Published online Mar 16, 2021. doi: 10.4253/wjge.v13.i3.90
Peer-review started: November 4, 2020
First decision: December 18, 2020
Revised: January 1, 2021
Accepted: January 28, 2021
Article in press: January 28, 2021
Published online: March 16, 2021
Processing time: 125 Days and 0.7 Hours
Blue rubber bleb nevus syndrome (BRBNS) is a rare vascular disease, difficult to diagnose and choose a treatment method, especially in young children. There are several limiting factors to the use of enteroscopy for diagnostics and treatment in pediatric patients, in general. The literature on BRBNS cases is limited and presents various therapeutic approaches.
We present here a case of BRBNS involving a 4-year-old female, whose intestinal venous lesions were successfully treated by endoscopic sclerotherapy and aethoxysklerol foam. Skin lesions, typical for BRBNS, appeared on the 8th d of the child’s life and their number increased over the next several months. The child also experienced episodes of critical decrease in hemoglobin level (by as much as 52 g/L) for several years, requiring iron supplementation and several blood transfusions. Video capsule endoscopy revealed numerous vascular formations in the small bowel. The combined findings of gastrointestinal venous formations and skin lesions prompted BRBNS diagnosis. Single-balloon enteroscopy was used to perform sclerotherapy, with aethoxysklerol foam. A positive effect was observed within 19 mo of follow-up. We continue to monitor the patient’s hemoglobin level, every 2 wk, and it has remained satisfactory (> 120 g/L).
Endoscopic sclerotherapy can be effective in the clinical management of gastrointestinal manifestations of BRBNS in young children.
Core Tip: In blue rubber bleb nevus syndrome (BRBNS), vascular malformations can affect any organ in the body but skin and gastrointestinal tract are the most frequent. Skin venous malformations have been observed in patients with BRBNS since childhood, with number and size of lesions increasing through time. Gastrointestinal lesions also occur at an early age and provoke gastrointestinal bleeding, leading to anemia. Treatment of the clinical manifestations of BRBNS can be carried out by endoscopic, pharmacological or surgical approaches. We present here a BRBNS case in a young child, treated by sclerotherapy with aethoxysklerol foam applied during single-balloon enteroscopy.
- Citation: Marakhouski K, Sharafanovich E, Kolbik U, Sautin A, Nikalayeva K, Pataleta A, Sanfirau K, Svirsky A. Endoscopic treatment of blue rubber bleb nevus syndrome in a 4-year-old girl with long-term follow-up: A case report. World J Gastrointest Endosc 2021; 13(3): 90-96
- URL: https://www.wjgnet.com/1948-5190/full/v13/i3/90.htm
- DOI: https://dx.doi.org/10.4253/wjge.v13.i3.90
Blue rubber bleb nevus syndrome (BRBNS), or bean syndrome, is a rare congenital vascular disease, eliciting predominant damage of the skin and digestive tract[1,2] . The clinical spectrum of BRBNS is very heterogeneous, with various phenotypic patterns. Patients may experience single lesions of the skin and gastrointestinal (GI) tract or multiple lesions affecting the skin, GI tract, and other organs[3-5].
The pathogenesis of BRBNS has not been studied extensively. There is an assumption of autosomal dominant inheritance, based upon a change in the 9p chromosome locus and observations of this syndrome among blood relatives[6,7]; although, most cases appear to be sporadic[3,8].
Cutaneous venous formations are observed in 78% of patients and vascular lesions of the GI tract in 89%[9,10]. While BRBNS-related venous malformations can occur throughout the GI tract, they most often involve the small bowel (100%), followed by the colon (74%) and the stomach (26%); they vary in shape and number, ranging from a few to several hundred lesions[8,11] . The development of BRBNS is associated with GI bleeding, and normally the lesions grow in number and size over the lifetime of an afflicted individual[12]. The skin lesions rarely cause serious clinical problems-in contrast to the GI vascular malformations, which can cause acute or chronic bleeding and subsequent anemia, and in some cases fatality[13,14].
We present, herein, a case of BRBNS in a 4-year-old female with skin and GI manifestations.
A 4-year-old female was hospitalized in the Republican Center of Pediatric Surgery (Minsk, Belarus) in 2017 with the signs of chronic GI bleeding, iron deficiency anemia, episodes of melena, and a rapid deterioration in her general condition.
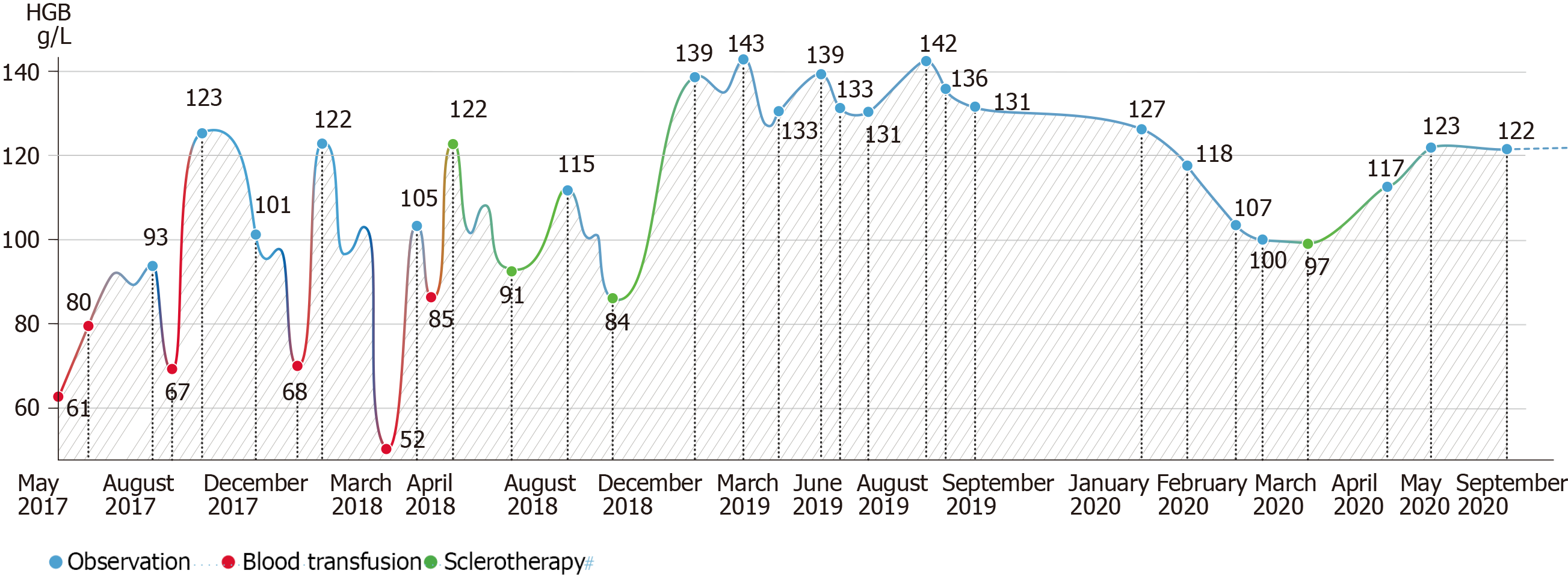
During the first year of observation in our clinic, the child underwent seven procedures of blood transfusions due to low hemoglobin levels before the first sclerotherapy was performed.
The patient’s birth (per via naturalis) had resulted from the mother’s first pregnancy, which was also full-term. Her birth weight was 3760 g and length was 51 cm. The patient’s mother noticed a roundish dark blue, soft-elastic formation on the skin of the child’s thigh at 8 d after the birth. A few months later, new formations appeared on the skin of the child’s head (at the border of the forehead and parietal ridge) and lumbar, perianal and plantar areas.
Anamnesis vitae yielded report of venous malformations involving the gluteo-femoral region, which had been partly excised at the age of 3 mo. Several complaints of melena were also disclosed. In addition, the parents reported that, at the age of 2 years, the child had developed periodic lethargy, drowsiness, and pallor of the skin; clinical assessment at that time yielded the first detection of a significant decrease in hemoglobin levels. Thus, iron supplements were prescribed. Several other episodes of a critical decrease in hemoglobin reportedly occurred over the next few years, all of which required a blood transfusion.
The patient has no family history of BRBNS.
The patient’s skin showed an overall paleness and several vascular skin lesions were found in the lumbar region, the inner part of the left thigh, the lower leg, the forearm (Figure 1), and on the sole of the right foot. The formations were of various sizes but all had a soft, elastic-like consistency and showed a cyanotic coloration.
The patient’s blood parameters were low, with hemoglobin of 95 g/L (normal range: 110-140 g/L), mean corpuscular hemoglobin concentration of 32.8 (normal range: 31.9-35.6 g/dL), erythrocytes of 4.4 × 1012/L (normal range: 3.9-5.3 × 1012/L), and hematocrit of 29% (normal range: 34%-40%).
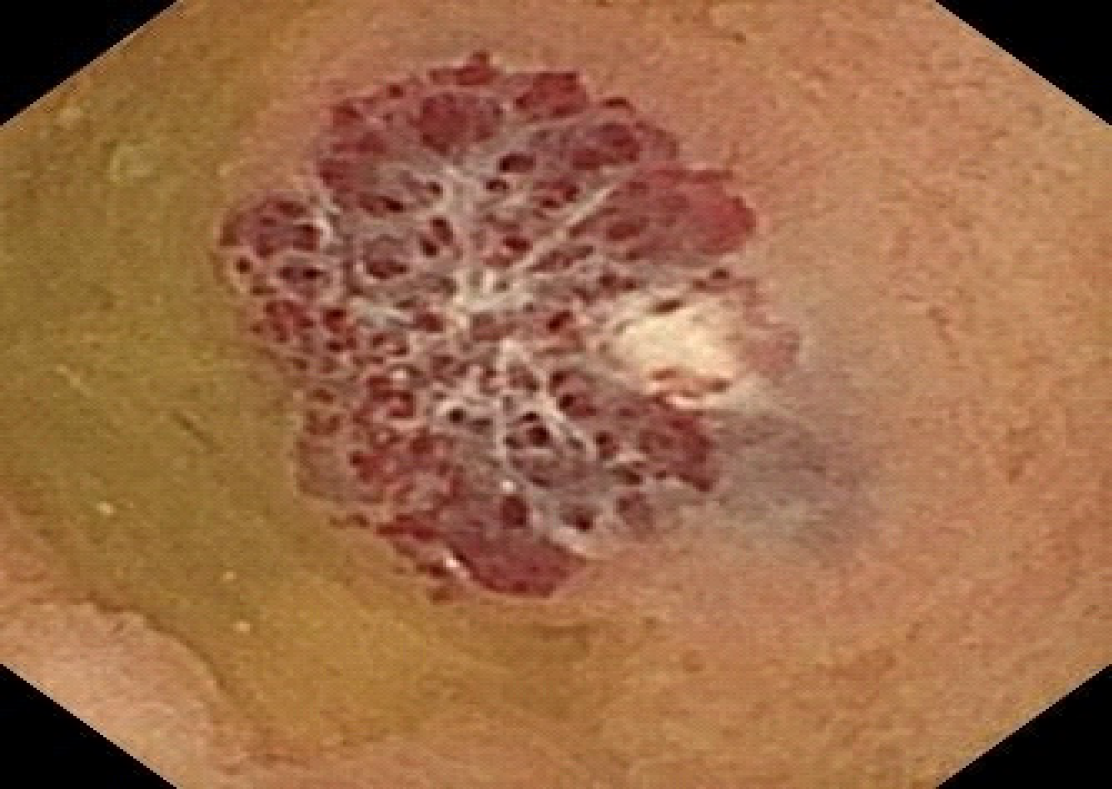
Ultrasound showed vascular malformations in the left lobe of the liver, pancreas, bladder, and left ovary. Magnetic resonance imaging of the soft tissues of the lower extremities showed vascular malformations in the upper third of the left thigh. Although gastroscopy and colonoscopy were unsuccessful in detecting the source of GI bleeding, capsule enteroscopy revealed multiple (-10) vascular formations in the wall of the small intestine (Figure 2). All formations appeared round in shape and bluish-purple in color; the largest reached 2 cm in diameter.
BRBNS with secondary severe iron deficiency anemia.
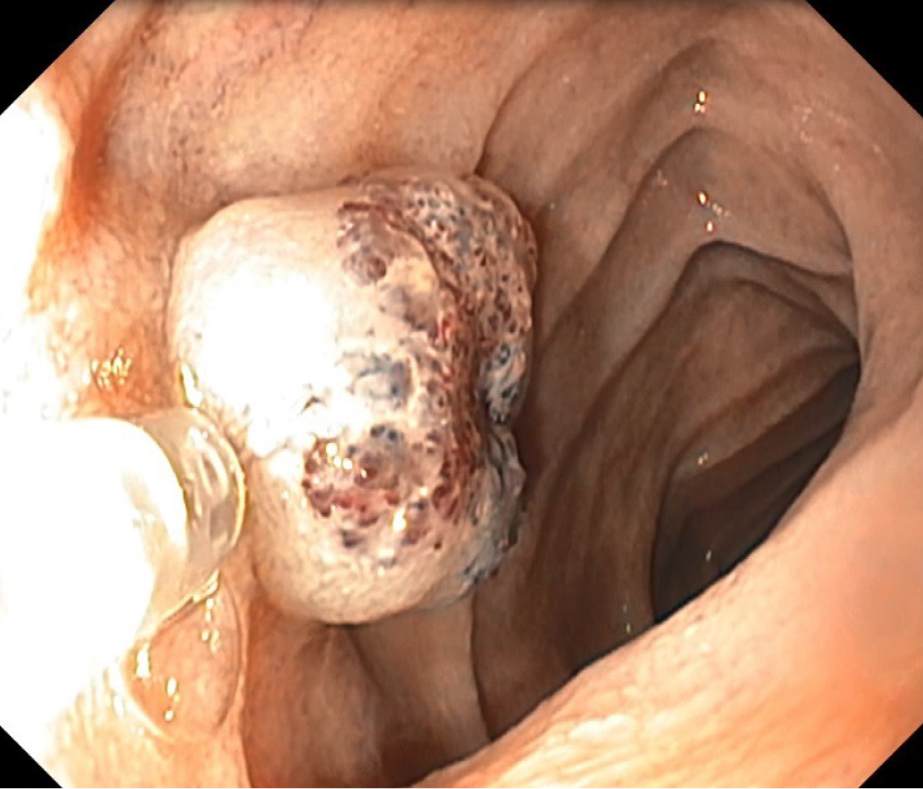
Sclerotherapy was ordered via single-balloon enteroscopy (Figure 3). During the first attempt at antegrade enteroscopy, it became clear that a total examination of the small bowel would be technically impossible. Therefore, subsequent enteroscopies were carried out with sequential antegrade and retrograde access guided by a tattoo of the maximum antegrade passage area of the enteroscope and simultaneous sclerotherapy. From December 2017 to March 2020, five total single-balloon enteroscopies were performed (Table 1). During each, foam sclerotherapy was carried out using 10 mL of a 1% aethoxysklerol solution, targeting all of the vascular malformations that had been identified. The sclerotherapy procedure itself was performed according to the Tessari method[15], in which a 1:4 mixture of the sclerosing agent and air [2 mL of 1% aethoxysklerol (10 mg/mL) mixed with 8 mL of air] was pumped in via two syringes connected by a 3-way adapter with a tap.
| December 20, 2017 | March 23, 2018 | May 22, 2018 | August 31, 2018 | March 30, 2020 | |
| Enteroscopy | |||||
| Antegrade | + | + | + | + | + |
| Retrograde | - | + | + | + | + |
| Sclerotherapy | + | + | + | + | + |
| Malformations | |||||
| Stomach | - | + | + (sclerotherapy) | No new ones | Not visualized |
| Small bowel | + | + | + | + | + |
| Large bowel | - | - | - | - | + |
The total follow-up duration was 33 mo (from December 2017 to September 2020). The first period of remission lasted 15 mo (from October 2018, upon the first detection of hemoglobin > 120 g/L, to January 2020). In February 2020, the patient’s hemoglobin level began to fall, reaching a low of 97 g/L in March 2020. At the end of March 2020, single-balloon enteroscopy was reperformed. New vascular malformations were detected in the small bowel and, for the first time, in the colon, and these were considered as the likely cause of the hemoglobin decline. The sequential sclerotherapy was followed by a return of the hemoglobin level to the previous value of 120 g/L in early May 2020. The 2-wk interval follow-ups have shown the level to remain at > 120 g/L since then (Figure 4). It’s worth noting that the child has not received iron supplement therapy since November 2018.
Treatment of BRBNS is usually based upon the patient’s symptomatic profile and depending on degree of GI damage and/or involvement of other organs in the pathological process[10,16]. Choosing the optimal therapy for the manifestation of BRBNS with GI bleeding is a rather difficult task, especially when it comes to a 4-year-old patient. On the one hand, balloon-assisted enteroscopy-while being the gold standard for the diagnosis and treatment of bowel malformations in adult patients with BRBNS-is a relatively unsafe method in young children[17]. Limiting factors in any case are age and weight, especially so for children. Thus, we turned to the literature on pediatric cases of BRBNS.
Chen et al[18] reported on the successful performance of two-balloon enteroscopy in 72 pediatric patients, the youngest of whom was 6 years of age. In addition, Isoldi et al[10] reported on 18 clinical cases of BRBNS in children; all 4 who underwent balloon-assisted enteroscopy experienced a positive effect that lasted for 4-16 mo. We also chose to treat our patient’s illness with balloon-assisted (single) enteroscopies, and the beneficial clinical effect on hemoglobin endured over a total of 19 mo [from October 2018 to September 2020, excepting the 3 mo (February-April 2020) before the last treatment].
Different kinds of GI malformations in BRBNS can be addressed by surgical treatment; although, this approach is rather aggressive, carries risk of postoperative complications, and is probably better justified for patients with few GI malformations located in a limited span of the bowel. There is also the risk of re-manifestation after resection[19], even for the combination method of endoscopic electrocoagulation and surgical removal[20]. The endoscopic interventions themselves, including argon plasma coagulation, electrocautery and histoacryl injection, also carry risk of perforation and rebleeding[11,21]. In our case, the venous malformations detected during enteroscopy numbered more than 15 and were located along the entire length of the hollow organs of the GI tract. This situation would have required particularly extensive laparoscopic/open resection, posing too great overall risk to the young child. Moreover, the child’s young age presented the risk of new lesions forming on the wall of the intestine during the subsequent years of life, adding further reason against the laparoscopic/open resection approach[8] . Endoscopic sclerotherapy was suggested as a less aggressive and less invasive option.
Two studies[15,22] in the literature have suggested systemic medical therapy with sirolimus as highly effective for pediatric patients. Unfortunately, two other studies[23,24] confounded the potential benefit by reporting on substantial negative side effects.
The applied method of endoscopic treatment showed its effectiveness in regard to rescue of hemoglobin level for 19 mo, during a 3-year follow-up period. New, clinically significant malformations appeared in the patient’s small bowel only at 16 mo after the first application of endoscopic sclerotherapy. In the Republic of Belarus, the patient described herein is, to date, the smallest patient by age and weight to undergo total single-balloon enteroscopy. There were no side effects related to the procedure in our case. Thus, endoscopic sclerotherapy with aethoxysklerol foam can be an appropriate option for BRNBS treatment, even in young children.
Manuscript source: Unsolicited manuscript
Specialty type: Pediatrics
Country/Territory of origin: Belarus
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Isoldi S S-Editor: Zhang H L-Editor: A P-Editor: Wang LL
| 1. | Nakajima H, Nouso H, Urushihara N, Fukumoto K, Yamoto M, Miyake H, Sekioka A, Nomura A, Yamada Y. Blue Rubber Bleb Nevus Syndrome with Long-Term Follow-Up: A Case Report and Review of the Literature. Case Rep Gastrointest Med. 2018;2018:8087659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | McKinlay JR, Kaiser J, Barrett TL, Graham B. Blue rubber bleb nevus syndrome. Cutis. 1998;62:97-98. [PubMed] |
| 3. | Jin XL, Wang ZH, Xiao XB, Huang LS, Zhao XY. Blue rubber bleb nevus syndrome: a case report and literature review. World J Gastroenterol. 2014;20:17254-17259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 80] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Dobru D, Seuchea N, Dorin M, Careianu V. Blue rubber bleb nevus syndrome: case report and literature review. Rom J Gastroenterol. 2004;13:237-240. [PubMed] |
| 5. | Ertem D, Acar Y, Kotiloglu E, Yucelten D, Pehlivanoglu E. Blue rubber bleb nevus syndrome. Pediatrics. 2001;107:418-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Menegozzo CAM, Novo FDCF, Mori ND, Bernini CO, Utiyama EM. Postoperative disseminated intravascular coagulation in a pregnant patient with Blue Rubber Bleb Nevus Syndrome presenting with acute intestinal obstruction: Case report and literature review. Int J Surg Case Rep. 2017;39:235-238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Kisu T, Yamaoka K, Uchida Y, Mori H, Nakama T, Hisatsugu T, Miyaji H, Motooka M. A case of blue rubber bleb nevus syndrome with familial onset. Gastroenterol Jpn. 1986;21:262-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Dòmini M, Aquino A, Fakhro A, Tursini S, Marino N, Di Matteo S, Lelli Chiesa P. Blue rubber bleb nevus syndrome and gastrointestinal haemorrhage: which treatment? Eur J Pediatr Surg. 2002;12:129-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Boente MD, Cordisco MR, Frontini MD, Asial RA. Blue rubber bleb nevus (Bean syndrome): evolution of four cases and clinical response to pharmacologic agents. Pediatr Dermatol. 1999;16:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Isoldi S, Belsha D, Yeop I, Uc A, Zevit N, Mamula P, Loizides AM, Tabbers M, Cameron D, Day AS, Abu-El-Haija M, Chongsrisawat V, Briars G, Lindley KJ, Koeglmeier J, Shah N, Harper J, Syed SB, Thomson M. Diagnosis and management of children with Blue Rubber Bleb Nevus Syndrome: A multi-center case series. Dig Liver Dis. 2019;51:1537-1546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Choi KK, Kim JY, Kim MJ, Park H, Choi DW, Choi SH, Heo JS. Radical resection of intestinal blue rubber bleb nevus syndrome. J Korean Surg Soc. 2012;83:316-320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Adeniji AA, Fairlie FM, Jones TH, Wilkinson P. Pregnancy and blue rubber bleb naevus syndrome. Br J Obstet Gynaecol. 1999;106:1316-1318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Ning S, Zhang Y, Zu Z, Mao X, Mao G. Enteroscopic sclerotherapy in blue rubber bleb nevus syndrome. Pak J Med Sci. 2015;31:226-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Chen PP, Weishaar PD, Murray TG. Blue rubber bleb nevus syndrome. J Pediatr Ophthalmol Strabismus. 1997;34:321-323. [PubMed] |
| 15. | Tessari L, Cavezzi A, Frullini A. Preliminary experience with a new sclerosing foam in the treatment of varicose veins. Dermatol Surg. 2001;27:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Rešić A, Močić Pavić A, Čizmić A, Potočnjak I. Images in Vascular Medicine: Blue rubber bleb nevus syndrome: A rare cause of gastrointestinal bleeding and vascular anomaly in children. Vasc Med. 2018;23:82-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Agnese M, Cipolletta L, Bianco MA, Quitadamo P, Miele E, Staiano A. Blue rubber bleb nevus syndrome. Acta Paediatr. 2010;99:632-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Chen H, Liu Y, Fu L, Lin X, Fan D, Li C. Clinical utility of double-balloon enteroscopy in children: A single-centre experience in South China. J Paediatr Child Health. 2019;55:188-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Gonzalez D, Elizondo BJ, Haslag S, Buchanan G, Burdick JS, Guzzetta PC, Hicks BA, Andersen JM. Chronic subcutaneous octreotide decreases gastrointestinal blood loss in blue rubber-bleb nevus syndrome. J Pediatr Gastroenterol Nutr. 2001;33:183-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Kopácová M, Tachecí I, Koudelka J, Králová M, Rejchrt S, Bures J. A new approach to blue rubber bleb nevus syndrome: the role of capsule endoscopy and intra-operative enteroscopy. Pediatr Surg Int. 2007;23:693-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Ng WT, Kong CK. Argon plasma coagulation for blue rubber bleb nevus syndrome in a female infant. Eur J Pediatr Surg. 2003;13:137-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Ogu UO, Abusin G, Abu-Arja RF, Staber JM. Successful Management of Blue Rubber Bleb Nevus Syndrome (BRBNS) with Sirolimus. Case Rep Pediatr. 2018;2018:7654278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Yuksekkaya H, Ozbek O, Keser M, Toy H. Blue rubber bleb nevus syndrome: successful treatment with sirolimus. Pediatrics. 2012;129:e1080-e1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 24. | Salloum R, Fox CE, Alvarez-Allende CR, Hammill AM, Dasgupta R, Dickie BH, Mobberley-Schuman P, Wentzel MS, Chute C, Kaul A, Patel M, Merrow AC, Gupta A, Whitworth JR, Adams DM. Response of Blue Rubber Bleb Nevus Syndrome to Sirolimus Treatment. Pediatr Blood Cancer. 2016;63:1911-1914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |