Published online Mar 16, 2022. doi: 10.4253/wjge.v14.i3.142
Peer-review started: April 21, 2021
First decision: June 25, 2021
Revised: July 17, 2021
Accepted: February 11, 2022
Article in press: February 11, 2022
Published online: March 16, 2022
Processing time: 328 Days and 19.5 Hours
Musculoskeletal injuries (MSI) have plagued endoscopists and ancillary staff for decades without any innovative and strong ergonomic guidelines. It has placed a physical and mental strain on our endoscopists and ancillary staff. We have very have limited data supporting this claim in our region and most data is supported by western literature.
To document the prevalence of MSI, and awareness and practices of ergonomics by endoscopists and ancillary staff.
This is an observational cross-sectional study, conducted in Karachi, a city that boasts the maximum number of daily endoscopies in the country. An eleven-point self-administered questionnaire was distributed and used to evaluate MSI and ergonomic adjustments amongst three tertiary care setups in Karachi. An onsite survey via a 13-point checklist for endoscopy suite facilities was used to assess the ergonomically friendly conveniences at five tertiary care setups in Karachi. A total of 56 participants replied with a filled survey.
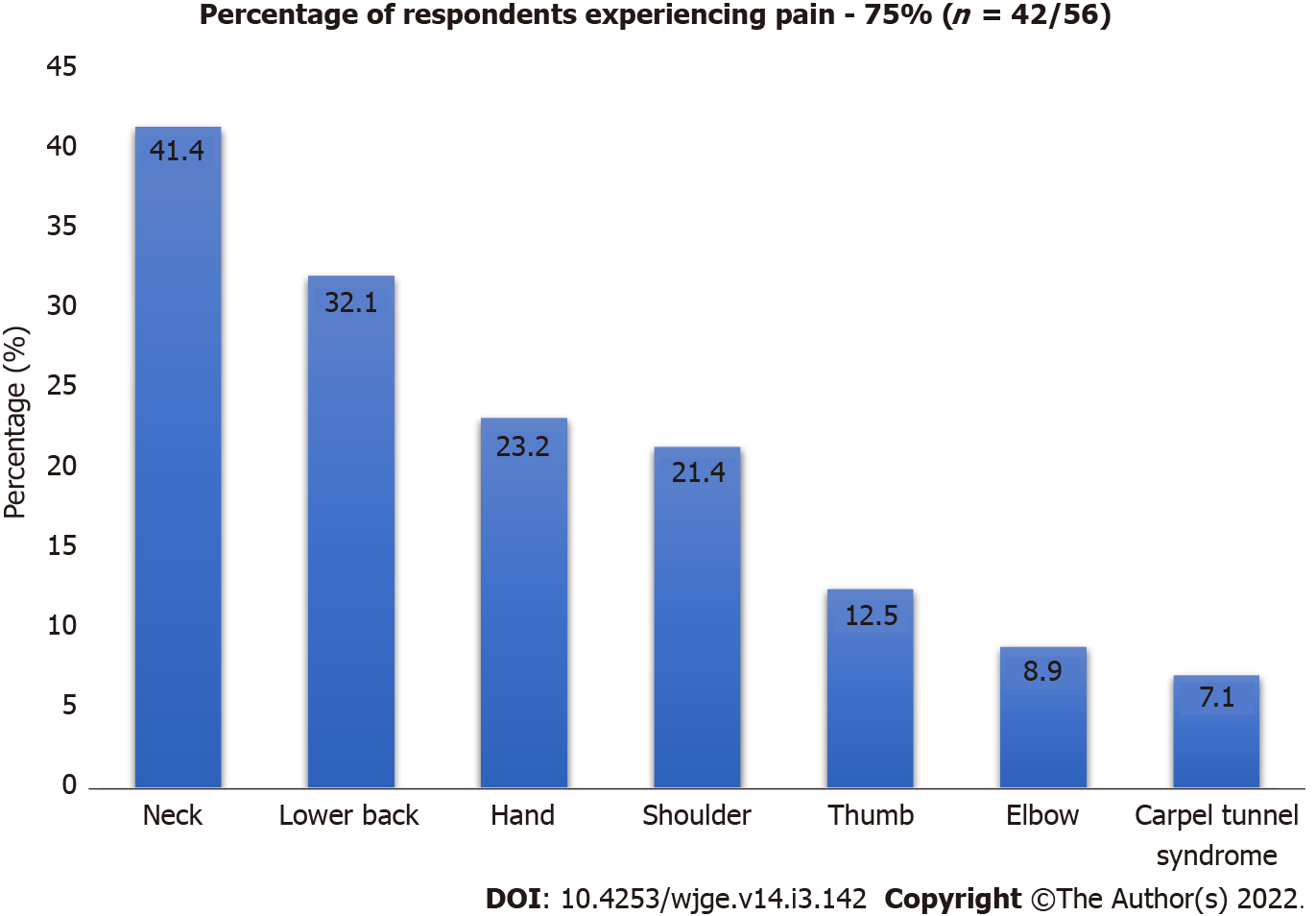
There were 56 participants in total with 39 (69.6%) males. Pain and numbness were documented by 75% of the patients, with pain in the neck (41.1%), lower back (32.1%), shoulder (21.4%), thumb (12.5%), hand (23.2%), elbow (8.9%), and carpal tunnel syndrome (CTS) (7.1%). Of those, 33.3% attributed their symptoms to endoscopy, 14.2% said that symptoms were not caused by endoscopy, and 52.4% were not certain whether endoscopy had caused their symptoms. Twenty-one point four percent of patients had to take time off their work, while 33.9% took medications for pain. Ergonomic modifications to prevent musculoskeletal injury, including placement of endoscopic monitor at eye level and the cardiac monitor in front, stopping the procedure to move patients, sitting while performing colonoscopy, and navigating height-adjustable bed were used by 21.4%. Nine out of 13 ergonomic facilities were not present in all five tertiary care hospitals. Conveniences, such as anti-fatigue mats, height-adjustable computer stations, and time out between patients were not present.
Three-fourth of our endoscopists reported MSI, of which more than half were not sure or attributed this problem to endoscopy. The prevalence of MSI warrants urgent attention.
Core Tip: Musculoskeletal injuries (MSI) have impacted gastroenterologists and ancillary staff involved in endoscopy. Maneuvers, time duration, and failure of ergonomic practices and provision of facilities have led to the prevalence of MSI. This has resulted in stress, chronic pain management, office leaves, and consumption of analgesics. We found three-fourth of our endoscopists reported MSI, of which more than half were not sure or attributed this problem to endoscopy. The high prevalence of MSI and lack of awareness among endoscopists and ancillary staff needs to be addressed urgently.
- Citation: Shah SZ, Rehman ST, Khan A, Hussain MM, Ali M, Sarwar S, Abid S. Ergonomics of gastrointestinal endoscopies: Musculoskeletal injury among endoscopy physicians, nurses, and technicians. World J Gastrointest Endosc 2022; 14(3): 142-152
- URL: https://www.wjgnet.com/1948-5190/full/v14/i3/142.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i3.142
Several studies have suggested a high prevalence of musculoskeletal injuries (MSI) among endoscopists and ancillary staff. Survey-based studies estimate a 29% to 89% prevalence of musculoskeletal pain among gastroenterologists[1], which directly translates to a loss of productivity. Rigorous training and increased demand for endoscopies make a gastroenterologist an asset in the workplace, especially in the developing world. A work-related injury can greatly affect the quality and longevity of the gastroenterologist, which can ultimately exacerbate the shortage of specialists[2]. Improving ergonomic conditions will ensure maximum utilization of this scarce human resource. MSI are widespread and are strongly correlated with high procedure volume and procedure duration[3]. Endoscopists are at risk for overuse syndromes and overuse injuries, such as carpal tunnel syndrome (CTS), De Quervain's tenosynovitis, and lateral epicondylitis because of the repetitive movements, pinching and gripping of the endoscope, pushing, pulling, torquing of the insertion tube and potentially awkward posture associated with endoscopic procedures[1,3]. However, institutional changes minimizing MSI are limited, which can be an important contributory factor of lack of awareness[1].
Limited documented data, especially in the eastern population, and lack of awareness are contributory factors to the lack of widespread change. Additionally, a robust analysis to identify risk factors associated with endoscopy-related injury is lacking. Creating awareness about the importance of ergonomics in endoscopy may prevent future injury. There is no standardized curriculum for learning endoscopic techniques, and most endoscopists learn their skills during their fellowship training through their faculty mentor, which creates great variability in the level of skill among trainees. This variability and lack of emphasis on ergonomics during teaching propagate the risk of MSI. Strategies for the management of the risk of MSI related to the practice of endoscopy include compliance with currently recommended ergonomic practices, standardized education of trainees in ergonomic technique when practicing endoscopy, research toward the modification and development of more ergonomic endoscopes and procedure spaces, and institutional emphasis[4]. This study aims to document the prevalence of MSI, awareness and practice of ergonomics by endoscopists and ancillary staff.
Questionnaires were tendered to endoscopists and ancillary staff. The questionnaire was designed and informed consent was implied by a completed response to the survey. The survey was handed out following June 2019 onwards with a collection on follow-up from respondents. Ethical approval was obtained from Ethics Review Committee Aga Khan University (5357-Med-ERC-18).
Participants were endoscopists and ancillary staff found in the endoscopy suites in three tertiary care hospitals namely, Aga Khan University Hospital, Liaquat National Hospital, and Dr. Ruth K. M. Pfau Civil Hospital, all located in Karachi, Pakistan. All endoscopy physicians, nurses, and technicians approached. There was no monetary compensation for participation.
An eleven-point, self-administered, paper-based survey was devised by an endoscopist and a member of the ancillary staff (Supplementary Material 1). Items in the questionnaire were generated based on literature review[2,3,5] and multidisciplinary discussions on the topic. These questions focused on demographics, average physical activity, location of the injury. It also questioned the subject’s perception of work/endoscopy-related MSI, and further intrigued on their remedies, the need for skipping work, and the use of ergonomic techniques to facilitate themselves.
Initially, the survey was pilot-tested by handing it over to endoscopists and ancillary staff members from the Department of Gastroenterology at Aga Khan University Hospital. The purpose was to evaluate its language, content clarity, and to deduce an approximate time to complete, although trained researchers were present during data collection to clarify any ambiguities. The final survey evaluated the respondent’s general demographic, characteristics, workload, type, treatment, and impact of severity of MSI on a daily professional capacity. The survey took approximately 6 min to be filled out.
A 13-point checklist (Supplementary Material 2) was adapted and devised from a literature search[6-9]. The endoscopic suites at five tertiary care hospitals, namely, Aga Khan University Hospital, Ziauddin University Hospital, Liaquat National Hospital, Dr. Ruth K. M. Pfau Civil Hospital, Sindh Institute of Urology and Transplant, all placed within Karachi, Pakistan were evaluated. The checklist was used to assess measures employed by these 5 major tertiary care hospitals in this metropolis to reduce MSI.
Ergonomic conditions were evaluated by the investigators. These 13 points briefly assessed the suite for endoscopic monitor, monitor height adjustability, booms, and stands. It also assessed time out between two consecutive patients, support stands, anti-fatigue mats, tiltable examination beds, cardiac monitor adjustability, and having the endoscopic retrograde cholangiopancreatography (ERCP) room in the same suite (Supplementary Material 2).
This observational cross-sectional study had its statistical review performed by a biomedical statistician present at the Department of Medicine at Aga Khan University. Analysis was performed using SPSS (Statistical Package of Social Sciences) version 19. Continuous variables were reported as mean ± SD. Prevalence (%) of demographic and clinical factors were assessed. All participants were divided into four groups: endoscopists, trainees, nurses, and technicians, and had their frequency of MSI compared in different groups by chi-square test. This data was stratified by gender and evaluated. All P values were based on two-sided tests and significance was set at a P value less than 0.05.
Data from 56 participants were collected, of which 39 (69.6%) were male (Table 1). Eighty-seven point five percent had right-hand dominance. There were 23.2% endoscopists, 16.1% gastroenterology residents, 26.8% endoscopy nurses, and 33.9% endoscopy technicians.
| Demographics | n = 56 (%) |
| Mean age, yr | 35.09 (18-62) |
| Male | 39 (69.6) |
| Female | 17 (30.3) |
| Endoscopist | 13 (23.2) |
| GI resident | 9 (16.1) |
| Endoscopy nurse | 15 (26.8) |
| Endoscopy technician | 19 (33.9) |
| Mean number of endoscopies performed per week | 63.85 |
The level of physical activity was appraised. No regular exercise was seen in 41.1%, 23.2% exercised less than 150 min/wk, 8.9% exercised 150 min/wk, and 26.8% exercised more than 150 min/wk.
Participants who had been doing endoscopies for up to 5 years accounted for 48.9%, while 51% had been involved in endoscopy for more than 5 years.
Pain and numbness were reported by 75% of total respondents with anatomical regions specified as neck (41.1%) lower back pain (32.1%) shoulder pain (21.4%), thumb pain (12.5%) hand pain (23.2%), elbow pain (8.9%) and CTS (7.1%), being the most affected with pain (Figure 1).
On an individual basis, out of endoscopists, residents, nurses, and technicians, we found endoscopists reporting the least to experience pain (53.8%) (Table 2). This was followed by residents at 77.8%, technicians at 78.9%, and finally with nurses reporting the most pain at 86.7%. Overall, there is not much distribution amongst the subgroups of the endoscopy team; however, we saw four cases of CTS. All four belonged to endoscopy nurses or endoscopy technicians.
| Endoscopist | GI resident | Endoscopy nurse | E. technician | P value | |
| Pain or numbness (%) | 0.22 | ||||
| Yes | 7 (53.8) | 7 (77.8) | 13 (86.7) | 15 (78.9) | |
| No | 6 (46.2) | 2 (22.2) | 2 (13.3) | 4 (21.1) | |
| Left thumb pain (%) | 0.02 | ||||
| Yes | 2 (15.4) | 0 | 2 (13.3) | 0 | |
| No | 11 (84.6) | 9 (100) | 13 (86.7) | 19 (100) | |
| Right thumb pain (%) | |||||
| Yes | 0 | 3 (33.3) | 0 | 0 | |
| No | 13 (100) | 6 (66.7) | 15 (100) | 19 (100) | |
| Left shoulder pain (%) | 0.48 | ||||
| Yes | 0 | 0 | 1 (6.6) | 0 | |
| No | 13 (100) | 9 (100) | 14 (93.4) | 19 (100) | |
| Right shoulder pain (%) | |||||
| Yes | 0 | 1 (11.1) | 0 | 0 | |
| No | 13 (100) | 8 (88.9) | 15 (100) | 19 (100) | |
| Both shoulder pain (%) | |||||
| Yes | 2 (15.4) | 2 (22.2) | 3 (20) | 3 (15.7) | |
| No | 11 (84.6) | 7 (77.8) | 12 (80) | 16 (84.) | |
| Left hand pain (%) | 0.06 | ||||
| Yes | 0 | 0 | 2 (13.3) | 0 | |
| No | 13 (100) | 9 (100) | 13 (86.7) | 19 (100) | |
| Right hand pain (%) | |||||
| Yes | 0 | 2 (22.2) | 1 (6.6) | 1 (5.3) | |
| No | 13 (100) | 7 (77.8) | 14 (93.4) | 18 (94.7) | |
| Both hand pain (%) | |||||
| Yes | 0 | 0 | 2 (13.3) | 5 (26.3) | |
| No | 13 (100) | 9 (100) | 13 (86.7) | 14 (73.7) | |
| Neck/upper back (%) | 0.004 | ||||
| Yes | 3 (23.1) | 5 (55.5) | 6 (40) | 9 (47.3) | |
| No | 10 (76.9) | 4 (44.5) | 9 (60) | 10 (52.7) | |
| Lower back (%) | |||||
| Yes | 2 (15.4) | 1 (11.1) | 8 (53.3) | 7 (36.8) | |
| No | 11 (84.6) | 8 (88.9) | 7 (46.7) | 12 (63.2) | |
| Left elbow pain (%) | 0.57 | ||||
| Yes | 0 | 0 | 1 (6.6) | 0 | |
| No | 13 (100) | 9 (100) | 14 (93.4) | 19 (100) | |
| Right elbow pain (%) | |||||
| Yes | 1 (7.6) | 1 (11.8) | 1 (6.6) | 0 | |
| No | 12 (92.4) | 8 (88.2) | 14 (93.4) | 19 (100) | |
| Both elbow pain (%) | |||||
| Yes | 0 | 0 | 1 (6.6) | 0 | |
| No | 13 (100) | 9 (100) | 14 (93.4) | 19 (100) | |
| L hand numbness (%) | 0.59 | ||||
| Yes | 1 (7.6) | 0 | 1 (6.6) | 0 | |
| No | 12 (92.4) | 9 (100) | 14 (93.4) | 19 (100) | |
| R hand numbness (%) | |||||
| Yes | 0 | 1 (11.1) | 0 | 1 (5.2) | |
| No | 13 (100) | 8 (88.9) | 15 (100) | 18 (94.8) | |
| B/l hand numbness (%) | |||||
| Yes | 0 | 0 | 1 (6.6) | 0 | |
| No | 13 (100) | 9 (100) | 14 (93.4) | 19 (100) | |
| Carpal tunnel (%) | 0.00 | ||||
| Yes | 0 | 0 | 2 (13.3) | 2 (10.5) | |
| No | 13 (100) | 9 (100) | 13 (86.6) | 17 (89.5) |
We found a majority of the male and female technicians (66% and 100%) (Table 3) agreeing to neck pain which is the most common area affected overall while most nurses, both in males (100%) and females (53.8%) said to experience no pain in their neck. This does have real-time value as we found nurses using and performing hand and wrist-based actions and movements more frequently, and likewise, the nurses in our setup play a major role in holding the mouth guard. Table 3 can be seen showing a sub-analysis of gender-based data of male vs females in their respective professions of endoscopists, residents, nurses, and technicians.
| Male | P value | Female | P value | ||||||||
| Endoscopist (%) | GI resident (%) | Nurse (%) | Technicians (%) | Endoscopist (%) | GI resident (%) | Nurse (%) | Technicians (%) | ||||
| Pain | 0.536 | 0.148 | |||||||||
| Yes | 7 (58.3) | 5 (71.4) | 2 (100) | 14 (77.8) | 0 (0) | 2 (100) | 11 (84.6) | 1 (100) | |||
| No | 5 (41.7) | 2 (28.6) | 0 | 4 (22.2) | 1 (100) | 0 | 2 (15.4) | 0 | |||
| Thumb pain | 0.028 | 0.207 | |||||||||
| Left | 2 (16.7) | 0 | 0 | 0 | 0 | 0 | 2 (15.4) | 0 | |||
| Right | 0 | 2 (28.6) | 0 | 0 | 0 | 1 (50) | 0 | 0 | |||
| No | 10 (83.3) | 5 (71.4) | 2 (100) | 18 (100) | 1 (100) | 1 (50) | 11 (84.6) | 18 | |||
| Shoulder pain | 0.472 | 0.152 | |||||||||
| Yes | 2 (16.7) | 2 (28.6) | 1 (50) | 2 (11.1) | 0 | 1 (50) | 3 (23.1) | 1 (100) | |||
| No | 10 (83.3) | 5 (71.4) | 1 (50) | 16 (88.9) | 1 (100) | 1 (50) | 13 (76.9) | 0 | |||
| Hand | 0.001 | 0.898 | |||||||||
| Left | 0 | 0 | 1 (50) | 0 | 0 | 0 | 1 (7.7) | 0 | |||
| Right | 0 | 1 (14.2) | 0 | 1 (5.55) | 0 | 1 (50) | 1 (7.7) | 0 | |||
| Both | 0 | 0 | 0 | 5 (27.7) | 0 | 0 | 2 (15.4) | 0 | |||
| No | 12 (100) | 6 (85.7) | 1 (50) | 12 (66.6) | 1 (100) | 1 (50) | 9 (69.2) | 1 (100) | |||
| Neck pain | 0.029 | 0.258 | |||||||||
| Yes | 3 (25) | 3 (42.9 ) | 0 (0) | 8 (66) | 0 (0) | 2 (100) | 6 (46.2) | 1 (100) | |||
| No | 9 (75) | 4 (57.1) | 2 (100) | 4 (44) | 1 (100) | 0 (0) | 7 (53.8) | 0 | |||
| Lower back pain | 0.003 | 0.3 | |||||||||
| Yes | 2 (16.7) | 1 (14.3) | 2 (100) | 6 (54.5) | 0 (0) | 0 (0) | 6 (46.2) | 1 (100) | |||
| No | 10 (83.3) | 6 (85.7) | 0 | 5 (45.5) | 1 (100) | 2 (100) | 7 (53.8) | 0 | |||
| Elbow pain | 0.468 | 0.99 | |||||||||
| Yes | 1 (8.3) | 1 (14.3) | 0 | 0 | 0 (0) | 0 (0) | 3 (23.1) | 0 | |||
| No | 11 (91.7) | 6 (85.7) | 2 (100) | 18 (100) | 1 (100) | 2 (100) | 10 (76.9) | 1 | |||
| Hand numbness | 0.75 | 0.489 | |||||||||
| Left | 1 (8.3) | 0 | 0 (0) | 1 (5.6) | 0 (0) | 1 (50) | 2 (15.4) | 0 | |||
| Right | 11 (91.7) | 7 | 2 (100) | 17 (94.4) | 1 (100) | 1 (50) | 11 (84.6) | 1 | |||
| Both | |||||||||||
| No | |||||||||||
| Carpal tunnel | 0.007 | 0.874 | |||||||||
| Yes | 0 | 0 | 0 | 2 (22) | 0 (0) | 0 | 2 (15.4) | 0 | |||
| No | 12 | 7 | 2 | 7 (78) | 1 (100) | 2 | 11 (84.6) | 1 | |||
Of all the total respondents only 33.3% of those having pain attributed it to endoscopy while, 52.4% were not certain whether the symptoms had been caused by endoscopy and 14.3% said that symptoms were not caused by endoscopy.
Thirty-two point one percent of respondents indicated evident pain during endoscopy, with 33.3% of those were bothered by this symptom.
Thirty point five percent of the participants indicated that the duration of their symptoms was more than 6 mo, and of those, 57.1% indicated that their symptoms were static and 10.7% indicated they were increasing. Around 21.4% of respondents had to take time off from work and 33.9% took medications for resolution of pain.
The responders were asked if they used some modifications to prevent these injuries (Supplementary Material 1). Specific modifications that were assessed were placing the endoscopic monitor at eye level (21.4%) or cardiac monitor in front (12.5%), stopping the procedure to move patients (8.9%), sitting while performing a colonoscopy (12.5%), and using height-adjustable patient beds (23.2%).
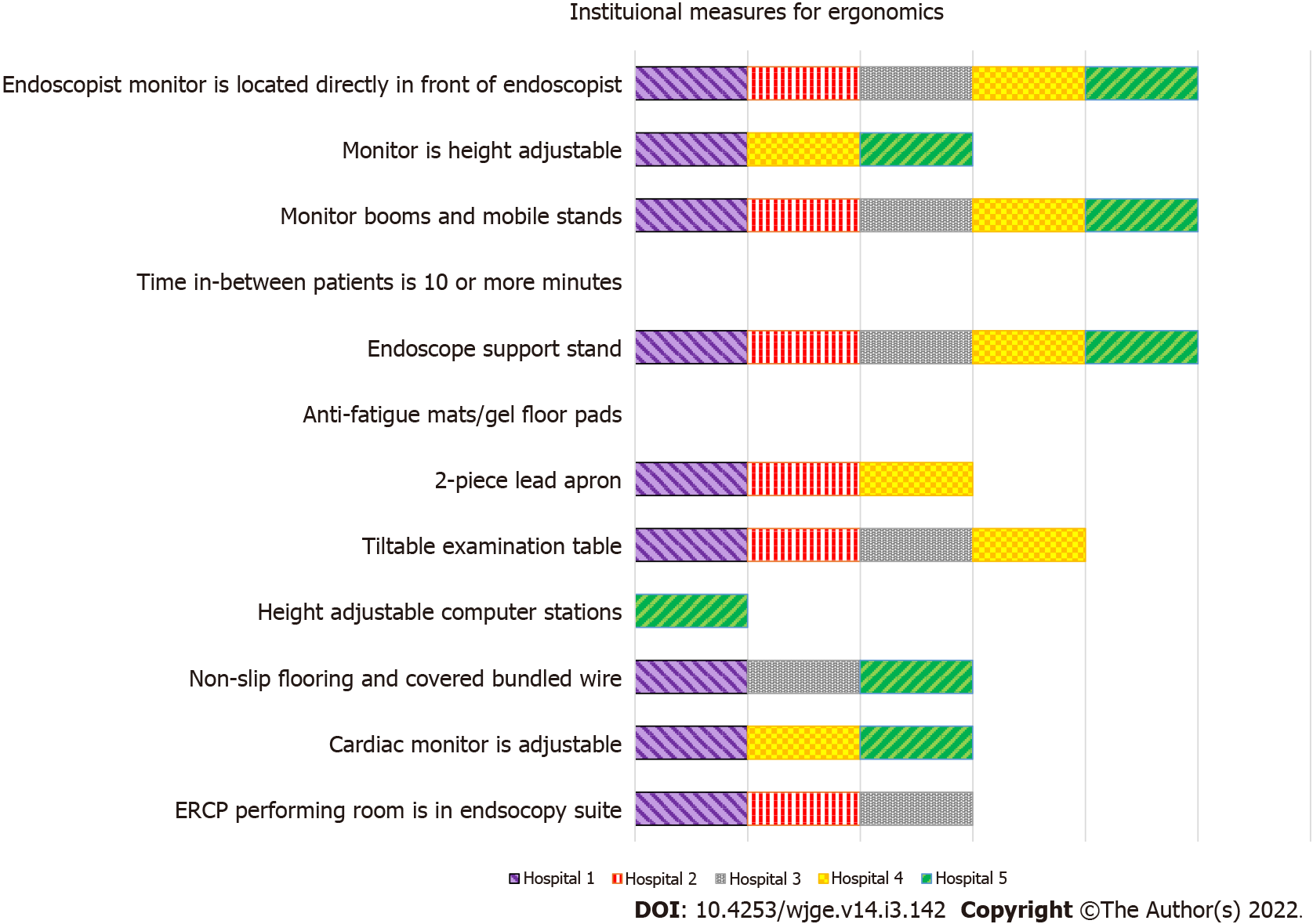
All 5 tertiary care institutions ensured that the endoscopist monitor was located directly in front of the endoscopist and monitor boom, mobile stands, and endoscope support stands were available (Figure 2). All 5 hospitals also ensured that the patient examination table was height adjustable. Four out of the 5 hospitals had a tiltable examination table. Three out of 5 tertiary setups had adjustable monitor height, adjustable cardiac monitor, 2-piece lead aprons, non-slip flooring, and covered bundled wires. Three of 5 hospitals also had an ERCP room in the endoscopy suite.
One hospital provided an adjustable computer station and none of the institutions provided anti-fatigue mats/gel floor pads or had a time-out session of 10 min or more in between two consecutive endoscopy patients.
In this study, we tried to shed light on challenges affecting MSI in endoscopists and their ancillary staff. Numerous studies have identified procedure volume and number of years in practice to be a risk factors for injury[10]. In this study, we documenting the prevalence of such injuries, the awareness and practice of ergonomic intervention by current endoscopists and the ancillary staff, as well as the availability and use of ergonomic facilities in our tertiary care institutions.
Workplace injury has undoubtedly put an additional strain on the already chronic shortage of specialists. It can harm the productivity of healthcare workers and cause long-term pain and disability.
The overall prevalence of pain or has been reported among reporting endoscopists to be as high as 29% to 89% in numerous literature[1,5,11,12]. Our study confirmed these results, with our respondents acknowledging the prevalence of such pain and injury in 75% of our subjects, similar to Hansel et al[5] at 74%. In the largest survey done, examining endoscopy-related MSI, which targeted members of the American Society for Gastrointestinal Endoscopy (ASGE), 53% of endoscopists had reported injuries[13]. Similarly, in a study involving 190 endoscopists in Japan, 43% reported musculoskeletal pain[14].
The site of injury plays an important role in the hindrance of an endoscopist’s work. The three most commonly affected anatomical regions in our series were the neck, lower back, and shoulders, at 41.1%, 32.1%, and 21.4%, respectively. These numbers were partially contradictory to most articles we found, such as Han et al[15] quoting shoulders and back at approximately 42% and 38%, respectively, and Villa et al[3] signifying the right wrist and left thumb being the most affected at 53% and 48%, respectively.
Although literature such as Villa et al[3] reported almost half of their subjects, 47%, acknowledging pain related to that of endoscopies, our study reflected one-third (33.3%) of our respondents attributing their symptoms due to such procedures. This could be identified as a lack of awareness or as a reluctance to practice ergonomic activities in the endoscopy suites.
Although three-quarters of our respondents acknowledging the presence of pain, surprisingly, 52.4% stated that they could not be certain whether endoscopy was a cause of their symptoms, and 14.3% said their symptoms were not caused by performing these procedures.
Some of the most important factors are repetitive movements, overuse of muscles, and prolonged standing, all of which are important parts of conducting an endoscopy. Some studies even go as far as quoting more than 16 h or 20 cases per week can lead to an increase in the risk of MSI[10,12]. Although factors leading to these injuries were not directly studied in our numbers, previous literature shed some light as stated above.
Arguably, gender does play a role according to a study conducted in ASGE fellows, which reported female gender as the only significant risk factor for MSI based on factors pertaining to their hand size and grip strength[13]. However, in our study, with only 30.3% females, a relative comparison showed no gender-related difference in MSI (Table 3).
Most literature on the prevalence of endoscopic MSI did not evaluate the impact of regular activity and work. Alarmingly, we noted 21.4% of our respondents had to take time off from work due to endoscopy-related pain. This number was an increase from other literature we found and can be subjectively linked to limited specialists and ancillary staff in this field in the city and long working hours this entails[2,5]. Morais et al[2] recently conducted a study amongst Portuguese endoscopists, and found that 10.1% of their respondents took time off on account of endoscopy-related injuries, with a median of 30 d. This number contrasts with previous literature in which only a few endoscopists reported missing work and only for a few days[5].
In regards to our study, this significant loss of productivity needs to be properly addressed. This will ensure avoidable time off and lead to a decreased load on fellow endoscopists and ancillary staff.
Our study further investigated what measures are being taken by the endoscopists at an institutional level to decrease MSI. For example, the availability and use of portable and/or flexible endoscopy and cardiac/vital monitors can play a vital role in preventing injuries[8].
Documentation of injuries is the first step in improving and promoting discussion on workplace ergonomics as indicated in a national survey by Austin et al[13], where gastroenterology trainees and program directors were approached pre- and post- ergonomic training, and 90% of participants reportedly agreed that the ergonomic training sessions had a positive impact. These trainings eventually led to a decrease in the number of injuries and the creation a more ergonomic friendly work environment for endoscopists. Such practices are uncommon in our institutions.
Multiple factors were questioned in our survey that we compiled based on the current literature search and the proven adjustments and maneuvers that played a role in ergonomics[8]. Out of the total, 23.2% adjusted the height-adjustable-bed, 12.5% placed a cardiac monitor in front, 8.9% stopped to move patients, and 8.9% sat while performing the procedure. Such low numbers speak volumes on the limited awareness of ergonomics, despite the availability of these possibilities, and also shed light on why ergonomic sessions must be undertaken in the initial training months of endoscopy. Regional pain as described above could all be caused due to poor posture. Lack of posture and ergonomic timeouts play a vital role in such context. Effective strategies to ensure good posture can significantly improve endoscopists’ pain.
To avoid improper positioning, endoscopy units should consider having an “ergonomic timeout” before starting a procedure to ensure proper bed height, patient position, and monitor location[3,11]. There is a clear role for widespread education and the implementation of guidelines for the best clinical practice of ergonomics[6,7,11,16]. It is easy to see the need for more training to ensure a higher percentage of respondents take preventive measures to improve their quality of life.
To elucidate this aspect, our 13-point checklist was studied at five tertiary care hospitals, where we examined the accessibility to basic endoscopy suite ergonomic capabilities in the devices used for every endoscopic procedure. Out of the five hospitals, none of them had a time out of ten mins or more between two patients, which could lead to patient identification errors and would give insufficient time for the endoscopist to complete individualized patient reports. A 10-min time-out would also support decreased muscle fatigue levels.
Height-adjustable examination beds, endoscopy support stand, monitor booms, and having the accessibility of the main endoscopic camera screen in front were available in all five tertiary care facilities.
None of the hospitals had any form of anti-fatigue mats or gel floor pads, however, three of them did have anti-slip flooring with wires being covered for protection against tripping over. Three of the hospitals also had movable cardiac/vital monitors alongside height-adjustable monitors for the endoscopist. One of the tertiary care hospitals had an adjustable computer station, while three of the hospitals had the ERCP procedure room within the reaches of the endoscopic procedure room.
Our respondents were limited to 56 participants. For ergonomic evaluations, only five units in a geographic area limit the generalizability of the findings. An analysis of the pre- and post- ergonomic training with quantitative and qualitative analysis on our subjects would have added to the reliability of our findings.
This is the first study to be conducted in Pakistan for injuries caused by endoscopy. Our endoscopists had a significant prevalence of MSI leading to hindrance in their day-to-day activities and professional continuity.
Lack of knowledge and awareness of such injuries, both at a personal and institutional level, need to be addressed. Multiple areas need to be addressed in a strategic approach. We must increase awareness of these injuries among endoscopists and staff and standardized curricula to educate fellows on ergonomic practices to reduce the early development of overuse injuries. Institutions should also have standardized ergonomic protocols in place in endoscopy suites.
More research is needed to document the efficacy of an intervention in improving quality of life and productivity.
Ergonomics in the field of gastroenterology with regards to musculoskeletal injuries (MSI) among endoscopists and ancillary staff have been highlighted in studies from the western world. MSI affect the quality and longevity of the gastroenterologist, which can lead to a shortage of specialists. There has been a dearth of literature on the topic from our region.
The goal of this research was to create awareness about the importance of ergonomics in endoscopy that may prevent future injuries. Research would lead towards the modification and development of more ergonomic endoscopes and techniques. Furthermore, procedure rooms and spaces with institutional emphasis would promote strategies for the management of musculoskeletal injury.
Our objective is to document the prevalence of MSI, awareness, and practice of ergonomics by endoscopists, ancillary staff, and institutions.
An observational cross-sectional study in Karachi. An eleven-point self-administered questionnaire was distributed and used to evaluate MSI and ergonomic adjustments amongst three tertiary care setups in Karachi. An onsite survey via a 13-point checklist for endoscopy suite facilities was used to assess the ergonomically friendly conveniences at five tertiary care setups.
There were 56 participants in total with 39 (69.6%) males. Pain and numbness were documented by 75% of the respondents, with the neck (41.1%) and lower back (32.1%) being the most commonly affected regions. Twenty one point four percent had to take time off their work, while 33.9% took medications for pain. Ergonomic modifications to prevent musculoskeletal injury were used by 21.4%. Institutions lacked sufficient ergonomic facilities.
Three-fourth of our endoscopists reported MSI, of which more than half are not sure or attributed this problem to endoscopy. The prevalence of MSI warrants urgent attention.
It would be interesting to see interventions to improve the ergonomics among participants, such as pre- and post-intervention improvement and the impact of creating awareness. Research can be directed towards the development of curriculum and guidelines addressing ergonomics and modifications to prevent MSI.
We thank all the respondents for taking out their time to fill in our questionnaire and also thank the following five hospitals for allowing us to examine their endoscopy suites: Aga Khan University Hospital, Liaquat National Hospital, Ziauddin University Hospital, Dr. Ruth K. M. Pfau Civil Hospital and Sindh Institute of Urology and Transplant.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Pakistan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arslan M, Costache RS, Mestrovic A, Patel D S-Editor: Gao CC L-Editor: Filipodia P-Editor: Gao CC
| 1. | Harvin G. Review of musculoskeletal injuries and prevention in the endoscopy practitioner. J Clin Gastroenterol. 2014;48:590-594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 2. | Morais R, Vilas-Boas F, Pereira P, Lopes P, Simões C, Dantas E, Cunha I, Roseira J, Cortez-Pinto J, Silva J, Lage J, Caine M, Rocha M, Flor de Lima M, Costa Santos MP, Garrido M, Sousa P, Marcos P, Azevedo R, Castro R, Cúrdia Gonçalves T, Leal T, Magno-Pereira V, Ramalho R, Rodrigues-Pinto E, Macedo G. Prevalence, risk factors and global impact of musculoskeletal injuries among endoscopists: a nationwide European study. Endosc Int Open. 2020;8:E470-E480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Villa E, Attar B, Trick W, Kotwal V. Endoscopy-related musculoskeletal injuries in gastroenterology fellows. Endosc Int Open. 2019;7:E808-E812. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 4. | Ofori E, Ramai D, John F, Reddy M, Ghevariya V. Occupation-associated health hazards for the gastroenterologist/endoscopist. Ann Gastroenterol. 2018;31:448-455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Hansel SL, Crowell MD, Pardi DS, Bouras EP, DiBaise JK. Prevalence and impact of musculoskeletal injury among endoscopists: a controlled pilot study. J Clin Gastroenterol. 2009;43:399-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Chang MA, Mitchell J, Abbas Fehmi SM. Optimizing ergonomics during endoscopy. VideoGIE. 2017;2:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Chang MA, Mitchell J, Abbas Fehmi SM. Optimizing ergonomics before endoscopy. VideoGIE. 2017;2:169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | ASGE Technology Committee; Pedrosa MC, Farraye FA, Shergill AK, Banerjee S, Desilets D, Diehl DL, Kaul V, Kwon RS, Mamula P, Rodriguez SA, Varadarajulu S, Song LM, Tierney WM. Minimizing occupational hazards in endoscopy: personal protective equipment, radiation safety, and ergonomics. Gastrointest Endosc. 2010;72:227-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Tanaka S, Raju GS. Part II: Optimizing endoscopy unit design: Lessons from a modern endoscopy suite in Japan. Tech Gastrointest Endosc. 2019;21:140-142. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Ridtitid W, Coté GA, Leung W, Buschbacher R, Lynch S, Fogel EL, Watkins JL, Lehman GA, Sherman S, McHenry L. Prevalence and risk factors for musculoskeletal injuries related to endoscopy. Gastrointest Endosc. 2015;81:294-302.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 70] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 11. | Shergill AK, McQuaid KR. Ergonomic endoscopy: An oxymoron or realistic goal? Gastrointest Endosc. 2019;90:966-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 12. | Singla M, Kwok RM, Deriban G, Young PE. Training the Endo-Athlete: An Update in Ergonomics in Endoscopy. Clin Gastroenterol Hepatol. 2018;16:1003-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Austin K, Schoenberger H, Sesto M, Gaumnitz E, Teo Broman A, Saha S. Musculoskeletal Injuries Are Commonly Reported Among Gastroenterology Trainees: Results of a National Survey. Dig Dis Sci. 2019;64:1439-1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Kuwabara T, Urabe Y, Hiyama T, Tanaka S, Shimomura T, Oko S, Yoshihara M, Chayama K. Prevalence and impact of musculoskeletal pain in Japanese gastrointestinal endoscopists: a controlled study. World J Gastroenterol. 2011;17:1488-1493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Han S, Hammad HT, Wagh MS. High prevalence of musculoskeletal symptoms and injuries in third space endoscopists: an international multicenter survey. Endosc Int Open. 2020;8:E1481-E1486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Edelman KM, Zheng J, Erdmann A, Garrett M, McGreal N, Moore J, Saha S, Zimmermann EM, Borum ML, Toriz BE, Provenzale D, Chow S-C, Corey KE, Cruz-Correa MR, Shafi M, Garman KS. Endoscopy-Related Musculoskeletal Injury in AGA Gastroenterologists is Common while Training in Ergonomics is Rare. Gastroenterology. 2017;152:S217. [DOI] [Full Text] |