] reported the case of a 34-year-old patient with abdominal pain and melena whose colonoscopy revealed multiple nodules and ulcers scattered throughout the ileum. Endoscopic images were suggestive of ileitis, mesenchymal tumor, or lymphoma.
Hasegawa et al[6] described two cases of oligosymptomatic patients with abdominal pain being a common symptom. Colonoscopy in the first case found multiple whitish nodules in the region close to the ileocecal valve, which had a smooth and polished appearance. In the second case, a colonoscopy revealed an ileocecal valve with an enlarged, soft appearance and areas of enanthema.
Makino et al[7] discussed a case of a patient with initial complaints of postprandial epigastric pain. Colonoscopy examination revealed multiple protruding lesions in the terminal ileum with an erosive surface covered by swollen mucosa.
In the report by Ohashi et al[8] colonoscopy identified multiple polyposis lesions in the terminal ileum with an absence of villi.
In all cases, biopsy with histological evaluation concurrently with immunohistochemical analysis was crucial for the diagnosis of MALT lymphoma.
The uniqueness of the case presented in this study is due to the fact that the patient was asymptomatic and her endoscopic findings had a more discrete and nonspecific pattern compared to other studies which made the diagnosis even more challenging.
Given the low sensitivity and specificity of endoscopic images in these cases the pathology can be confused with other important differential diagnoses such as inflammatory diseases (such as Crohn's disease) or infectious diseases, which makes the biopsy, even in asymptomatic patients, with anatomopathological analysis and performing immunohistochemistry, the gold standard for correct diagnosis[14].
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Batyrbekov K, Jin ZD, Chi T S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Violeta Filip P, Cuciureanu D, Sorina Diaconu L, Maria Vladareanu A, Silvia Pop C. MALT lymphoma: epidemiology, clinical diagnosis and treatment. J Med Life. 2018;11:187-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 77] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 2. | Vetro C, Romano A, Amico I, Conticello C, Motta G, Figuera A, Chiarenza A, Di Raimondo C, Giulietti G, Bonanno G, Palumbo GA, Di Raimondo F. Endoscopic features of gastro-intestinal lymphomas: from diagnosis to follow-up. World J Gastroenterol. 2014;20:12993-13005. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 37] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Oh SY, Kim WS, Kim JS, Kim SJ, Lee S, Lee DH, Won JH, Hwang IG, Kim MK, Lee SI, Chae YS, Yang DH, Kang HJ, Choi CW, Park J, Kim HJ, Kwon JH, Lee HS, Lee GW, Eom HS, Kwak JY, Lee WS, Suh C. Multiple mucosa-associated lymphoid tissue organs involving marginal zone B cell lymphoma: organ-specific relationships and the prognostic factors. Consortium for improving survival of lymphoma study. Int J Hematol. 2010;92:510-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | De Miranda Neto AA, Marques SB, Baba ER, Yamazaki K, Ribeiro IB, De Moura EGH. Extensive squamous metaplasia of the stomach. Arq Gastroenterol. 2020;57:335-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Terada T. Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) of the ileum in a 35-year-old Japanese woman. Int J Clin Exp Pathol. 2013;6:951-956. [PubMed] |
| 6. | Hasegawa N, Tsuboi Y, Kato K, Yamada K, Morita K, Kuroiwa M, Ito H, Matsushima T, Ono K, Oshiro M. Endoscopic diagnosis of ileocecal mucosa-associated lymphoid tissue lymphoma. Gastrointest Endosc. 1999;50:115-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Makino Y, Suzuki H, Nishizawa T, Kameyama K, Hisamatsu T, Imaeda H, Mukai M, Hibi T. Ileal Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma with a Large-Cell Component That Regressed Spontaneously. Gut Liver. 2010;4:117-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Ohashi S, Yazumi S, Watanabe N, Matsumoto S, Fukui T, Nishio A, Chiba T. Education and imaging. Gastrointestinal: MALT lymphoma of the terminal ileum. J Gastroenterol Hepatol. 2006;21:1495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Matsumoto Y, Matsumoto T, Nakamura S, Kawasaki A, Aso M, Aoyagi K, Sadoshima S, Onoyama K, Fujishima M. Primary ileal plasmacytoma arising in mixed low- and high-grade B-cell lymphoma of mucosa-associated lymphoid tissue type. Abdom Imaging. 2000;25:139-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Palo S, Biligi DS. A Unique Presentation of Primary Intestinal MALT Lymphoma as Multiple Lymphomatous Polyposis. J Clin Diagn Res. 2016;10:ED16-ED18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Ahmad A, Govil Y, Frank BB. Gastric mucosa-associated lymphoid tissue lymphoma. Am J Gastroenterol. 2003;98:975-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 85] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Halphen M, Najjar T, Jaafoura H, Cammoun M, Tufrali G. Diagnostic value of upper intestinal fiber endoscopy in primary small intestinal lymphoma. A prospective study by the Tunisian-French Intestinal Lymphoma Group. Cancer. 1986;58:2140-2145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Gong EJ, Choi KD. [Diagnosis and Treatment of Gastric Mucosa-associated Lymphoid Tissue Lymphoma]. Korean J Gastroenterol. 2019;74:304-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Park BS, Lee SH. Endoscopic features aiding the diagnosis of gastric mucosa-associated lymphoid tissue lymphoma. Yeungnam Univ J Med. 2019;36:85-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |